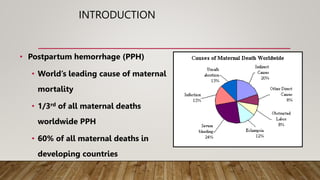
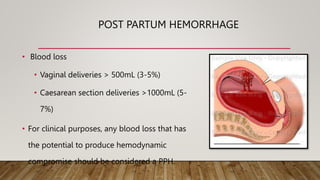
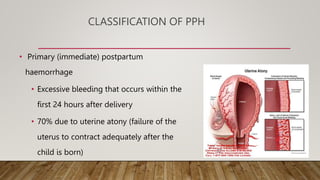
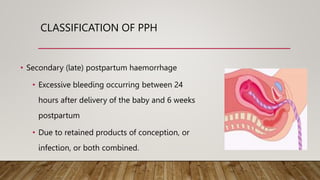
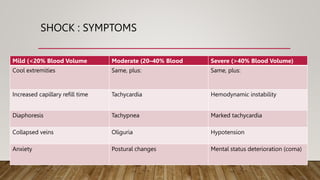
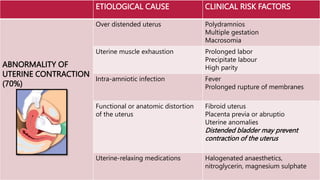
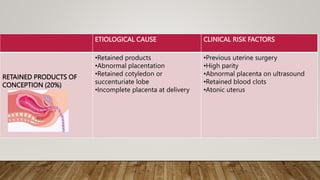
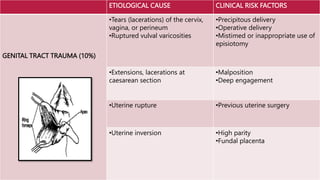
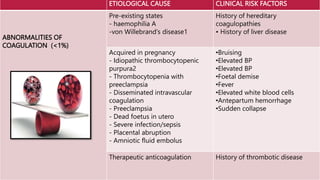
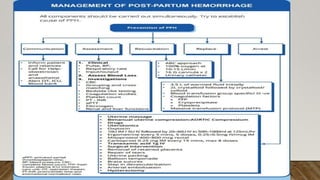
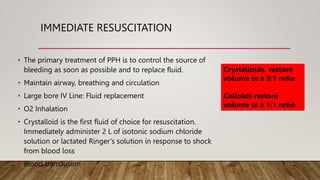
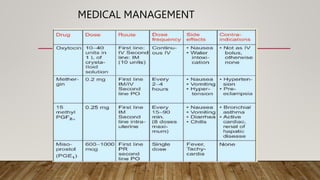
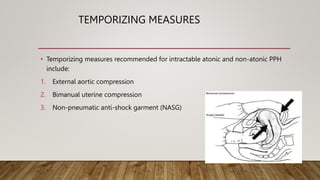
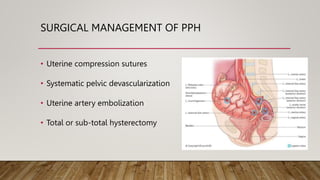
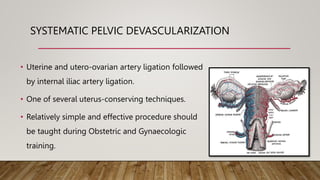
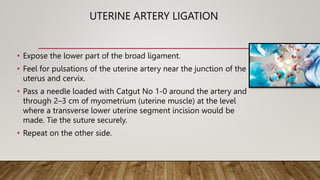
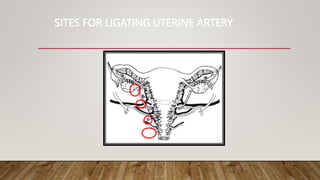
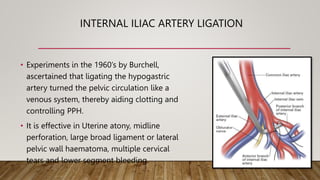
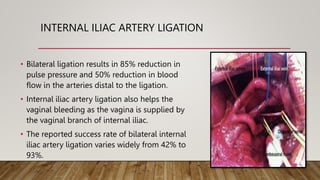
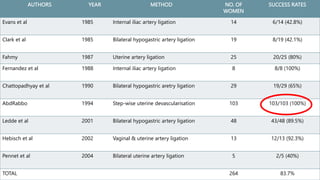
Postpartum hemorrhage (PPH) is a leading cause of maternal mortality, particularly in developing countries, with a significant number of deaths occurring shortly after delivery. The condition is classified into primary and secondary PPH, with various causes including uterine atony, retained products, and trauma. Management involves immediate resuscitation, medical interventions such as tranexamic acid, and surgical options like uterine artery ligation to effectively control the bleeding.