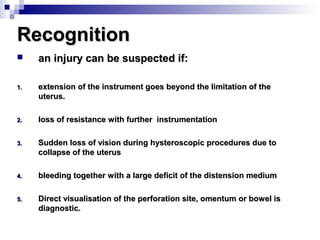
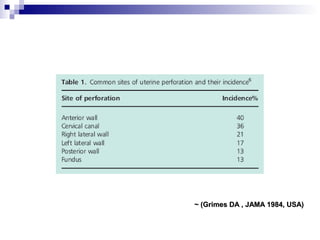
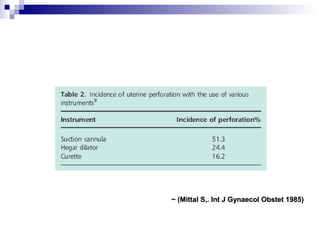
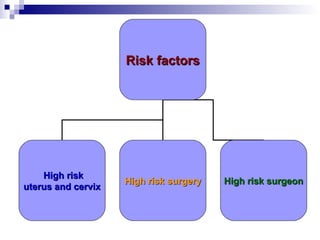
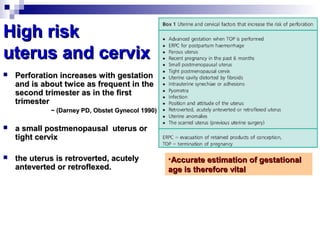
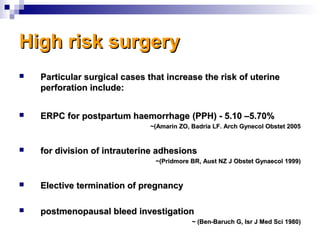
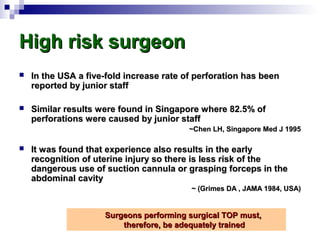
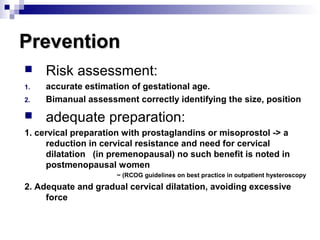
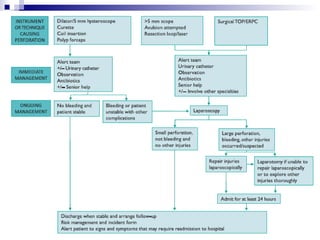
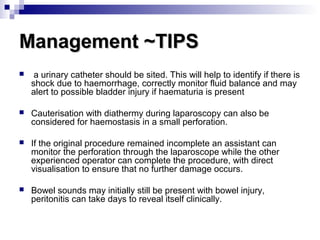
The document discusses uterine perforation, a potential complication of various gynecological procedures. It notes that termination of pregnancy is the most common associated procedure. Risk factors include uterine anomalies, infection, recent pregnancy, and postmenopause. Most perforations occur in the uterine body and cause little bleeding, but some can involve other organs. Prevention focuses on risk assessment, cervical preparation, and gradual dilation. Management tips include urinary catheterization, cauterization, and seeking help from senior physicians. Overall, uterine perforation is rare but can have serious consequences, so appropriate training and caution are important.