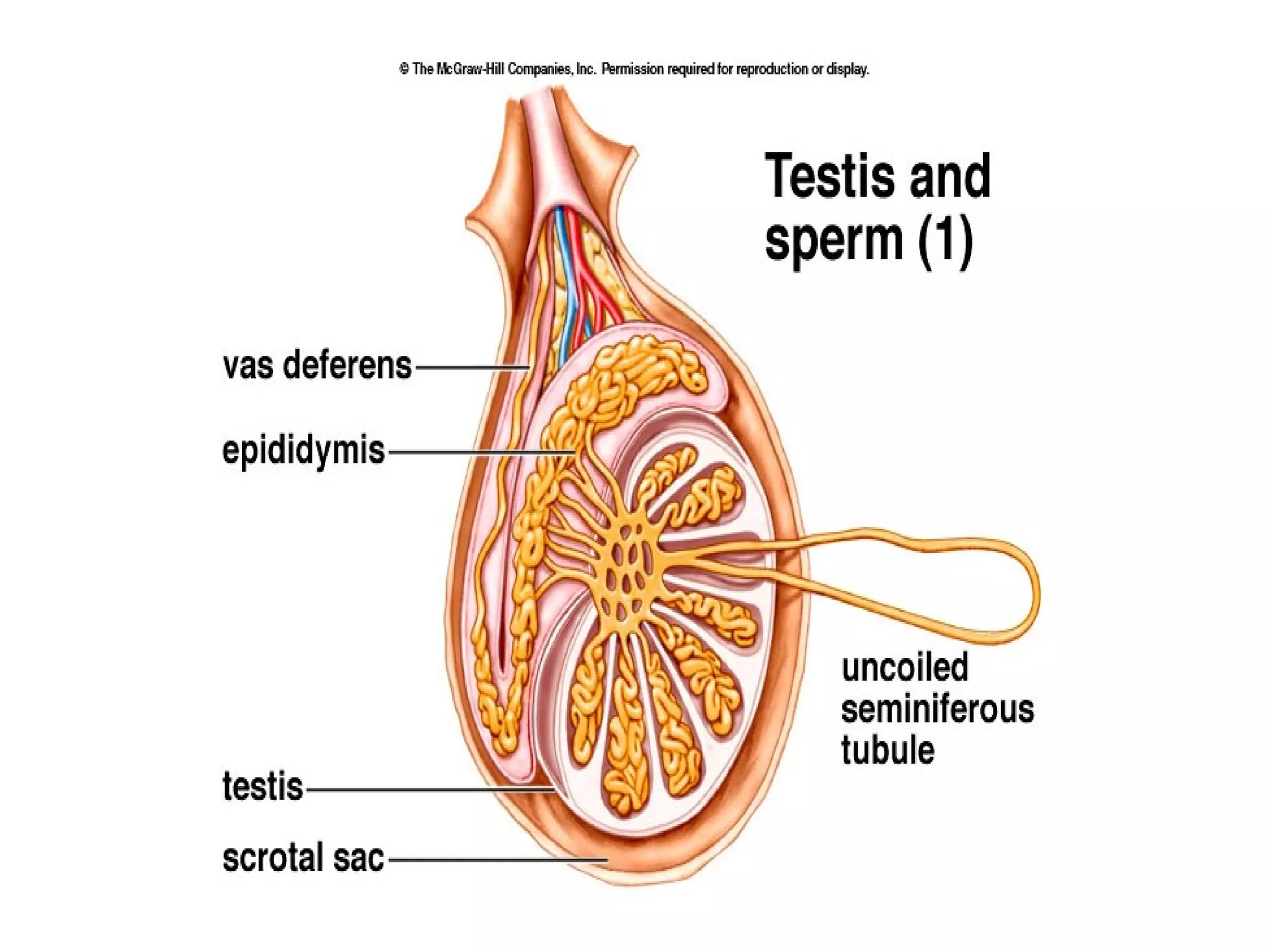
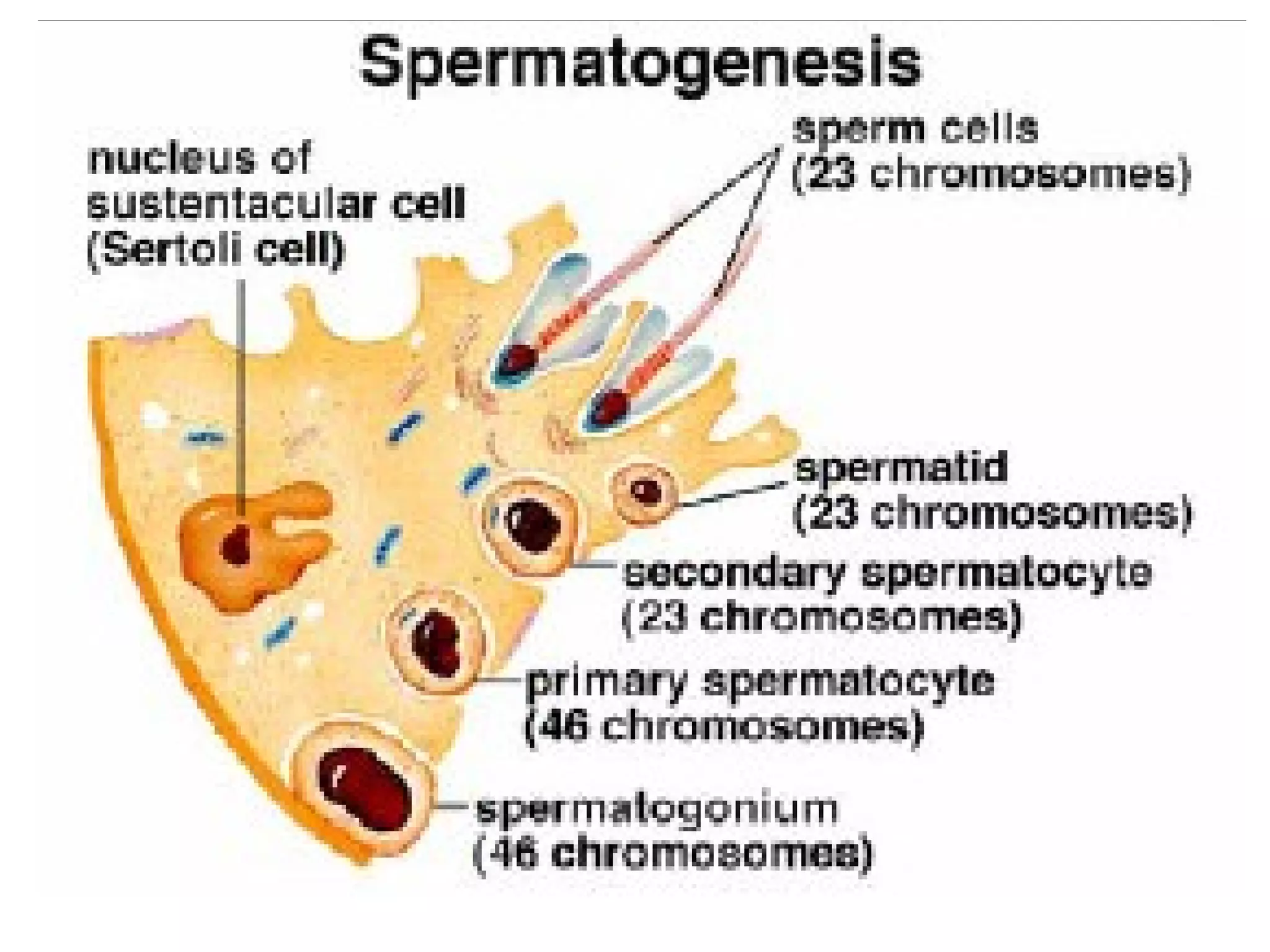
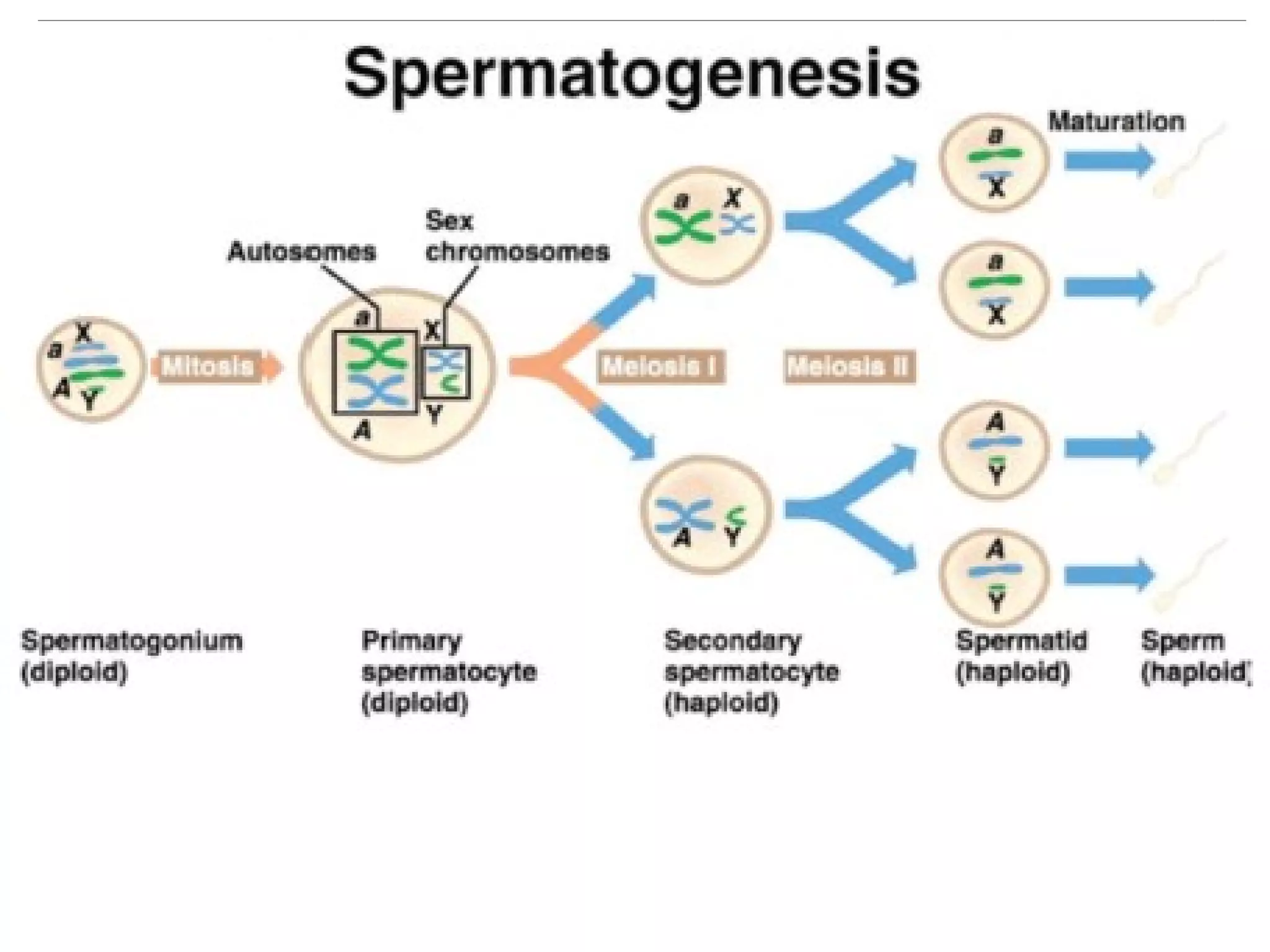
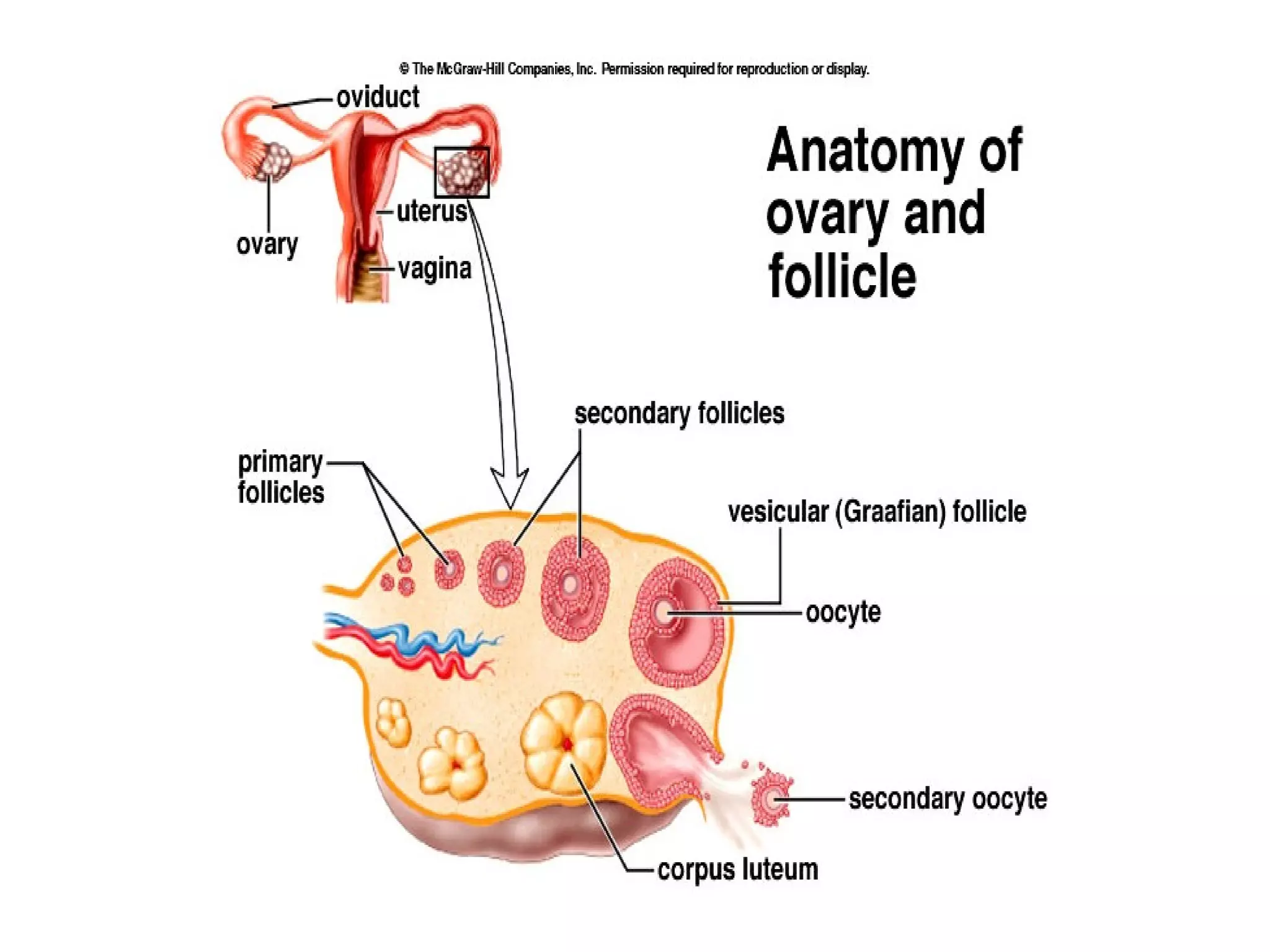
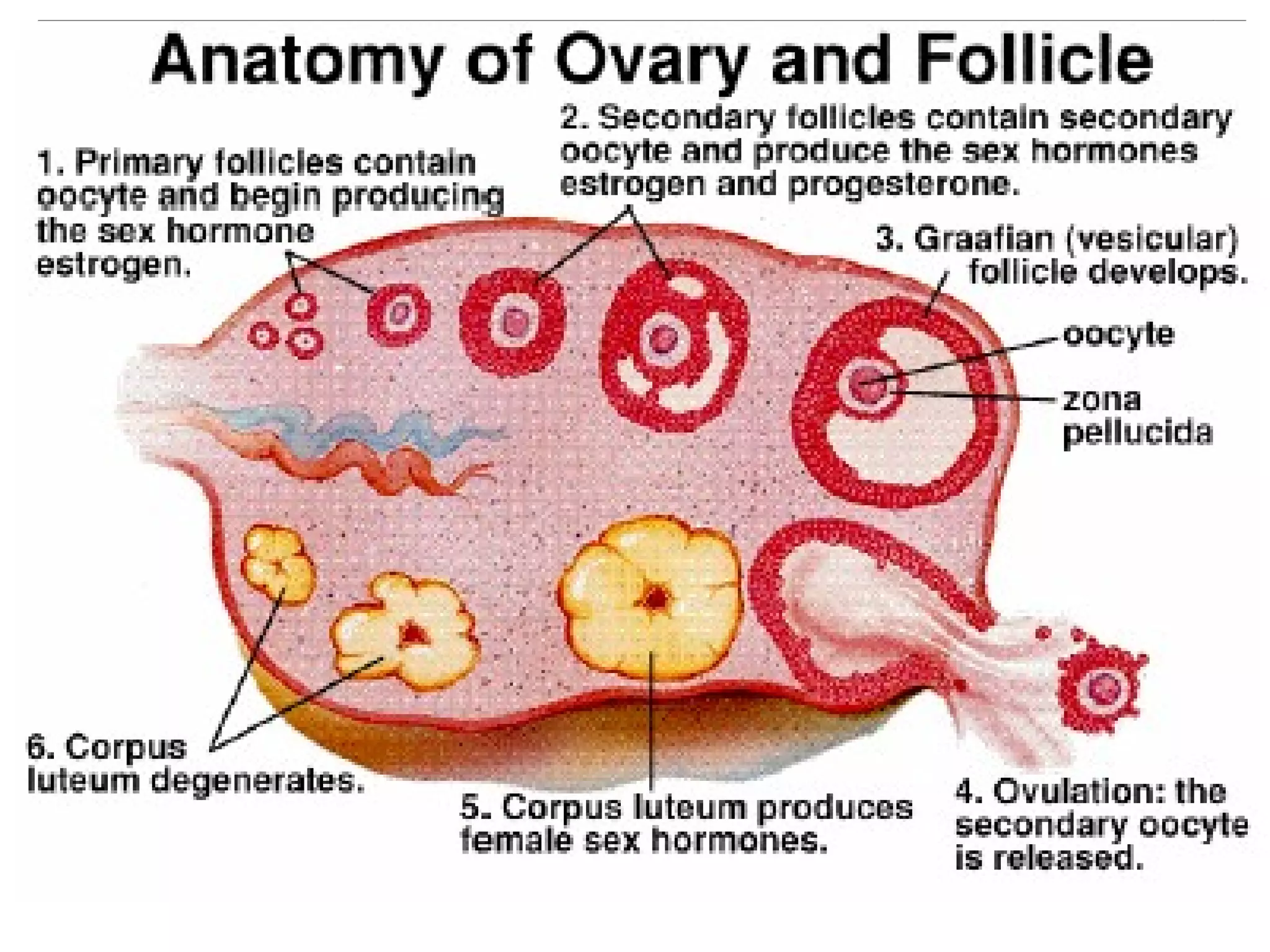
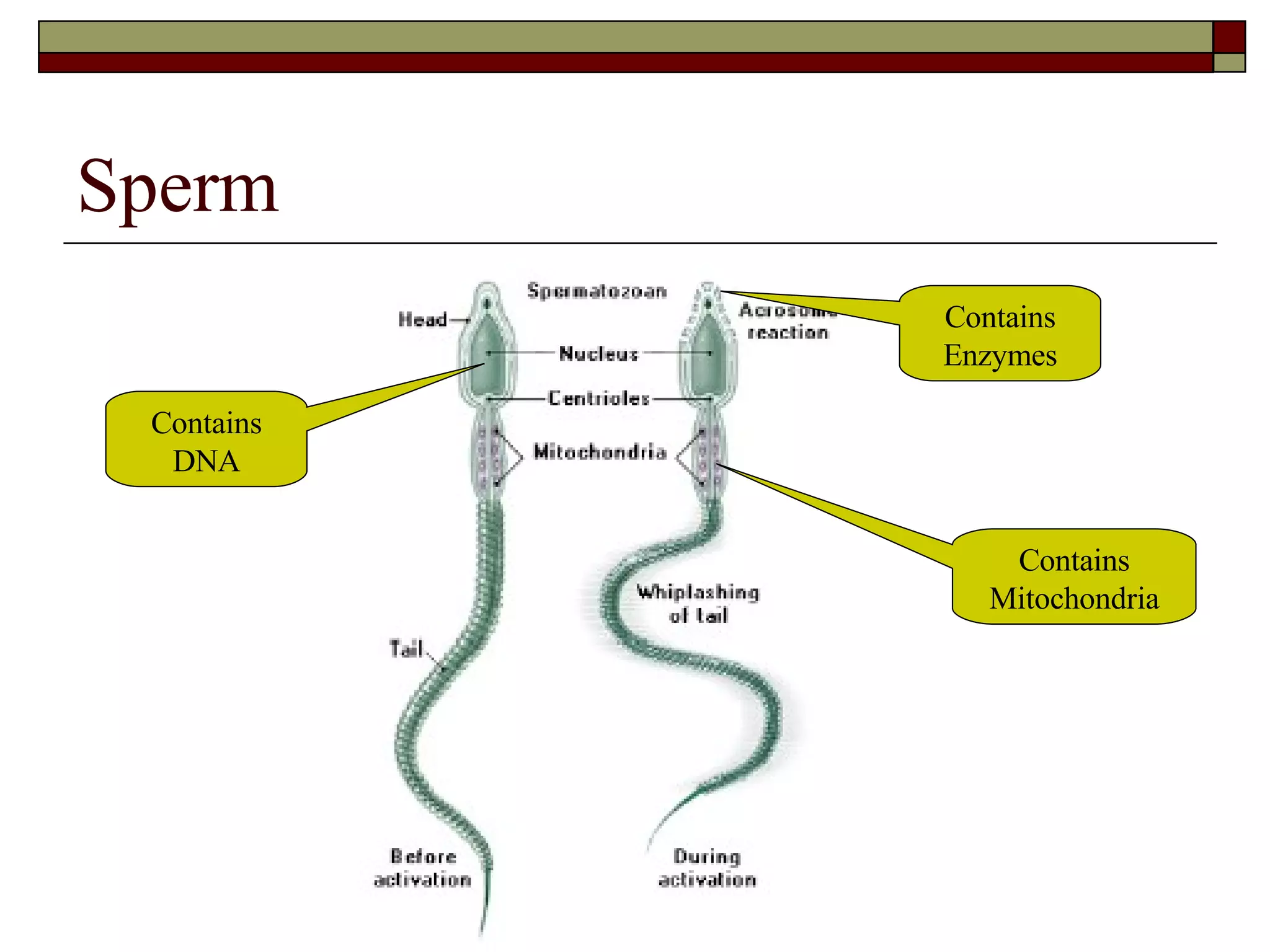
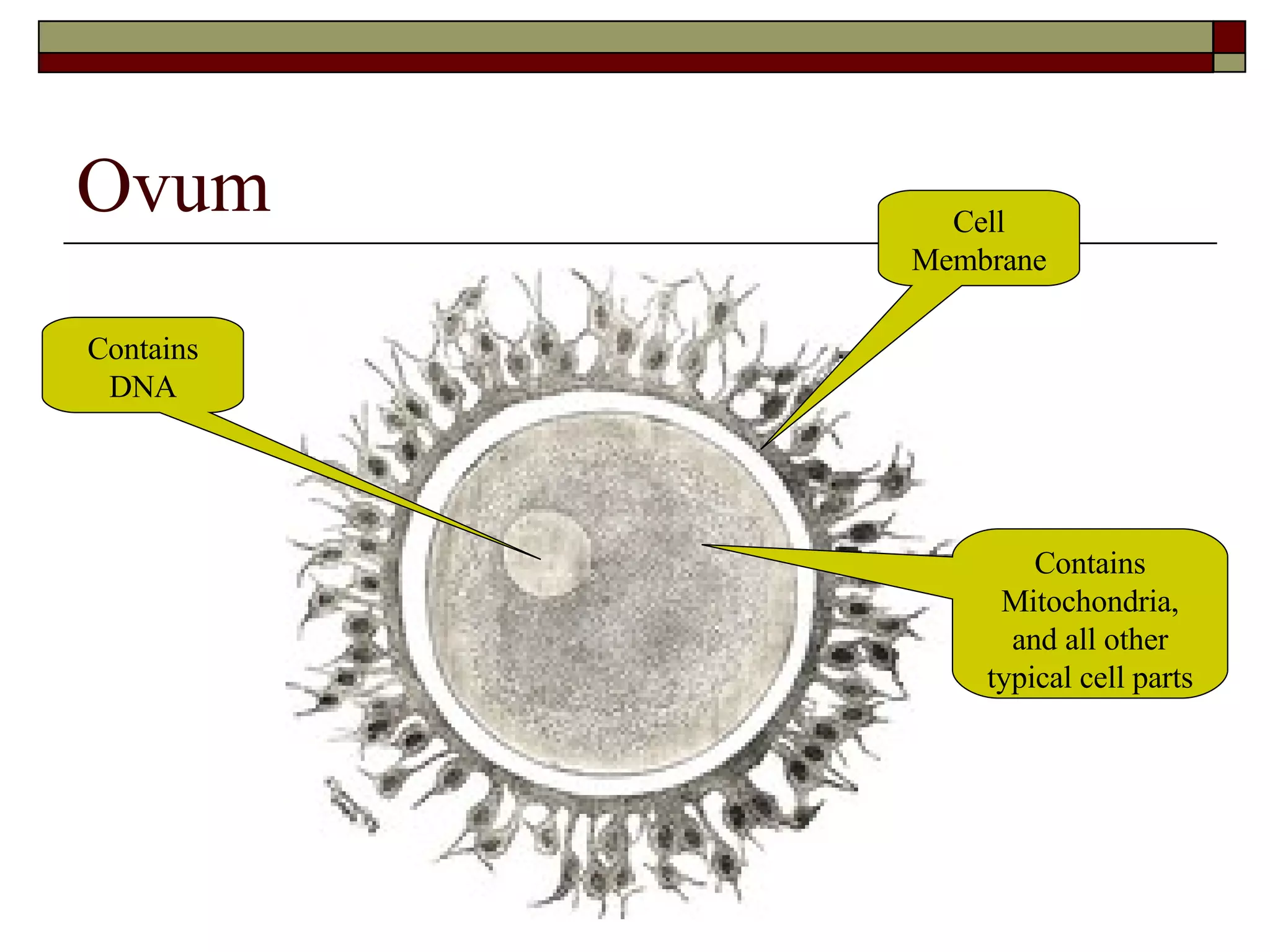
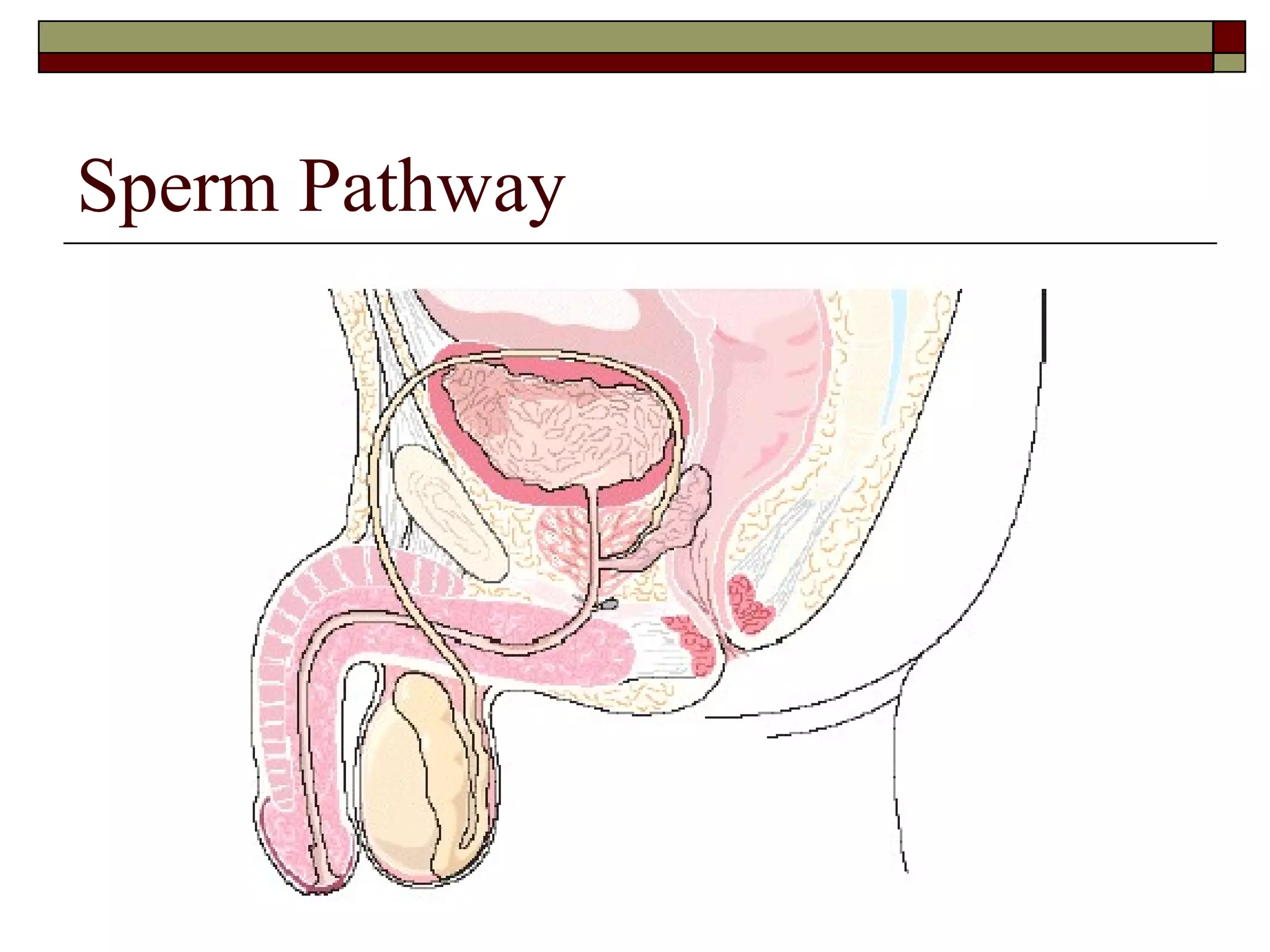
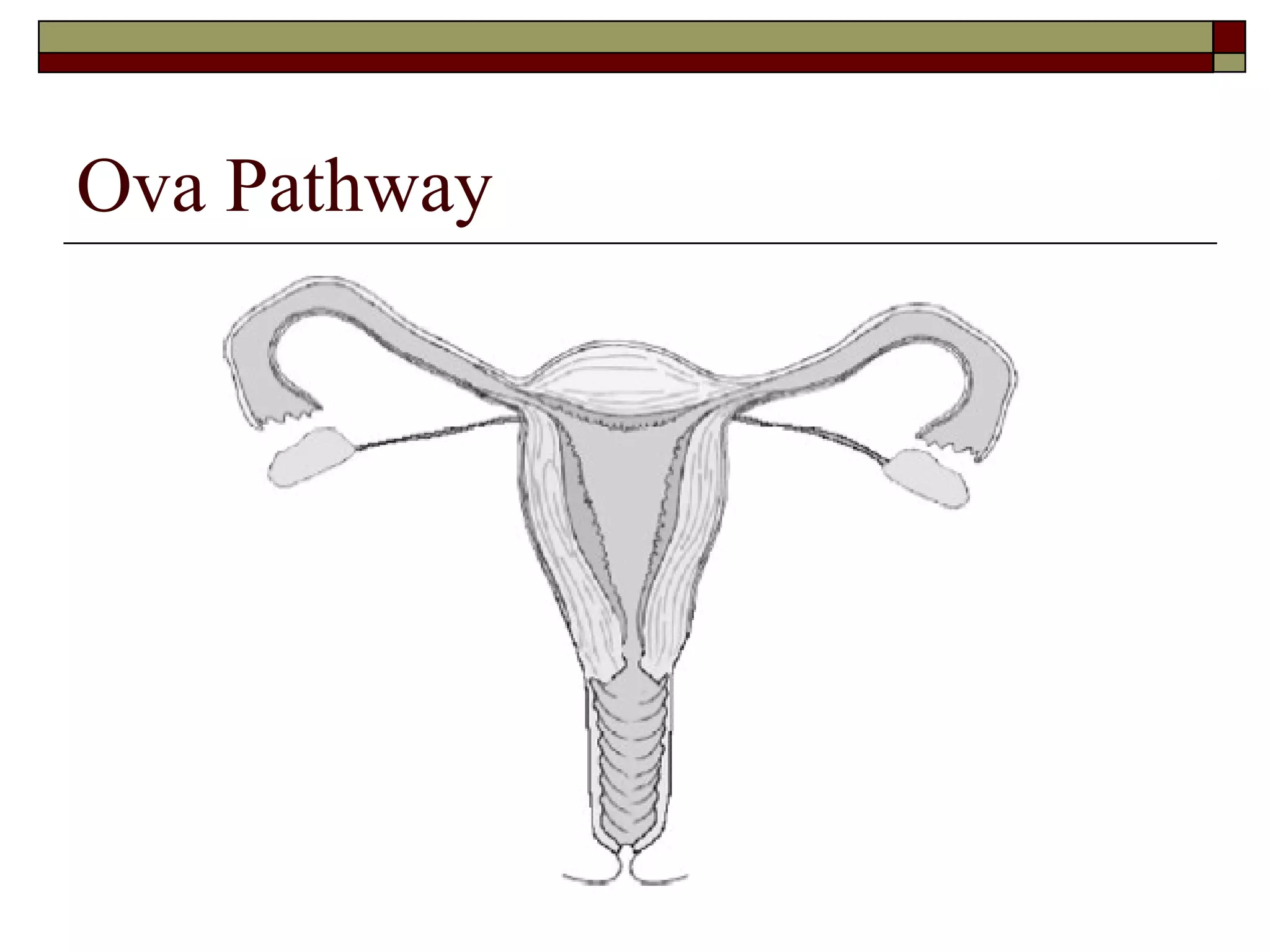
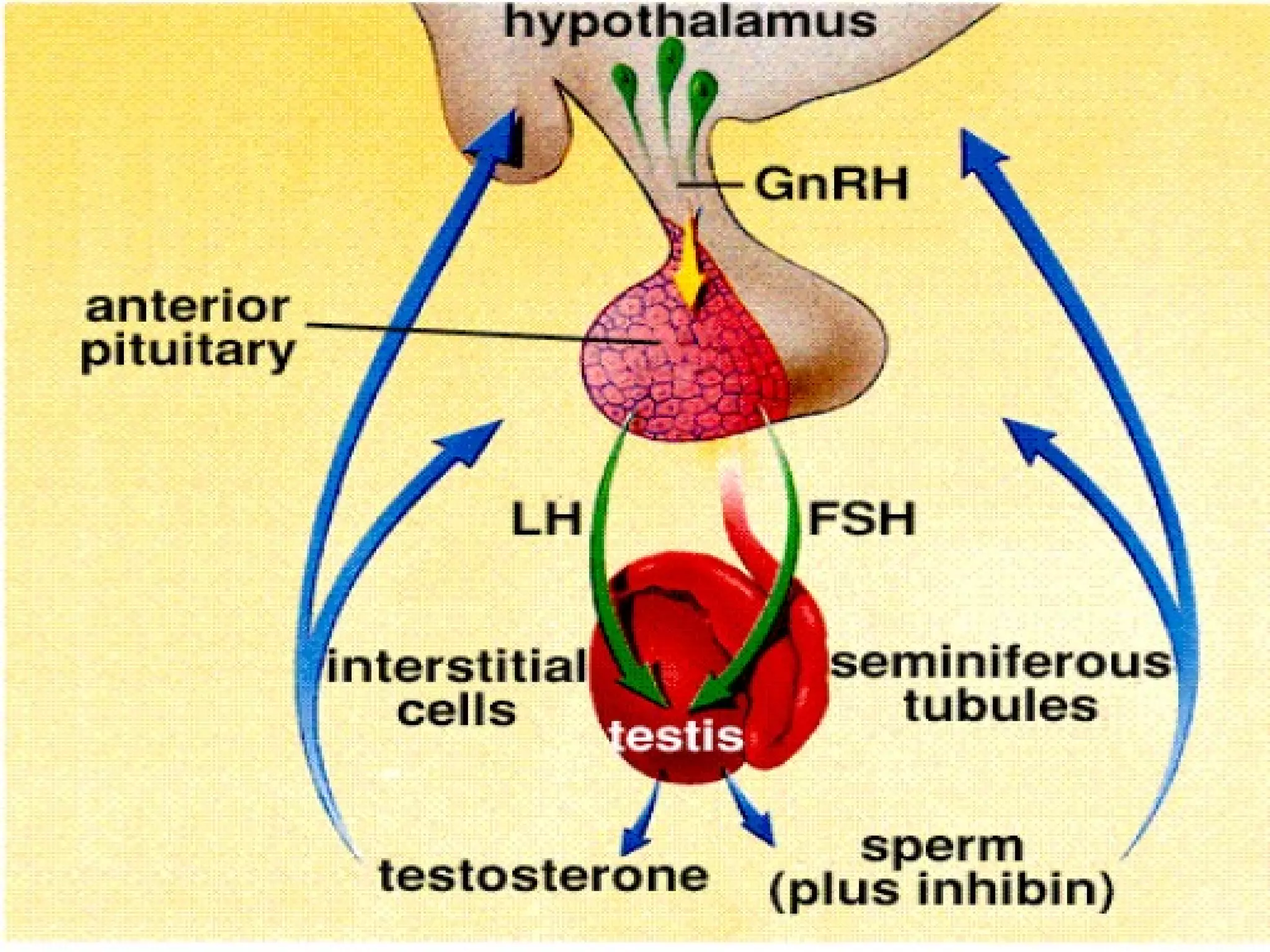
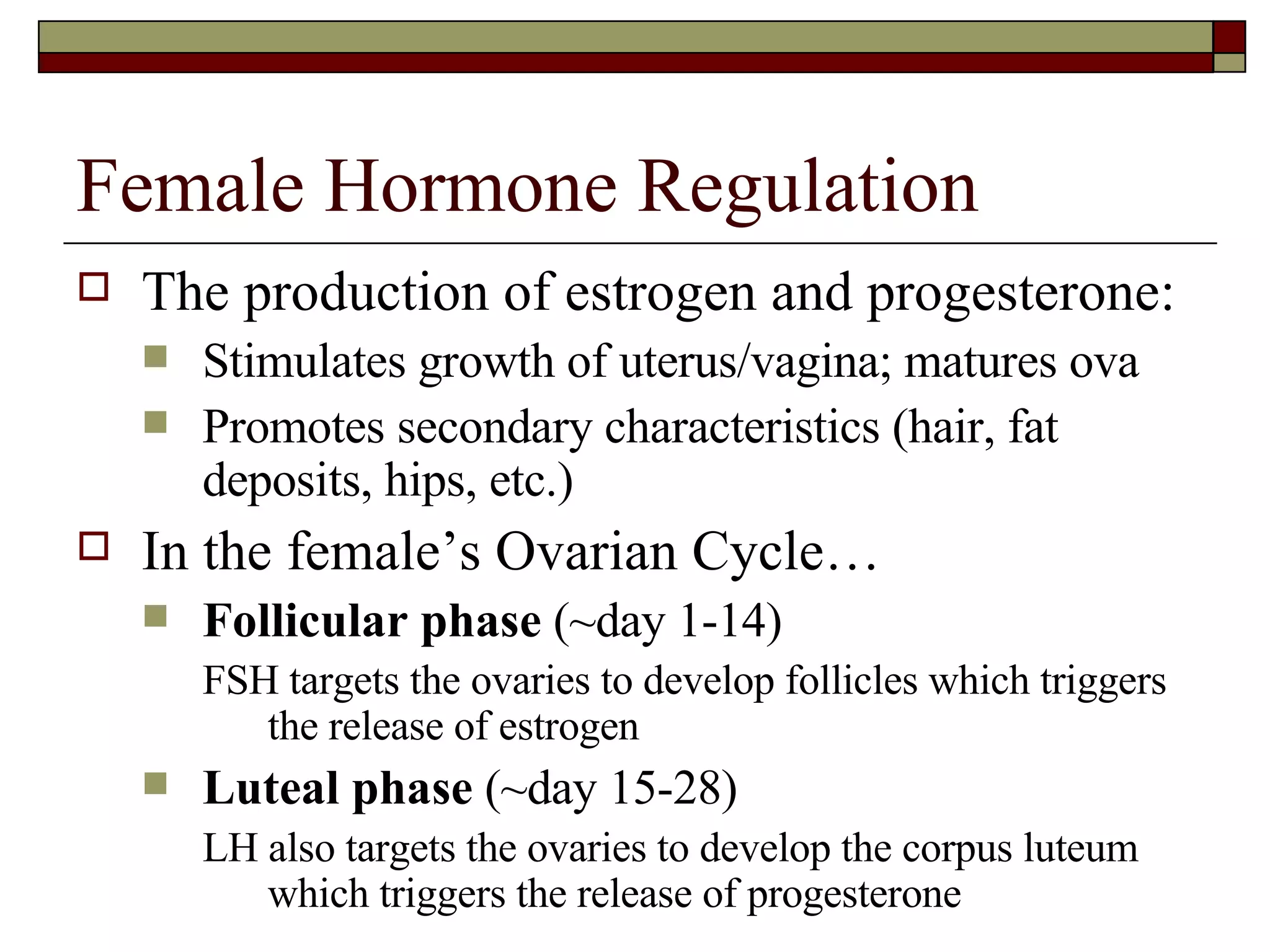
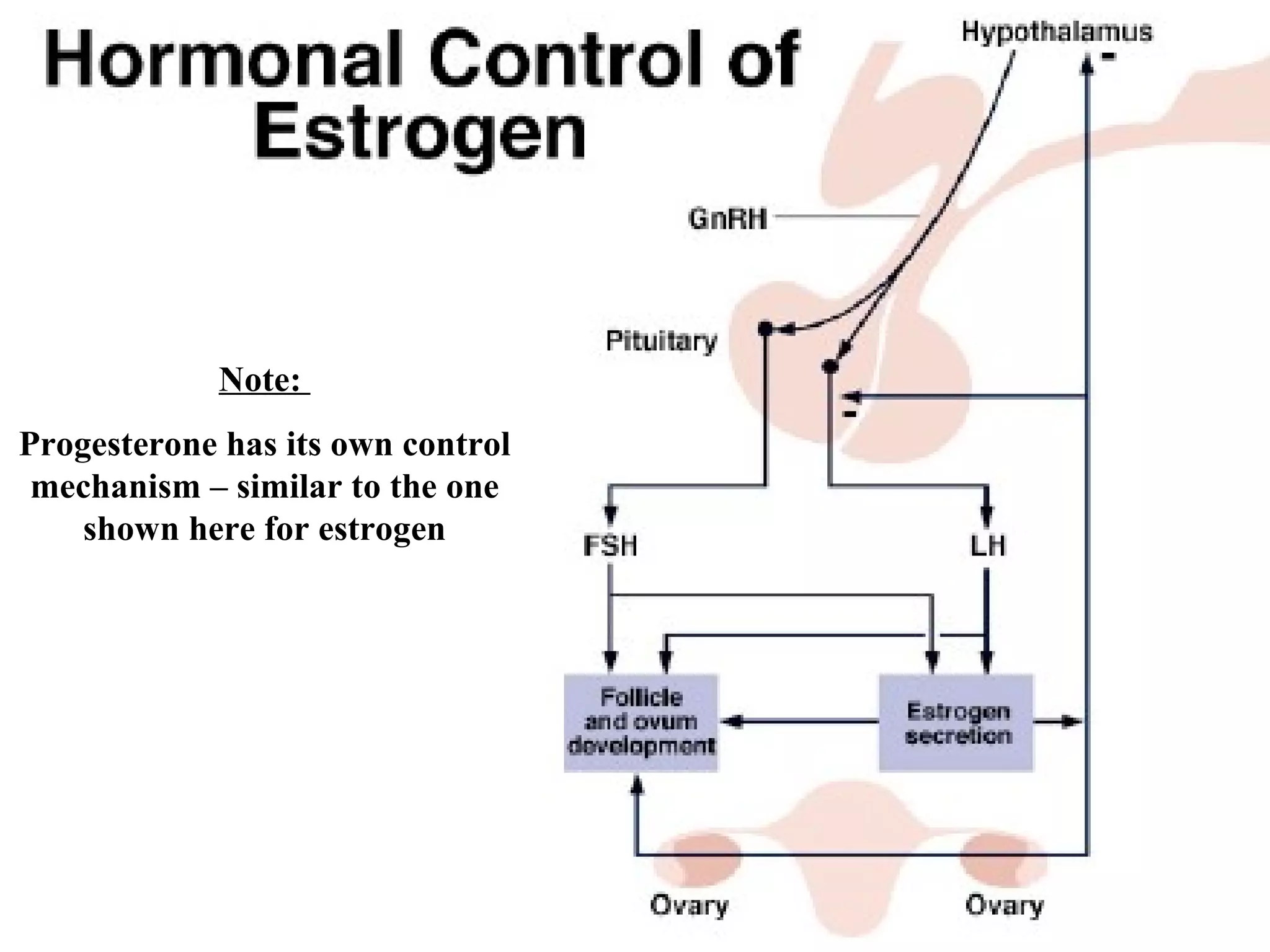
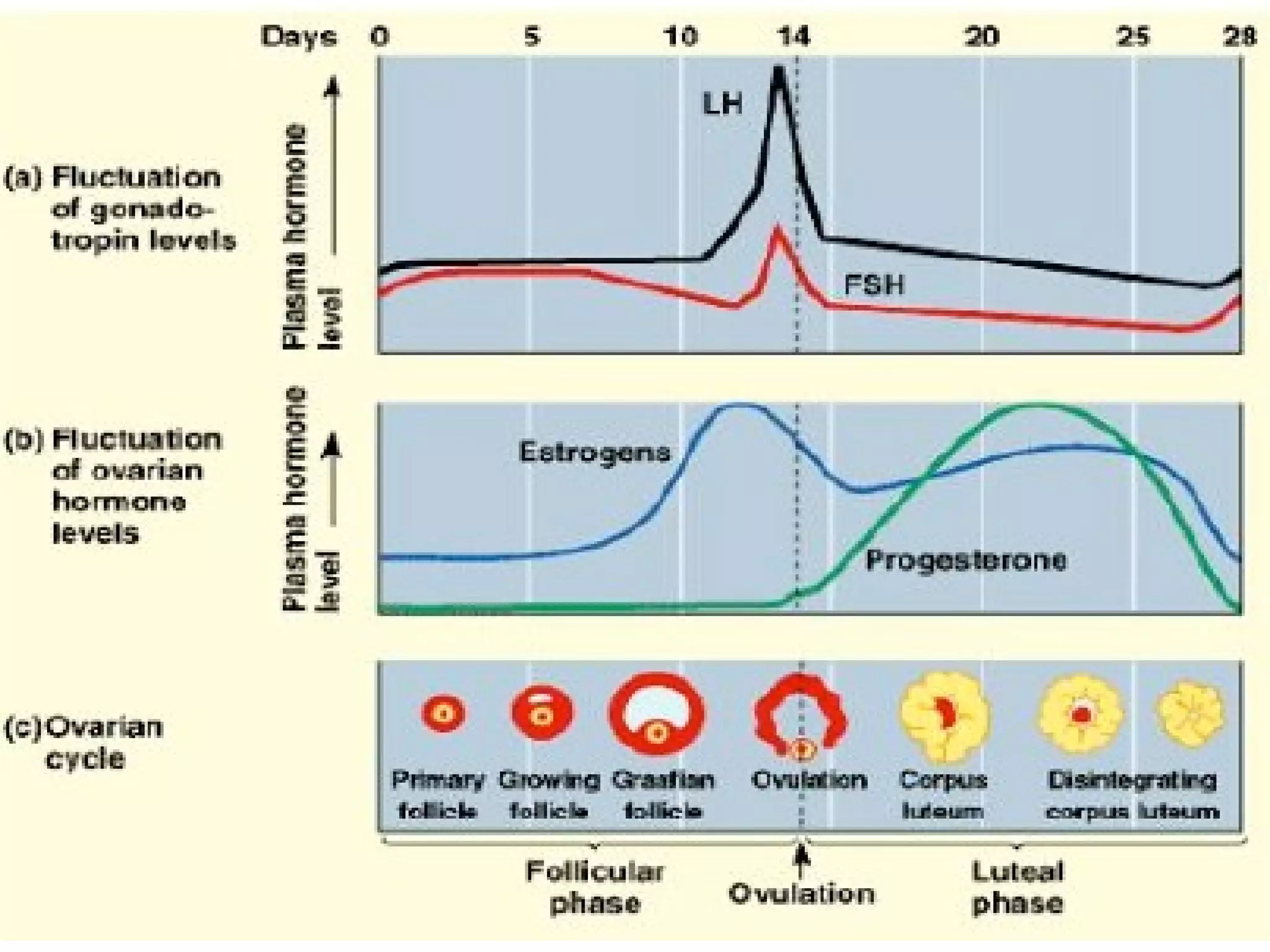
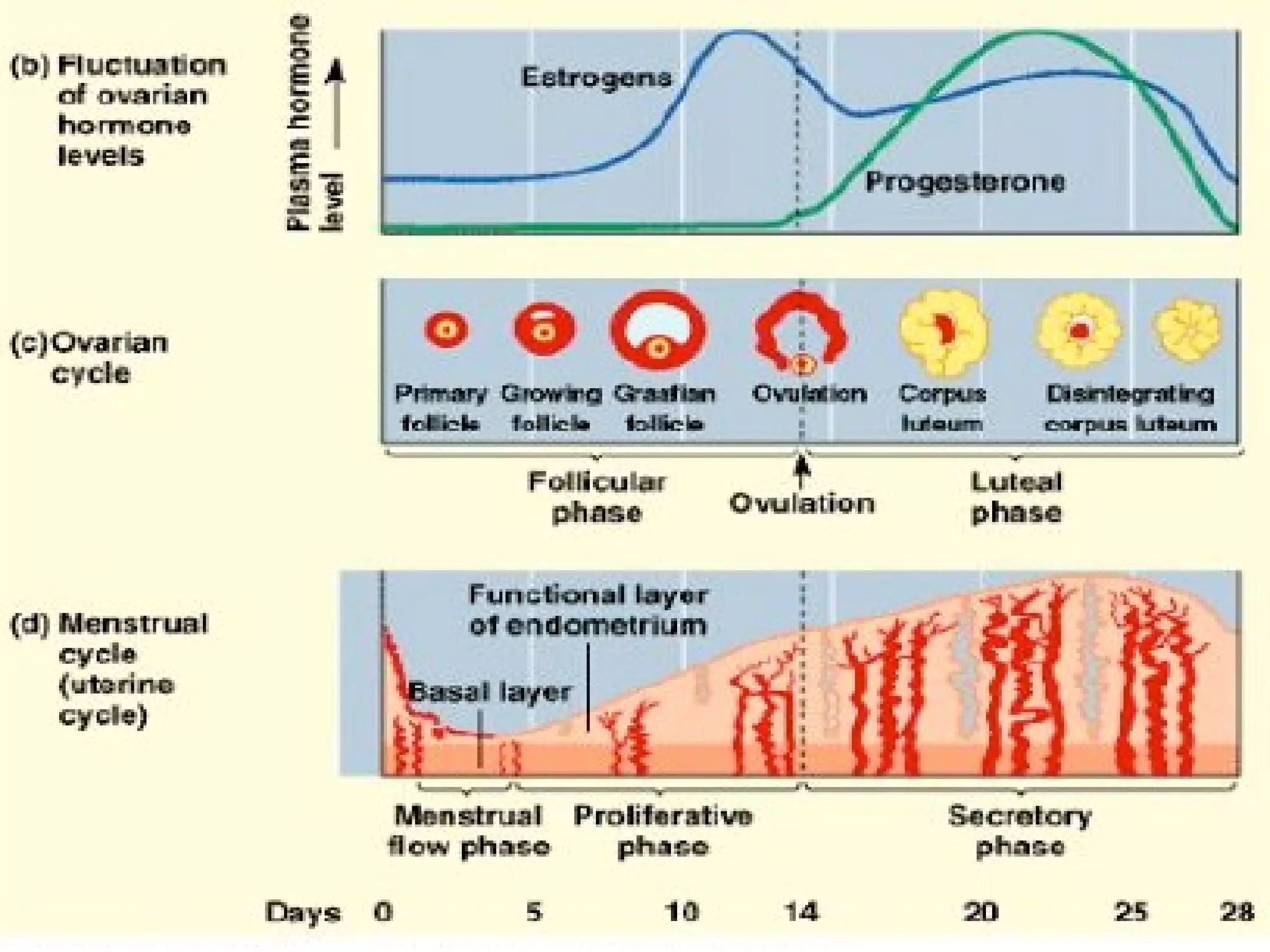
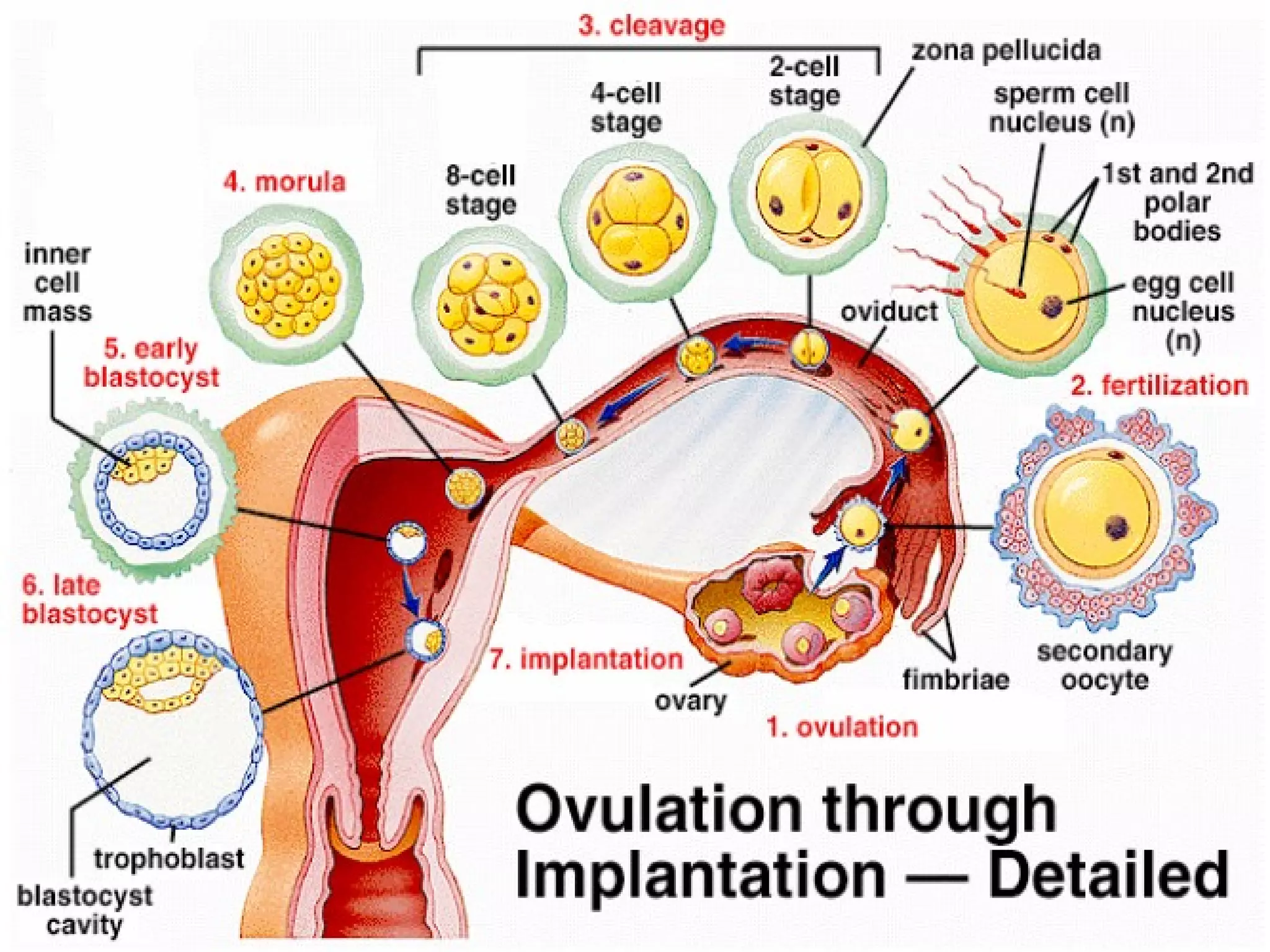
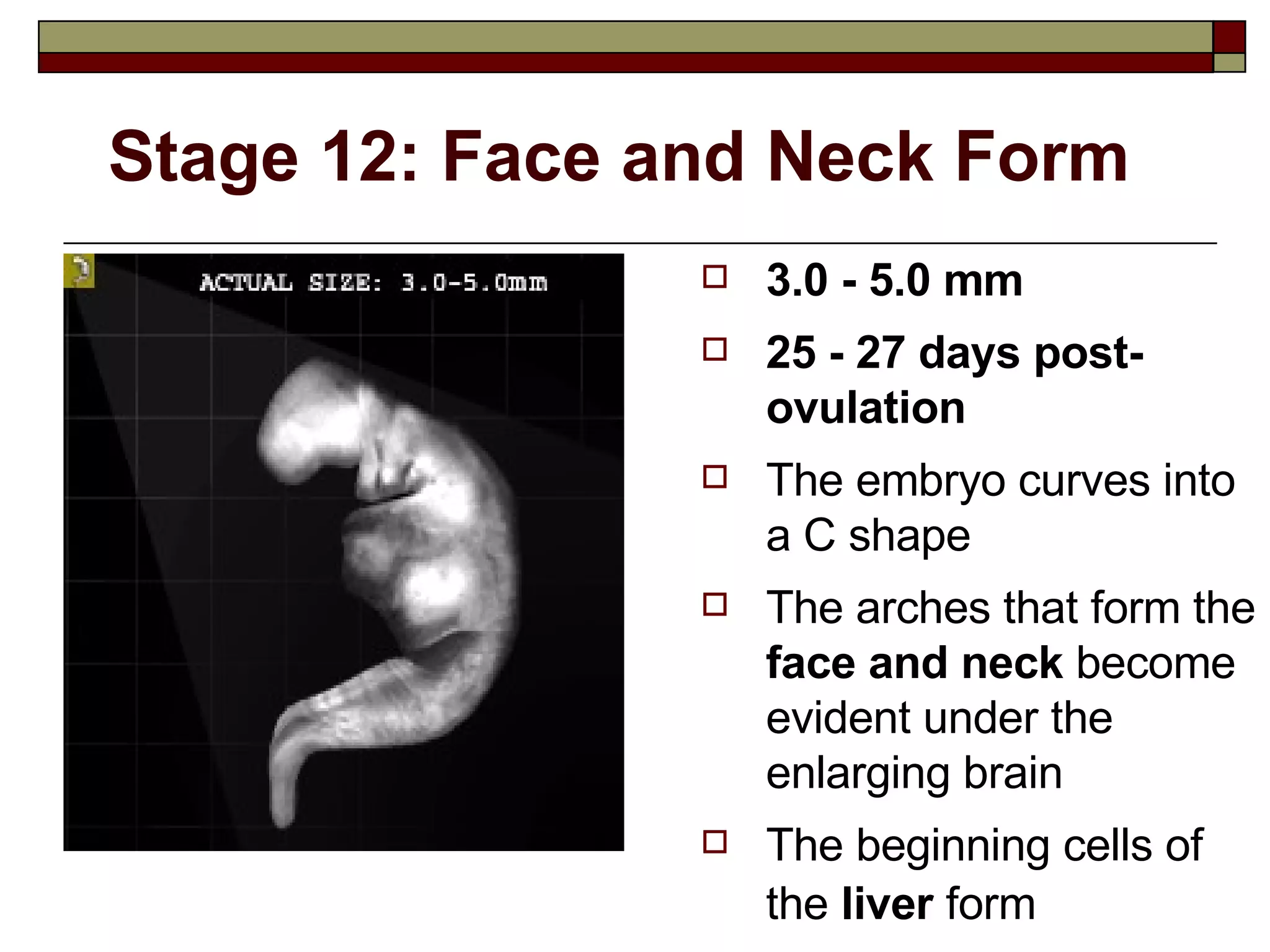
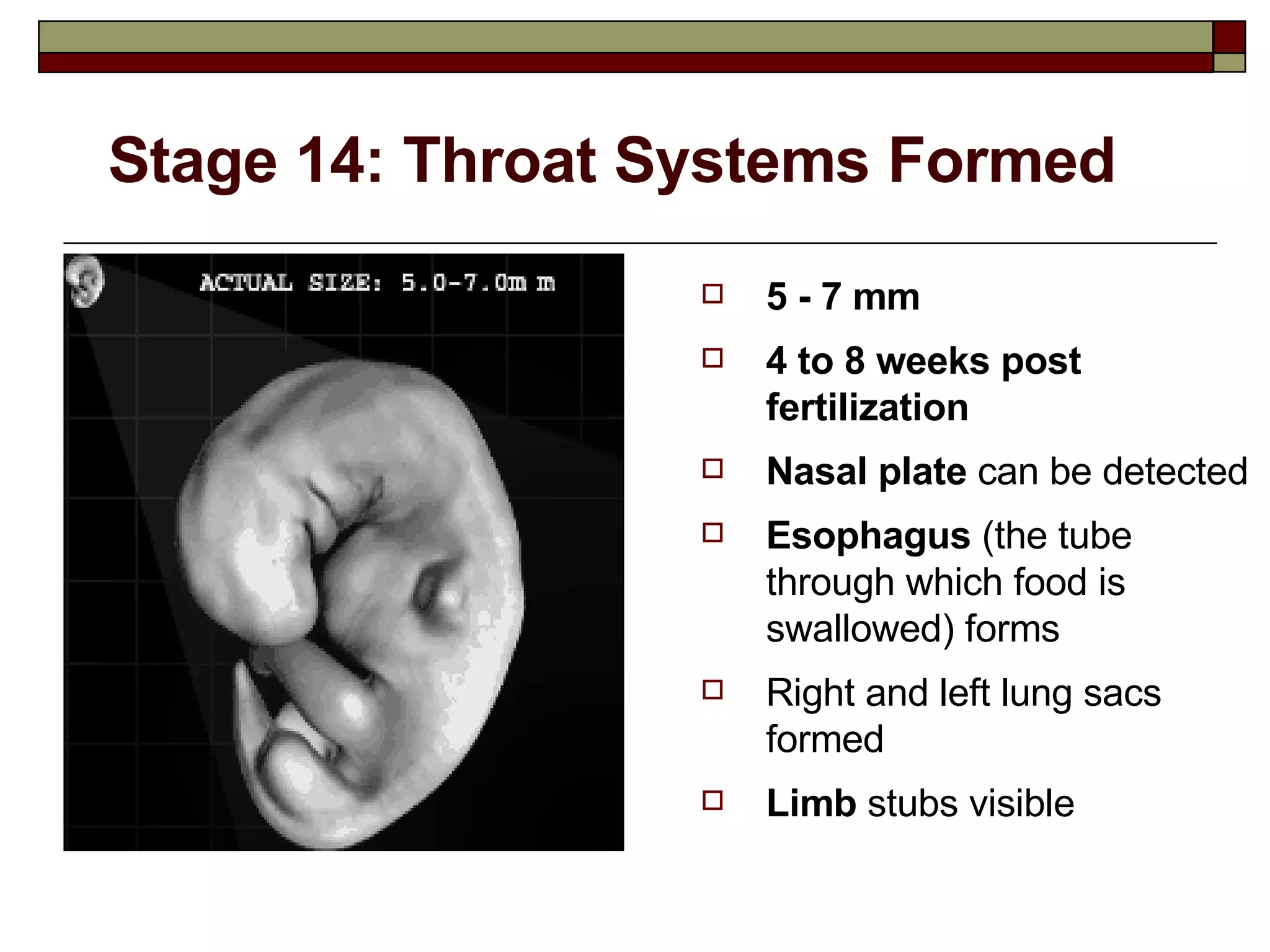
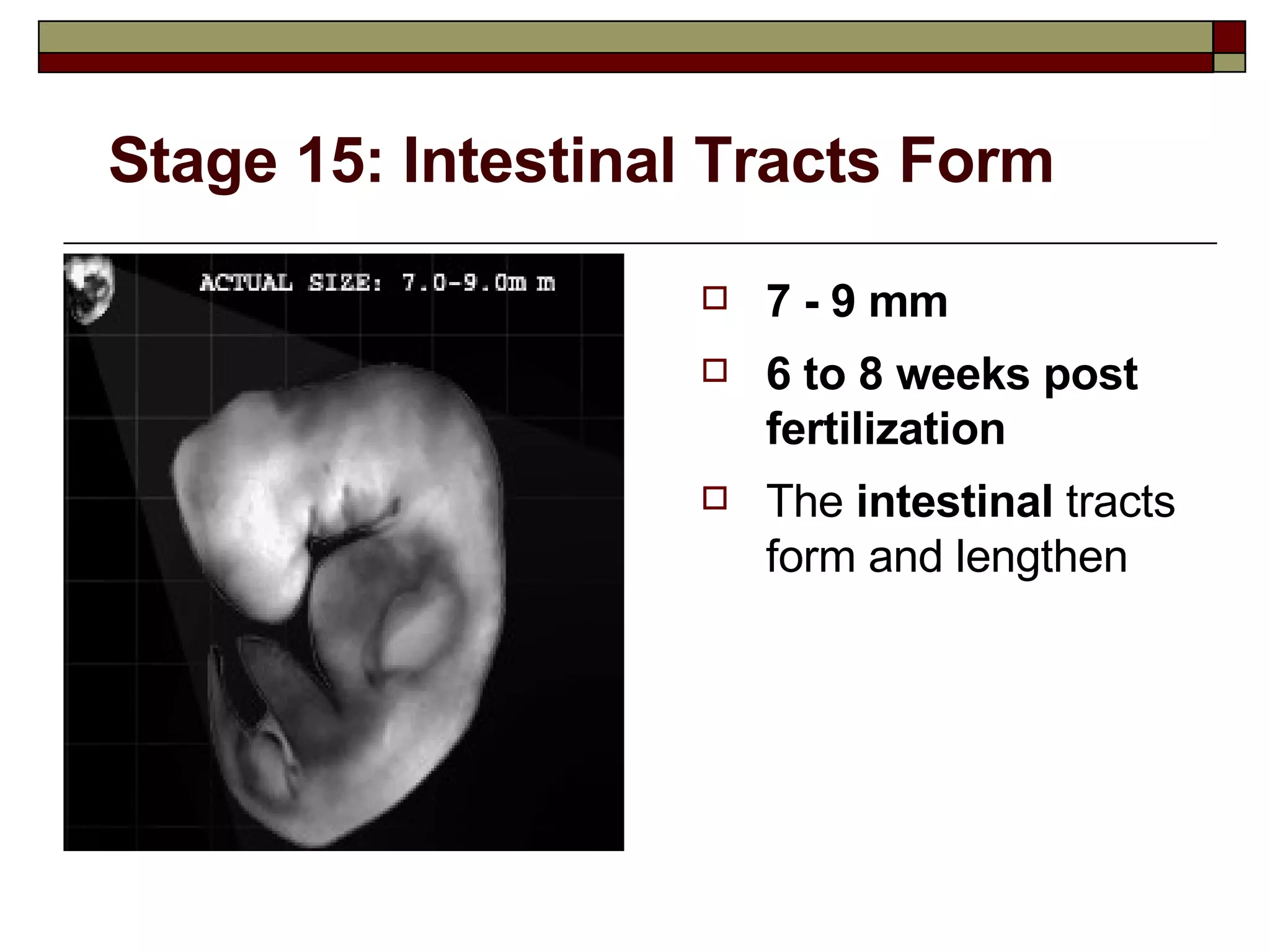
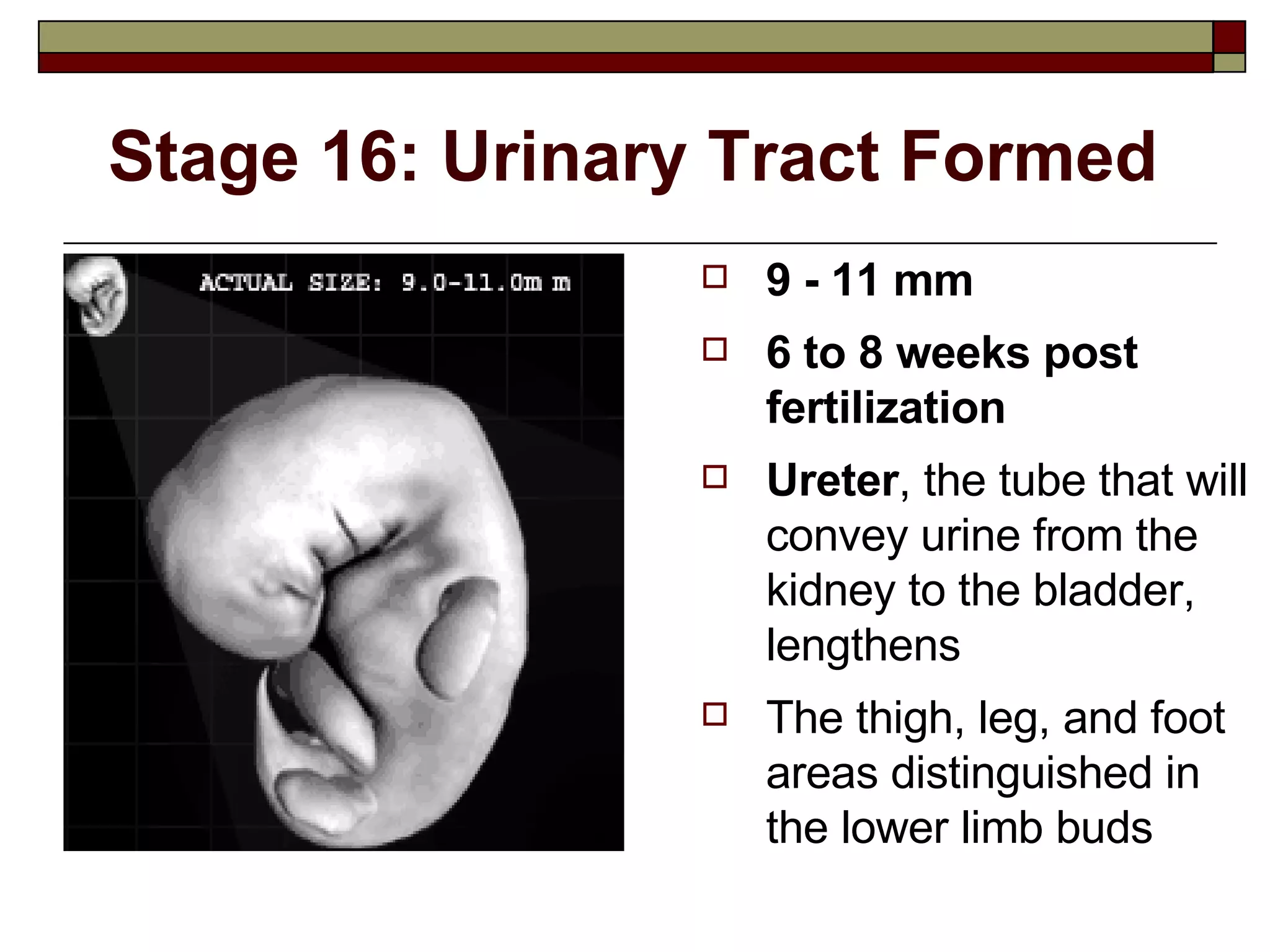
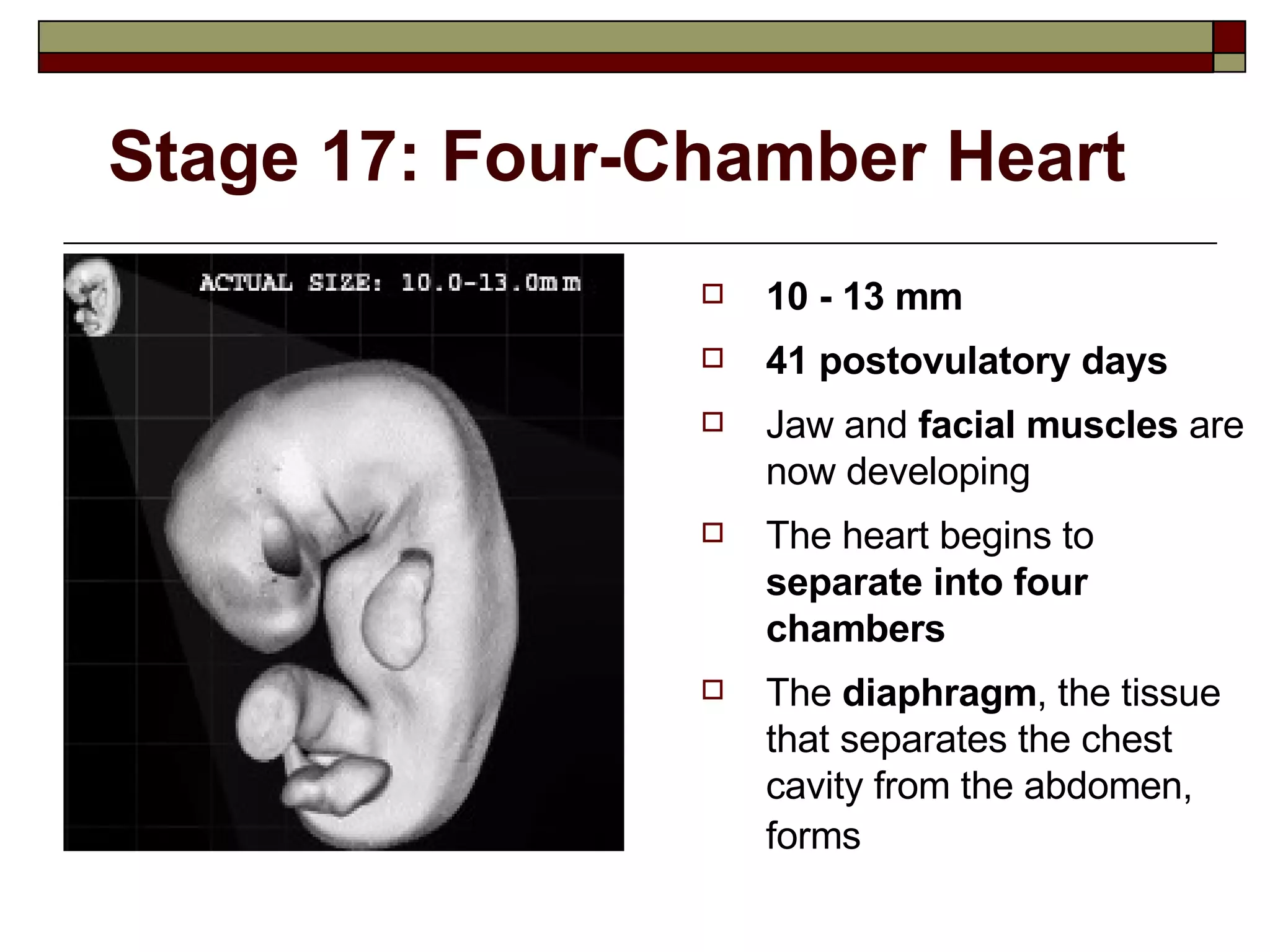
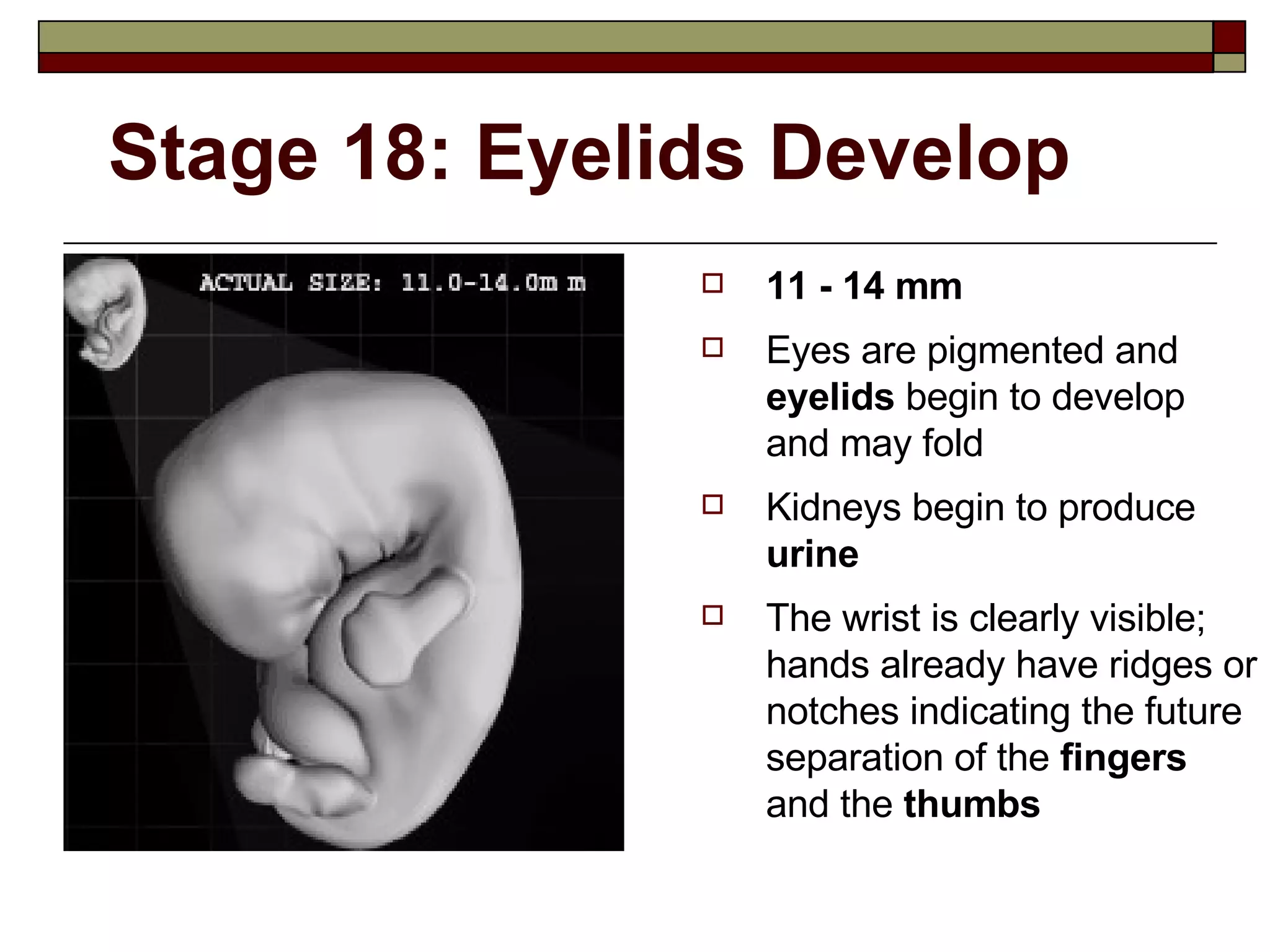
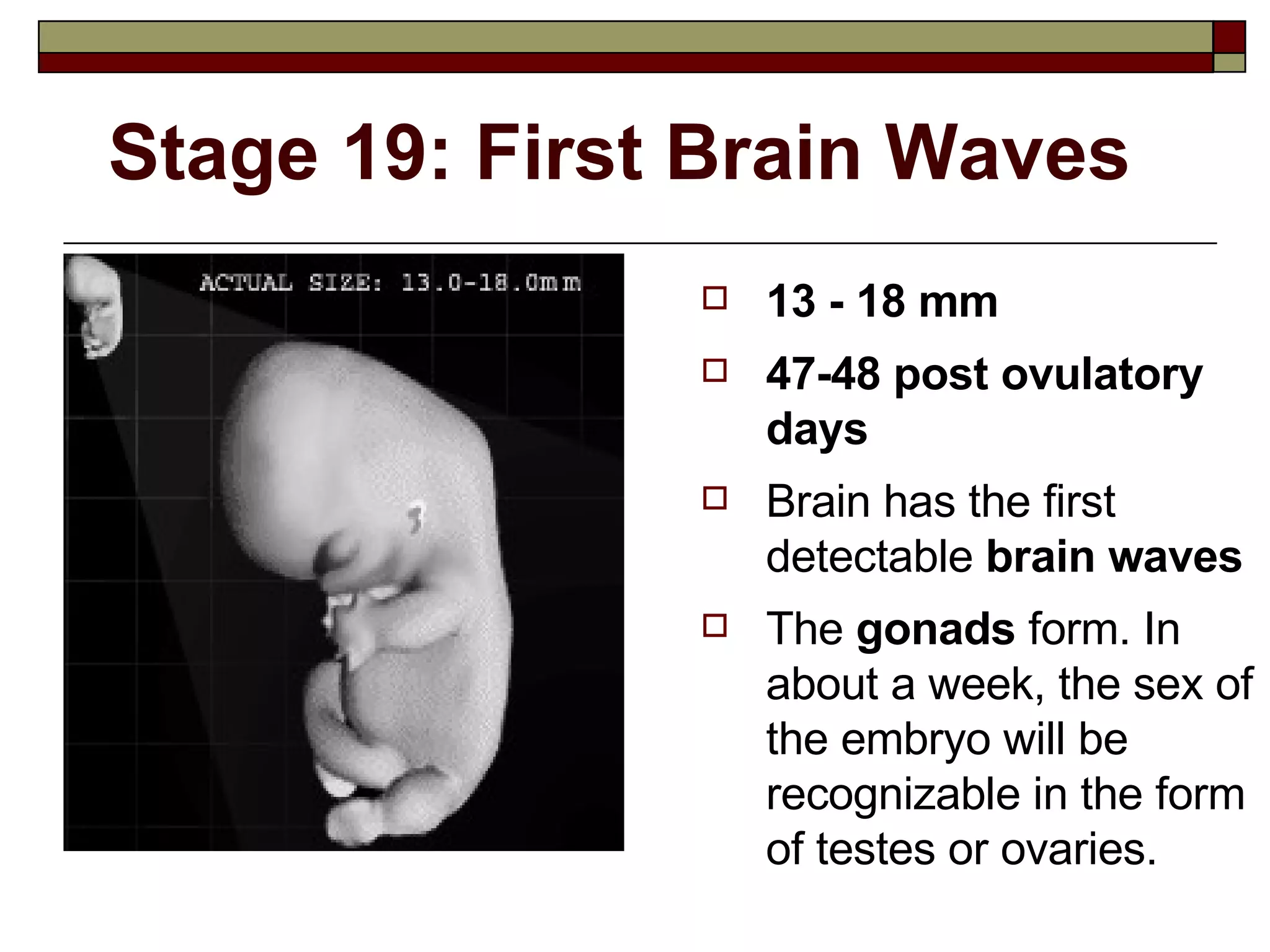
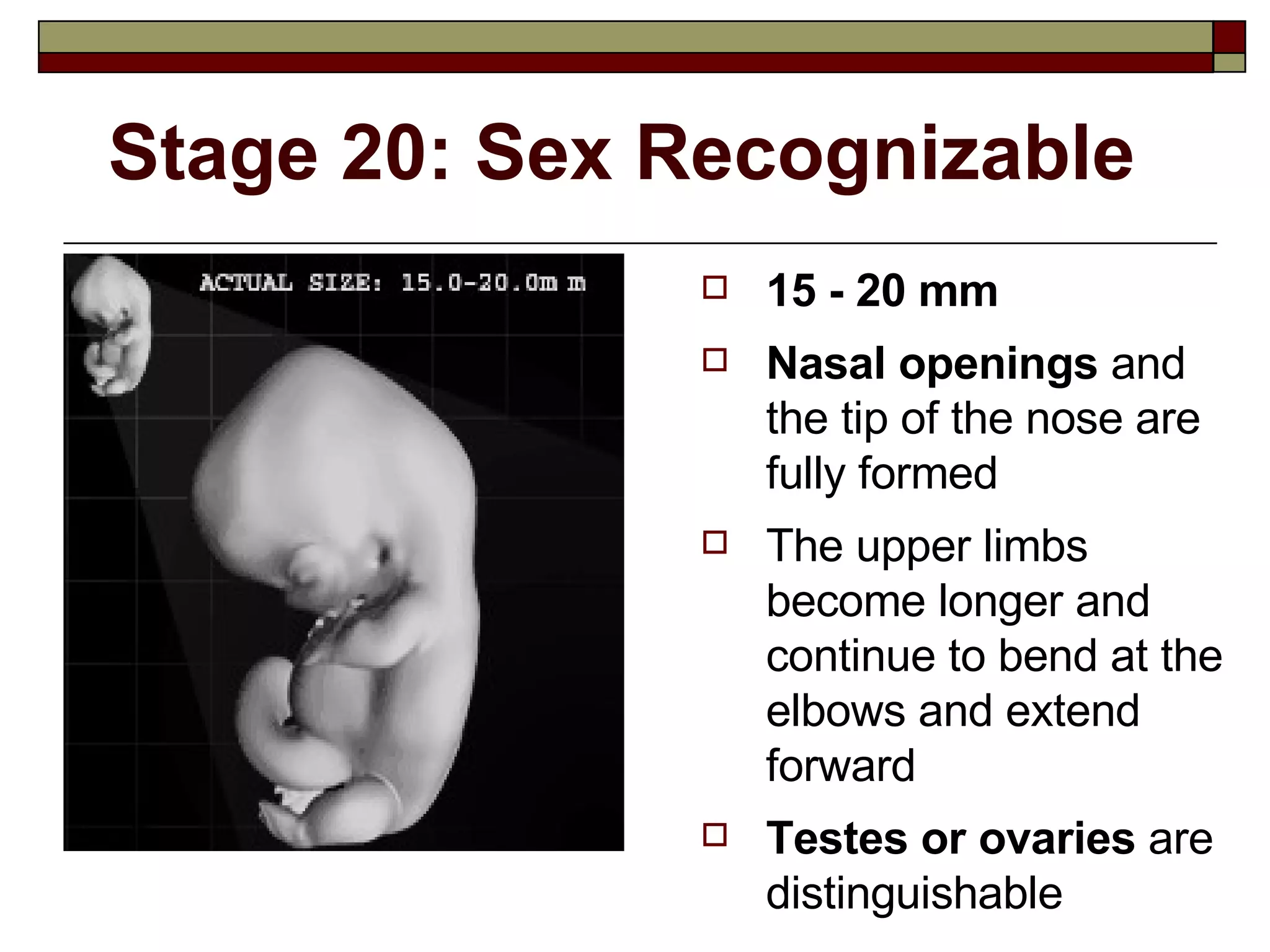
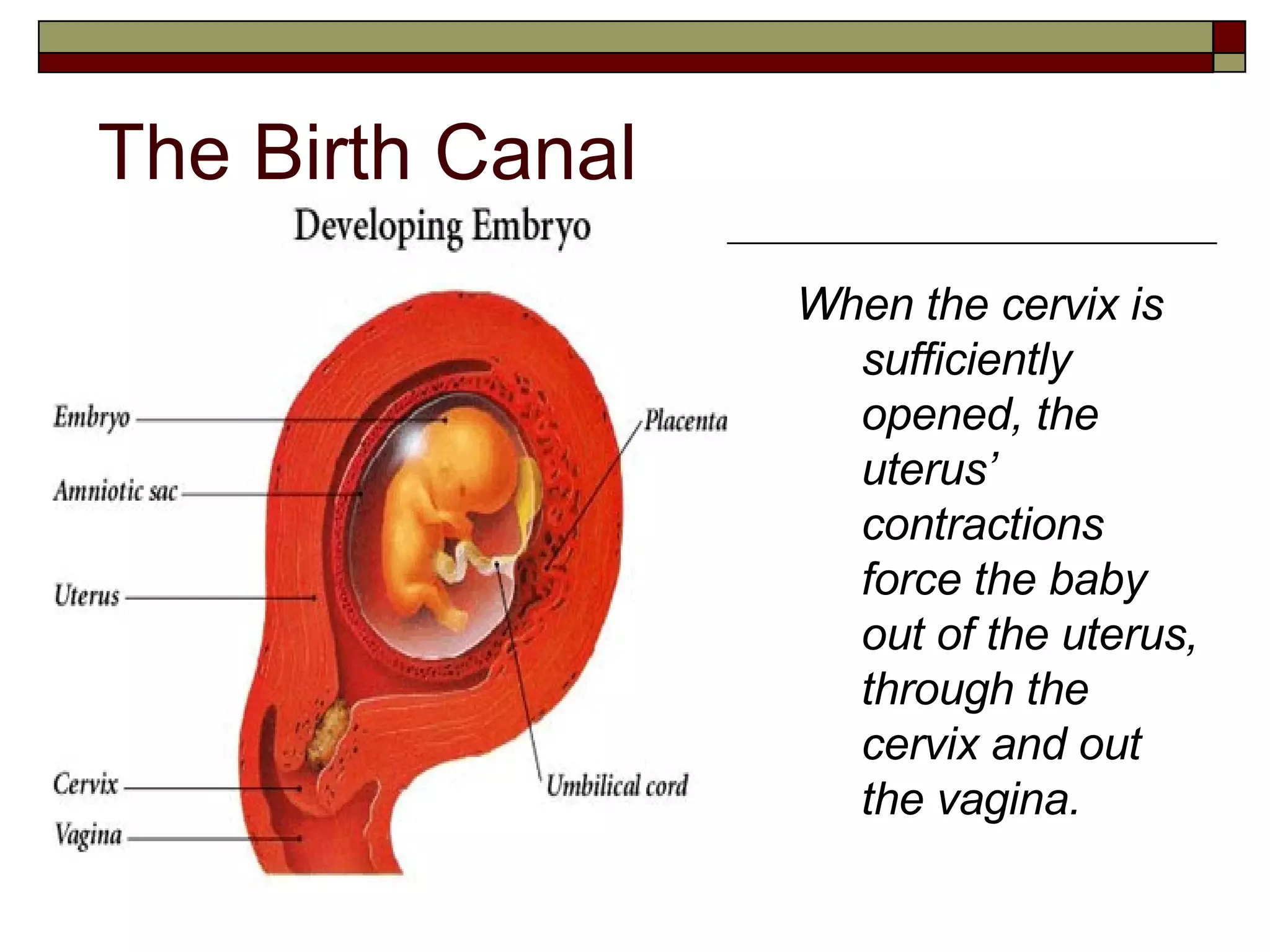
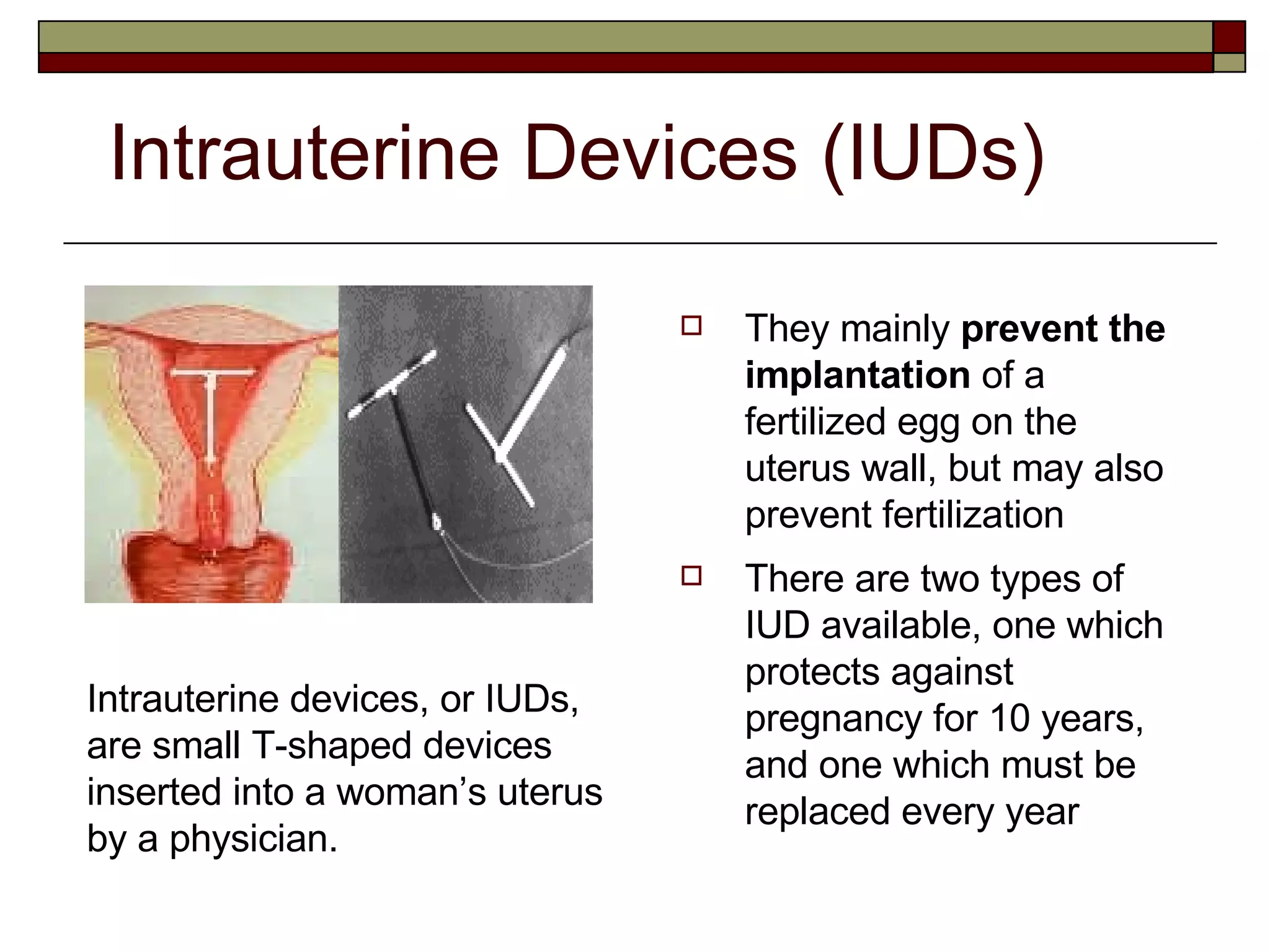
The document provides an overview of the male and female reproductive systems. It describes the gonads and gametes, how sperm and eggs are produced and transported, the hormones involved in reproduction, pregnancy and fetal development, and various methods of birth control and contraception.