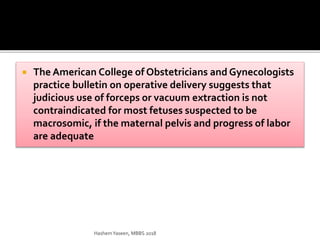
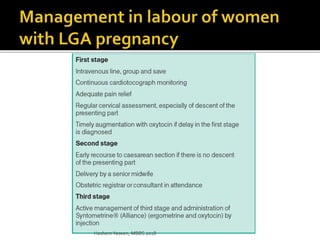
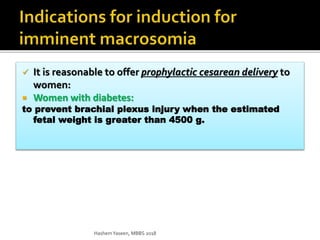
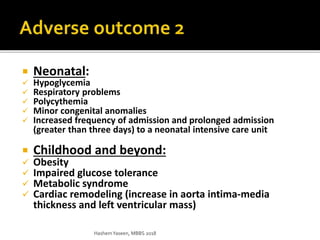
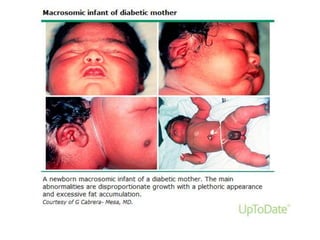
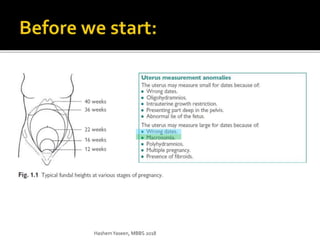
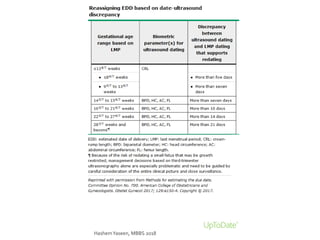
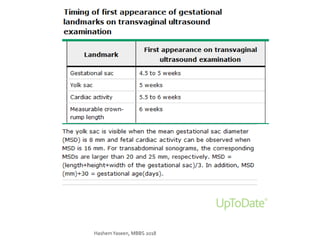
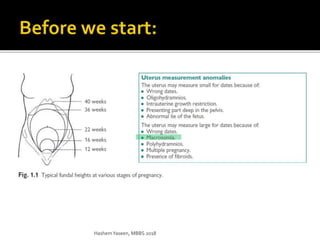
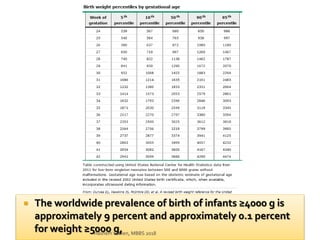
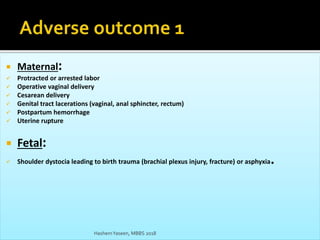
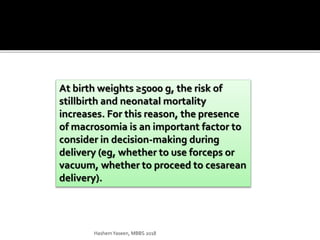
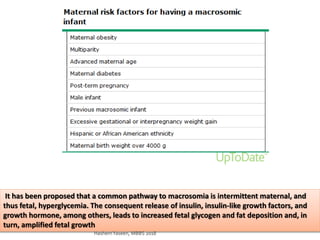
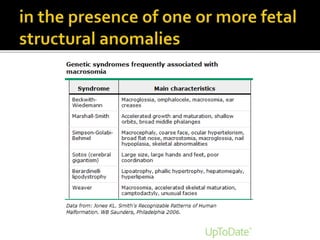
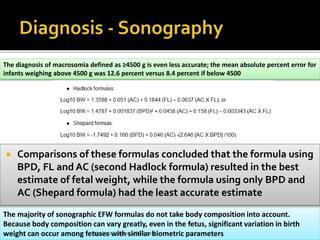
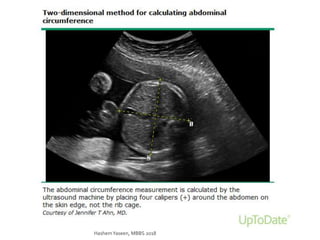
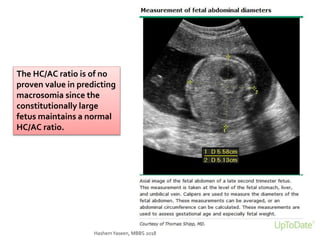
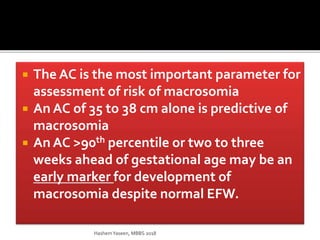
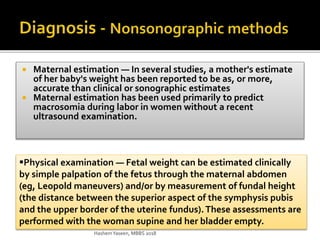
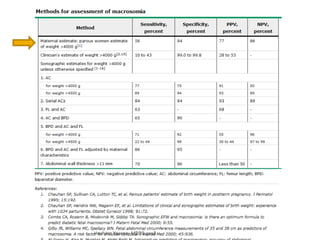
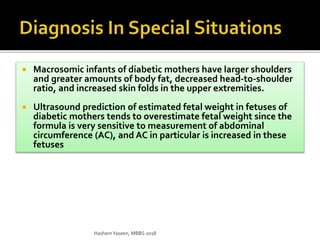
This document discusses macrosomia, which refers to infants with high birth weights, usually over 4000g or 9 pounds. Risks of macrosomia include difficult delivery and injuries. It reviews methods of predicting macrosomia like ultrasound measurements and maternal estimates. For infants over 4000g or 4500g, induction of labor at 39 weeks is recommended to reduce risks. For infants over 4500g born to diabetic mothers, cesarean delivery may help prevent injuries. The document provides details on evaluating and managing pregnancies at risk for a macrosomic infant.

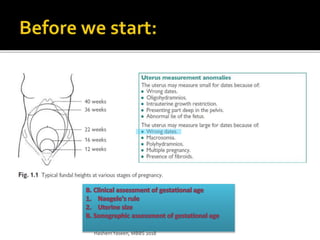


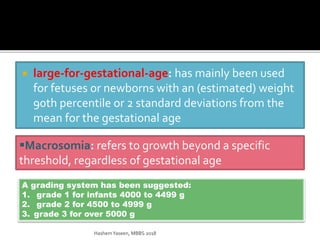

![ It is reasonable to offer elective induction of labor to
women:
Women without diabetes:
4000 and 4500 g -> at 39 weeks of gestation
Reduced the risk of neonatal fractures (relative risk [RR] 0.20, 95% CI 0.05-0.79)
Reduced the risk of shoulder dystocia (RR 0.60, 95% CI 0.37-0.98)
HashemYaseen, MBBS 2018](https://image.slidesharecdn.com/lgaseminarhashem2018-180314082032/85/LGA-seminar-hashem-2018-24-320.jpg)