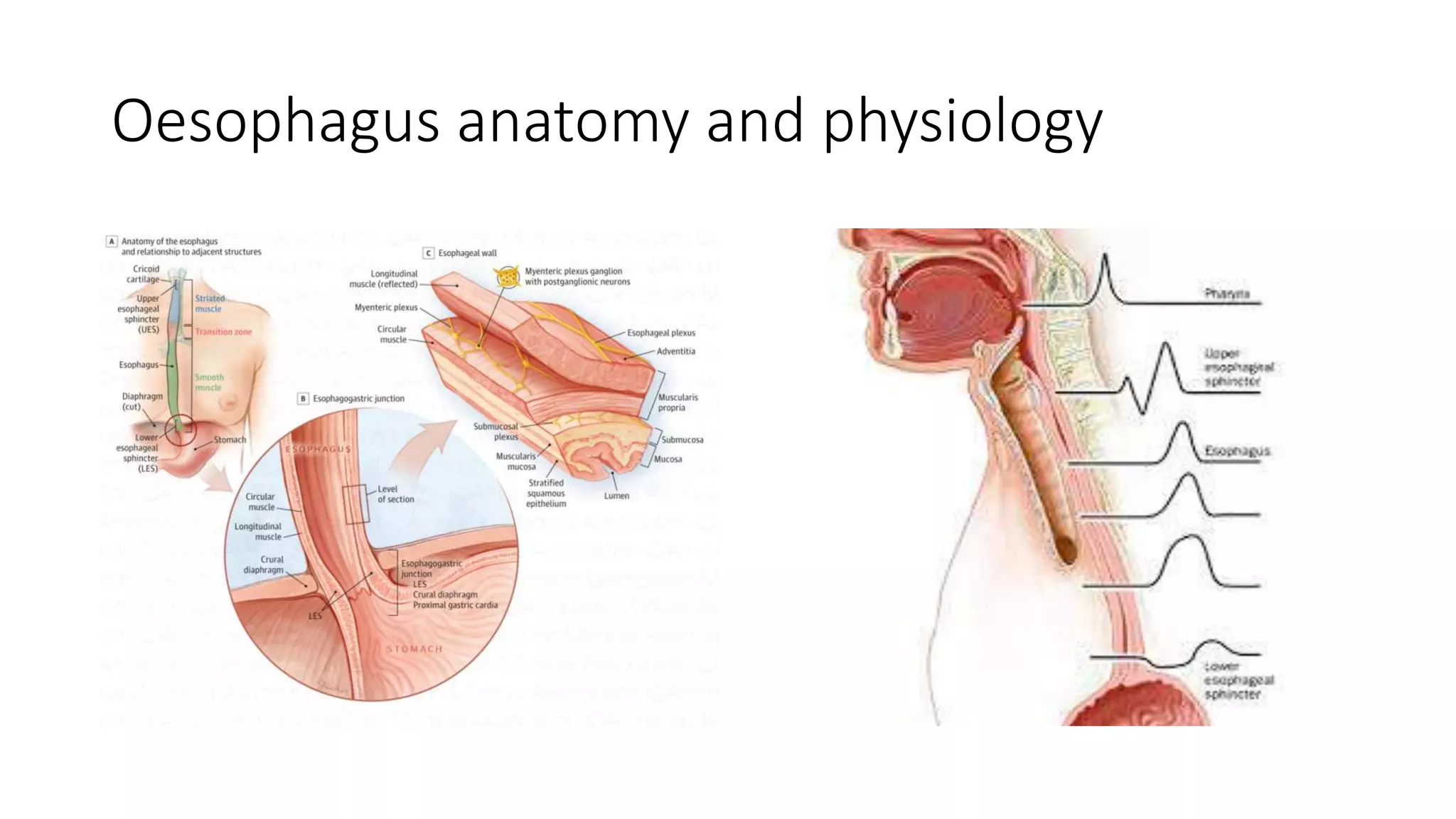
This document discusses oesophageal endoscopy procedures and their uses. It covers the anatomy and technology behind endoscopes, as well as various diagnostic and therapeutic applications. Key points include:
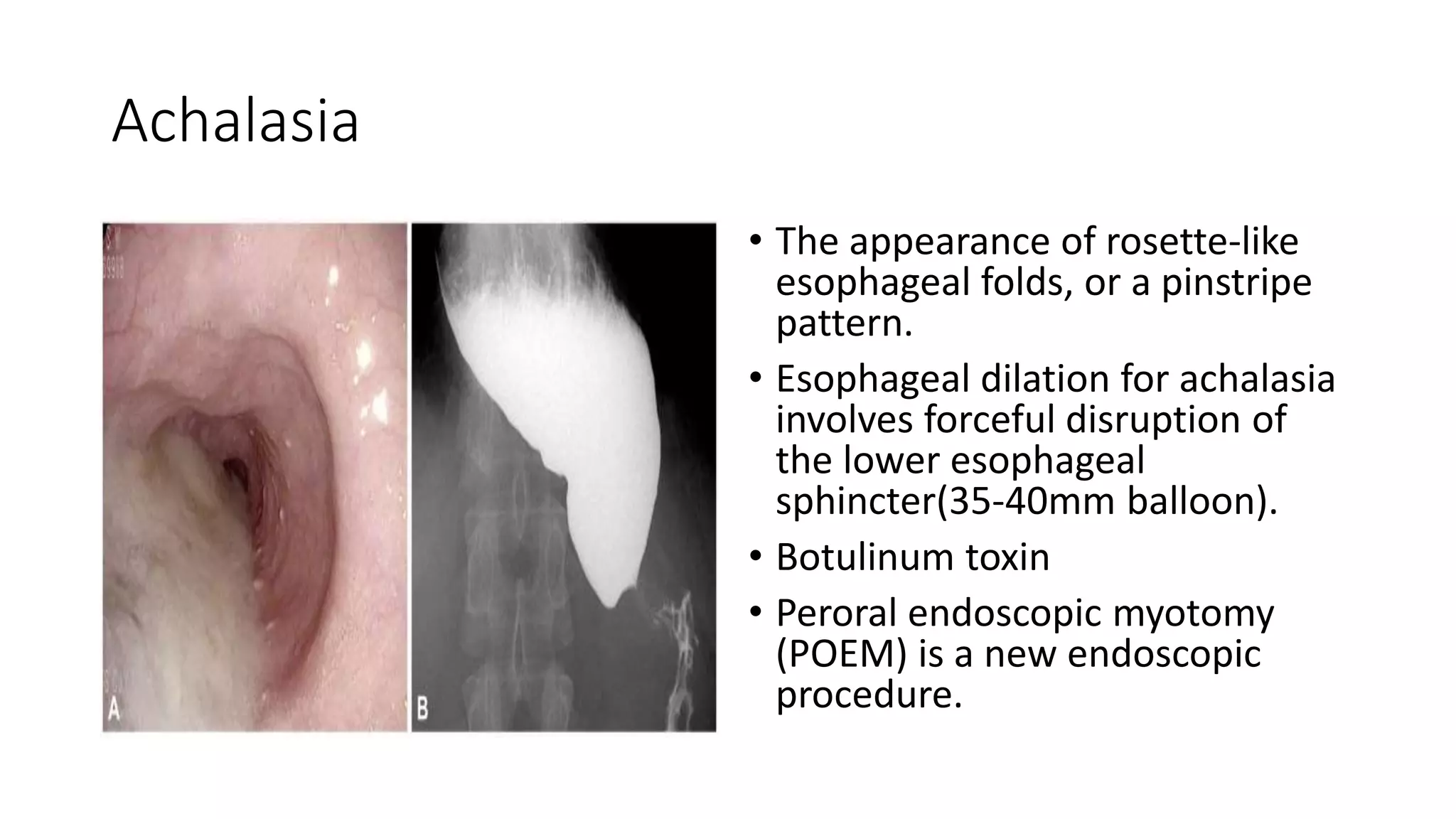
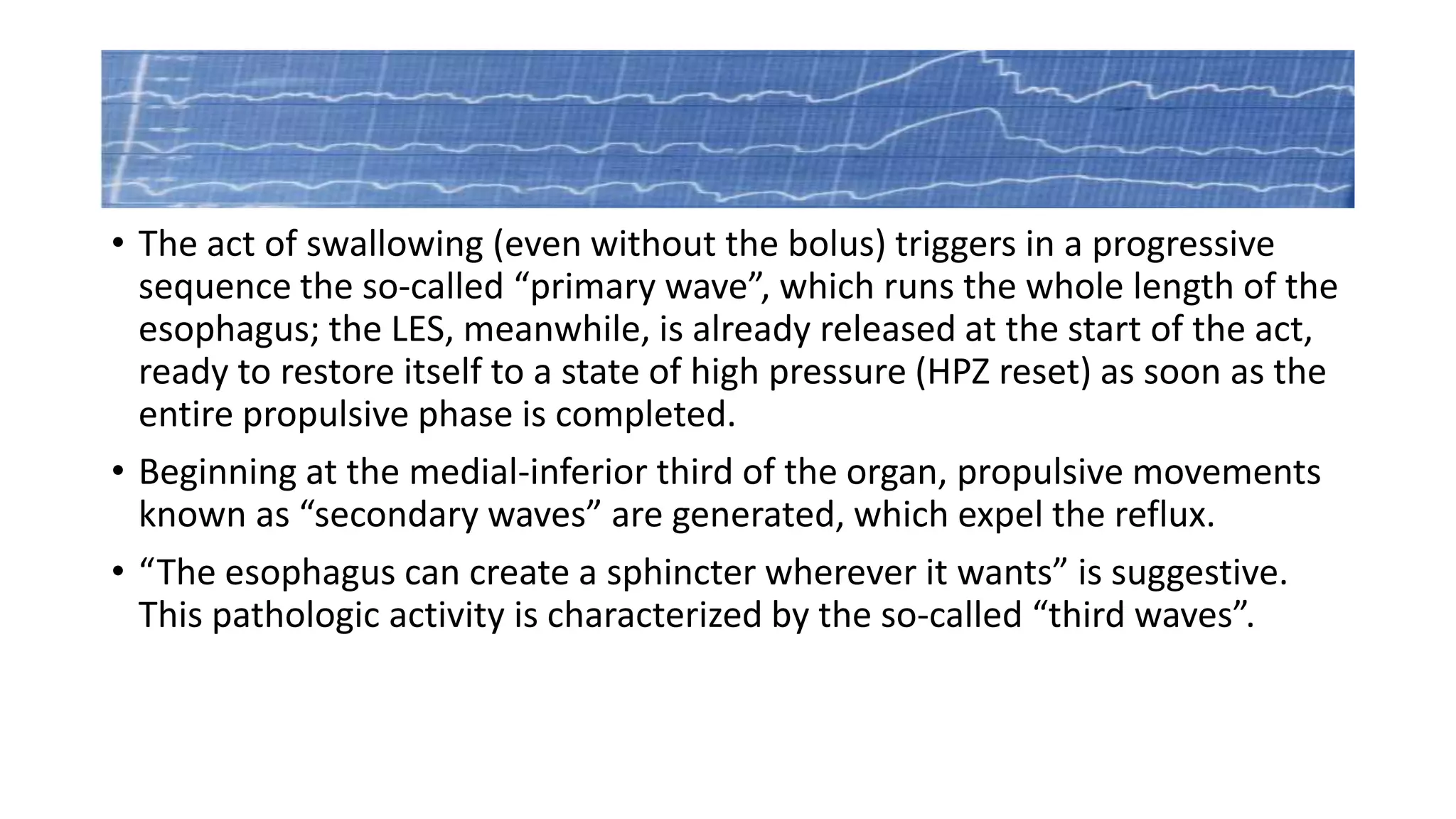
- Endoscopy has advanced from a purely diagnostic tool to one capable of various therapies for conditions like GERD, achalasia, and obesity.
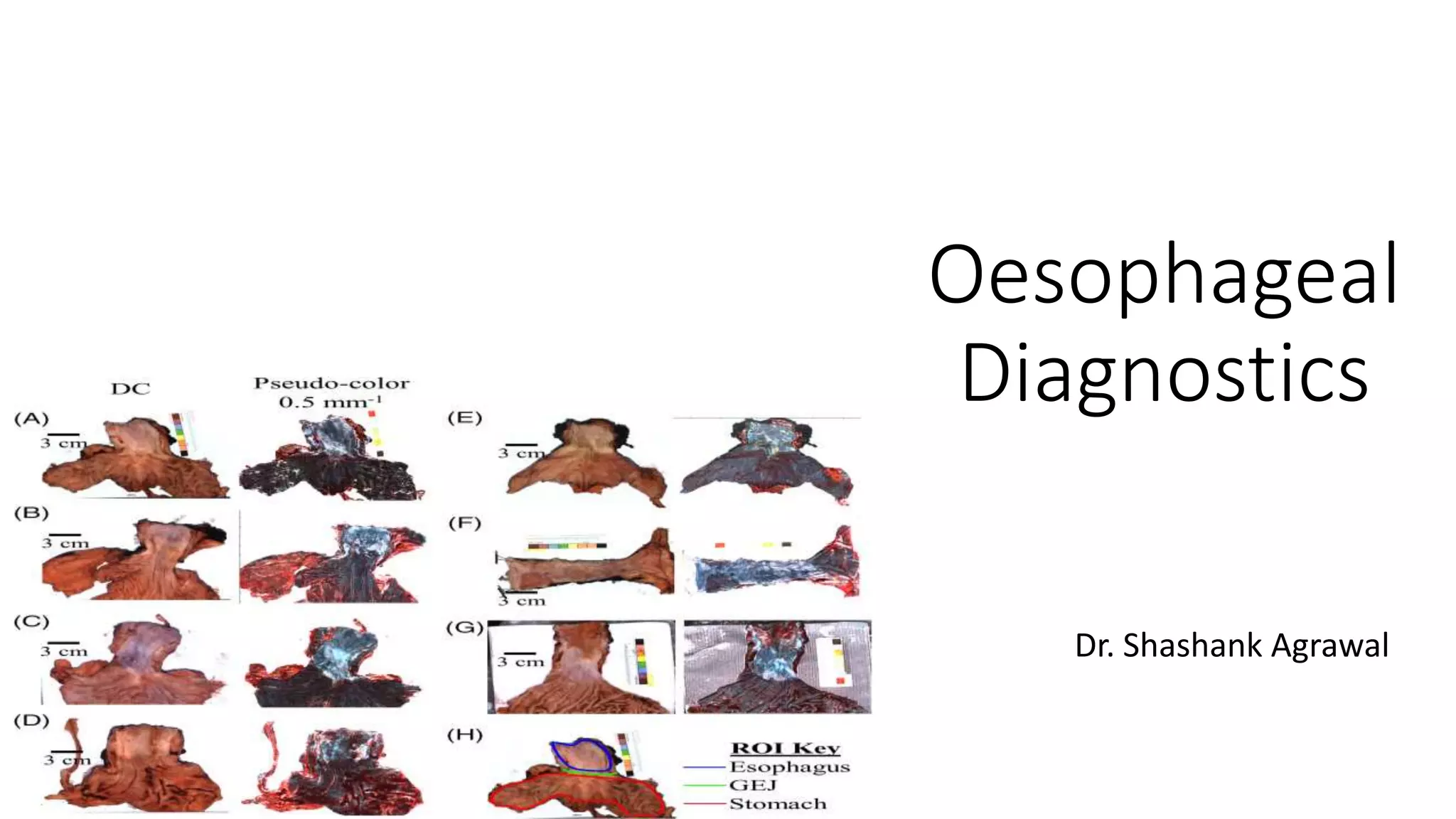
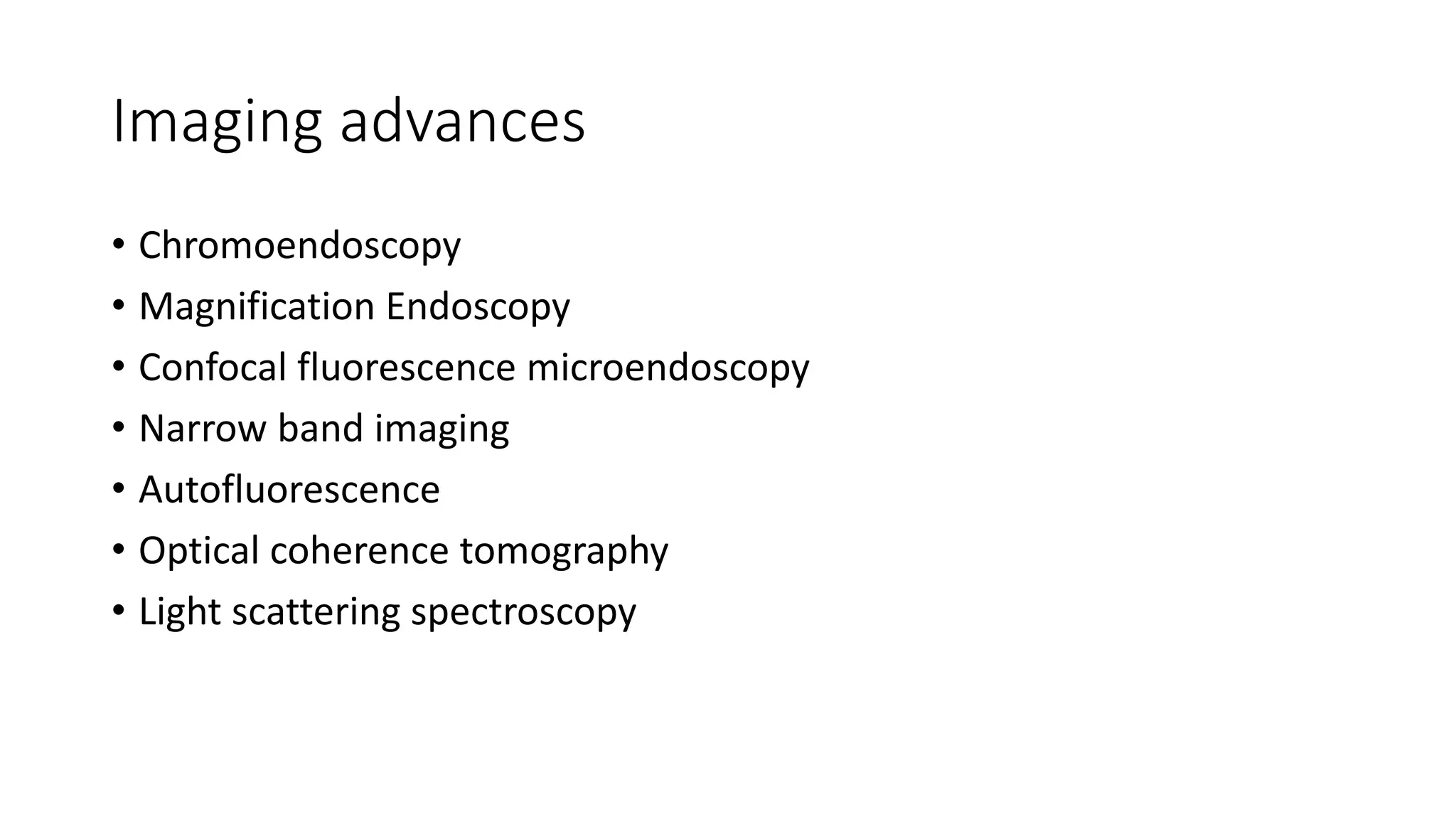
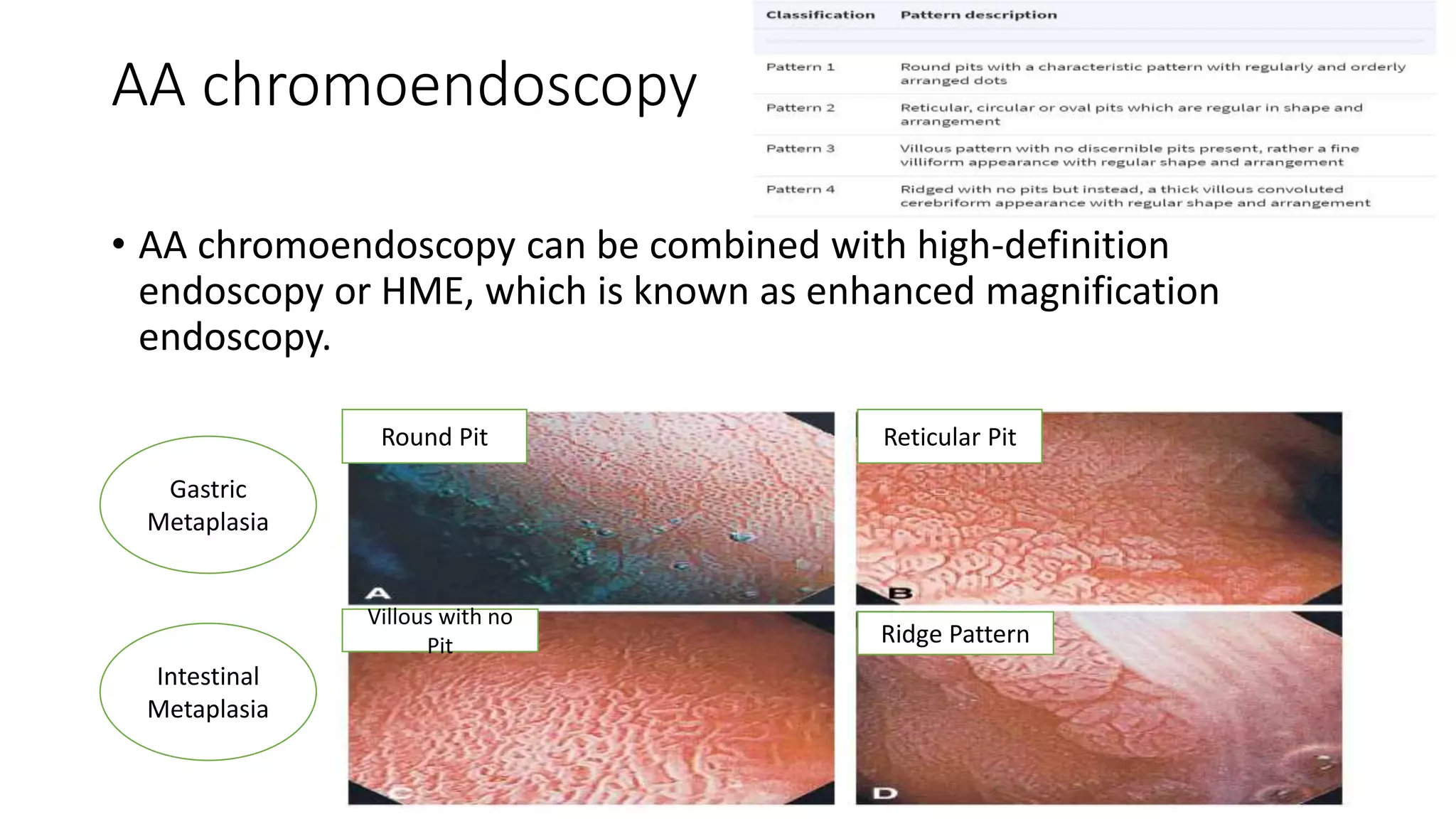
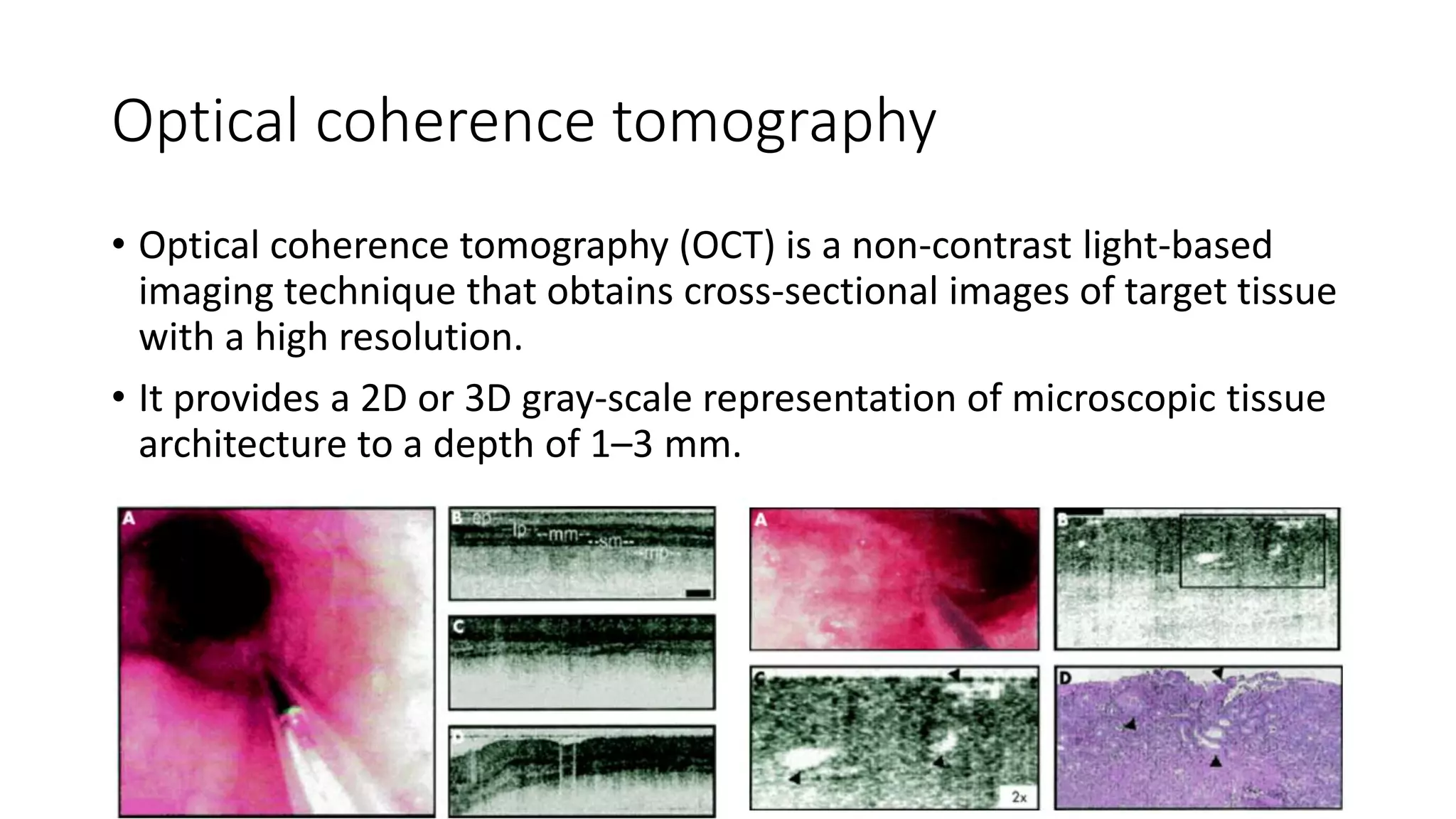
- Imaging technologies like chromoendoscopy and narrow band imaging help detect early neoplastic lesions and distinguish between dysplastic and non-dysplastic tissue.
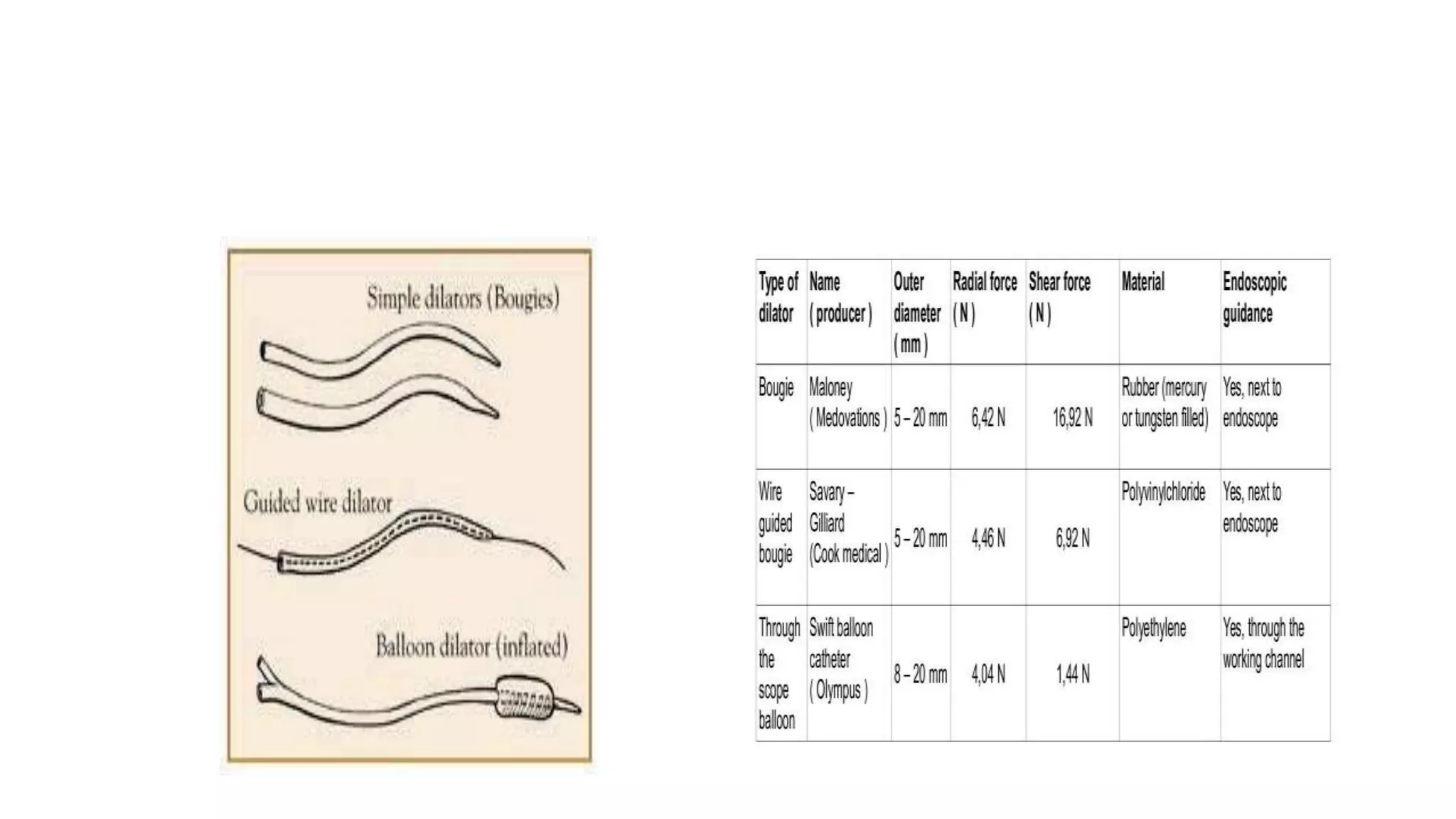
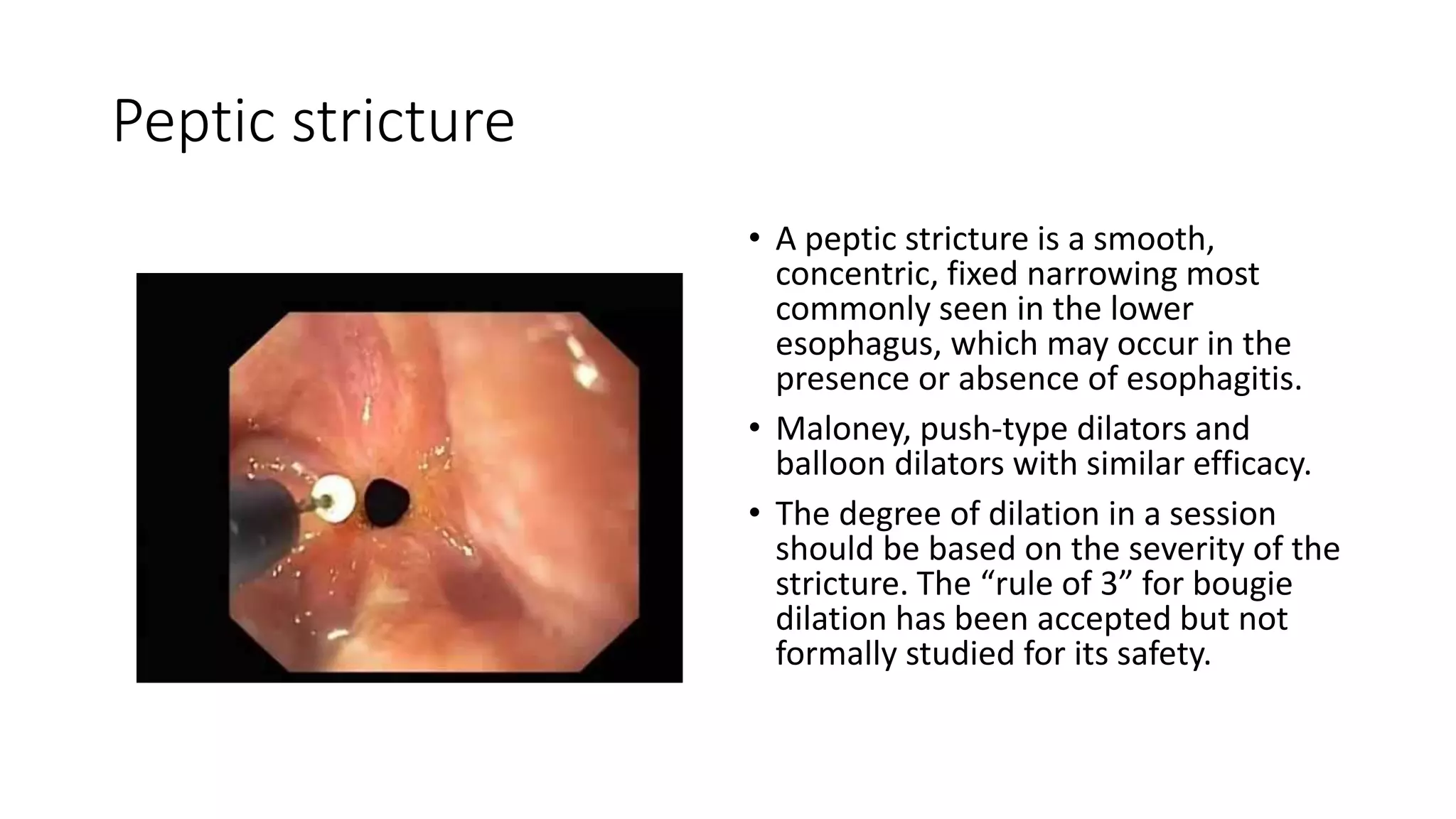
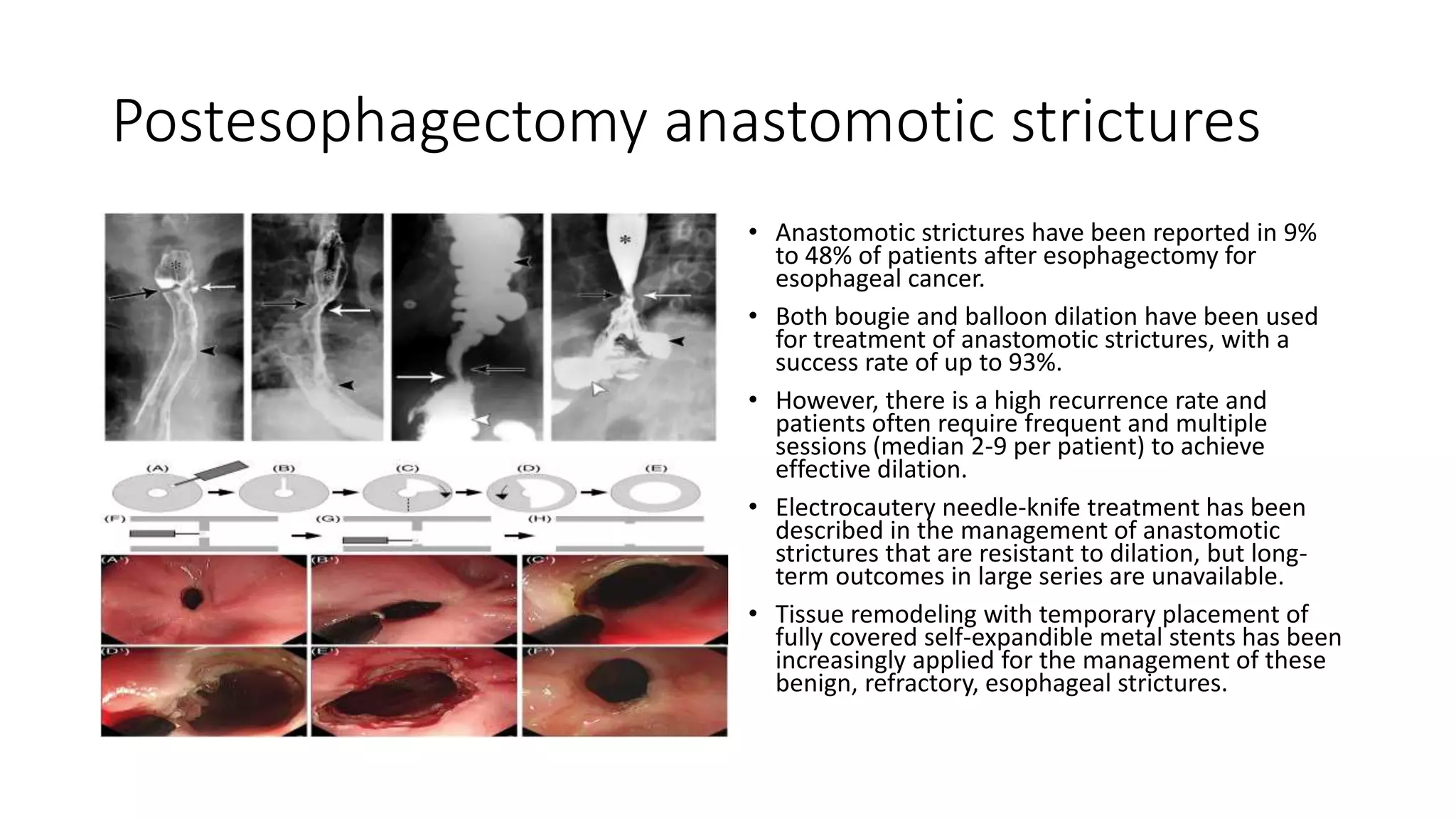
- Endoscopy is used to diagnose and treat conditions that cause dysphagia like peptic strictures, Schatzki rings, eosinophilic esophagitis, and post-surgical an