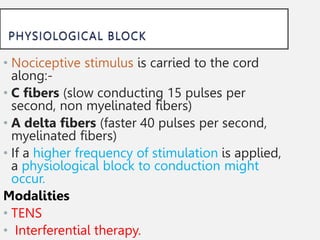
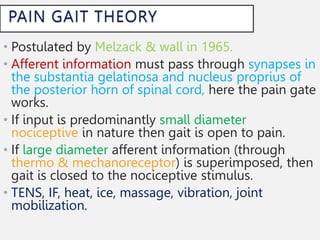
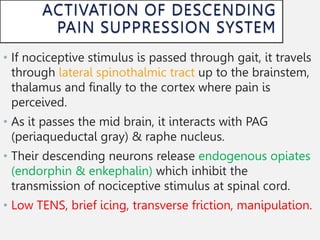
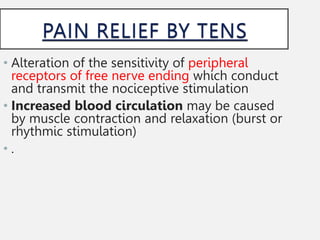
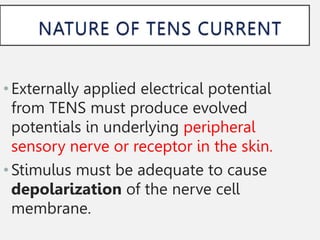
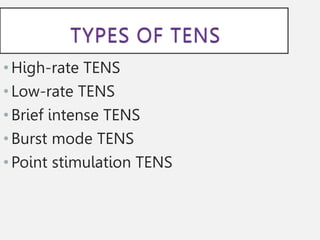
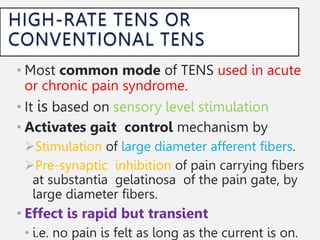
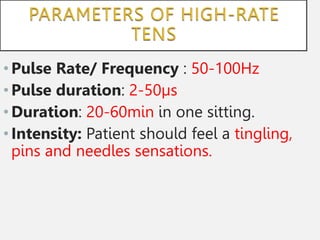
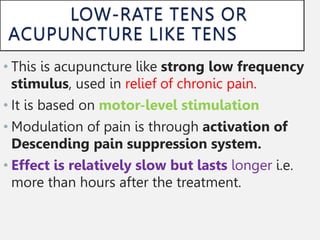
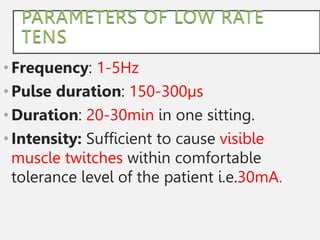
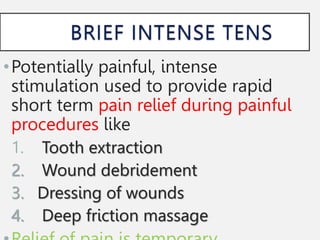
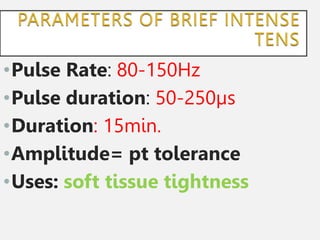
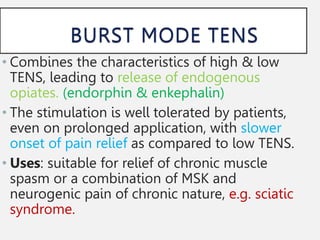
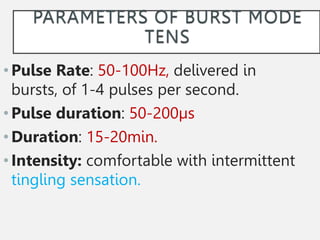
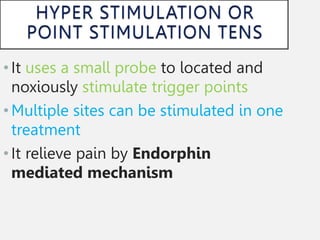
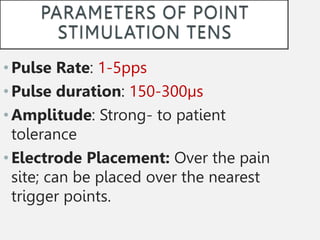
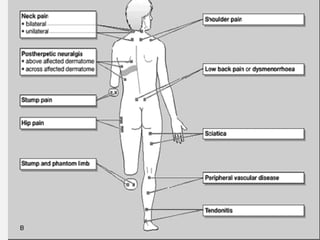
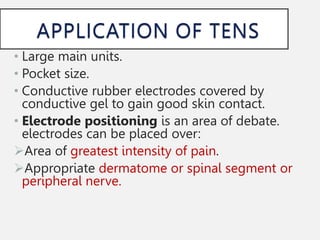
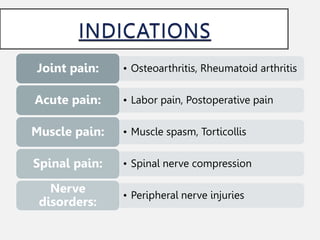
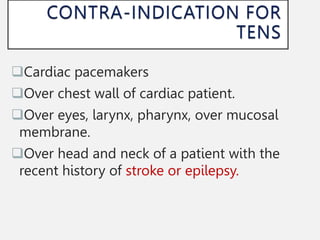
The document outlines Transcutaneous Electrical Nerve Stimulation (TENS) as a modern, non-invasive method for pain management, which utilizes electrical currents through skin electrodes to alleviate both acute and chronic pain. It explains different TENS modalities, their mechanisms, applications, and effectiveness, such as the activation of pain suppression systems and enhancement of local circulation. Additionally, it addresses proper electrode placement and contraindications for specific medical conditions.