The study evaluated the relationship between syntax score and lipid parameters, including lipoprotein (a), in 75 non-diabetic patients under 55 years with acute coronary syndrome. It found that higher syntax scores correlated with elevated levels of total cholesterol, non-HDL, and LDL, while no significant association was found between syntax scores and lipoprotein (a) levels. This indicates that while certain lipid profiles can indicate severity in coronary artery disease, lipoprotein (a) does not play a significant role in this context.
![Syntax Score and its Relation to Lipoprotein a –Lp (a) and Extended Lipid Parameters in Non-Diabetic Patients with Acute Coronary Syndrome Having Age below 55 Years
IJCCR
Syntax Score and its Relation to Lipoprotein a –Lp (a) and
Extended Lipid Parameters in Non-Diabetic Patients with Acute
Coronary Syndrome Having Age below 55 Years
*1Dr Tejas Shah (MD, DNB – Cardiology), 2Dr Chaitri Shah (MD Anaesthesiology), 3Dr Jasmin
Jasani (MD Pathology), 4Dr JD Lakhani (MD Medicine), 5Mr. Ronak Shah (M.Sc Clinical
Research)
1Assistant Professor, Department of Cardiology, Sumandeep Vidyapeeth, At & Po Piparia, Ta. Waghodia, Vadodara
391760, Gujarat, India
2,3,4Professor, Sumandeep Vidyapeeth, At & Po Piparia, Ta. Waghodia, Vadodara 391760, Gujarat, India
5Research Assistant, Sumandeep Vidyapeeth, At & Po Piparia, Ta. Waghodia, Vadodara 391760, Gujarat, India
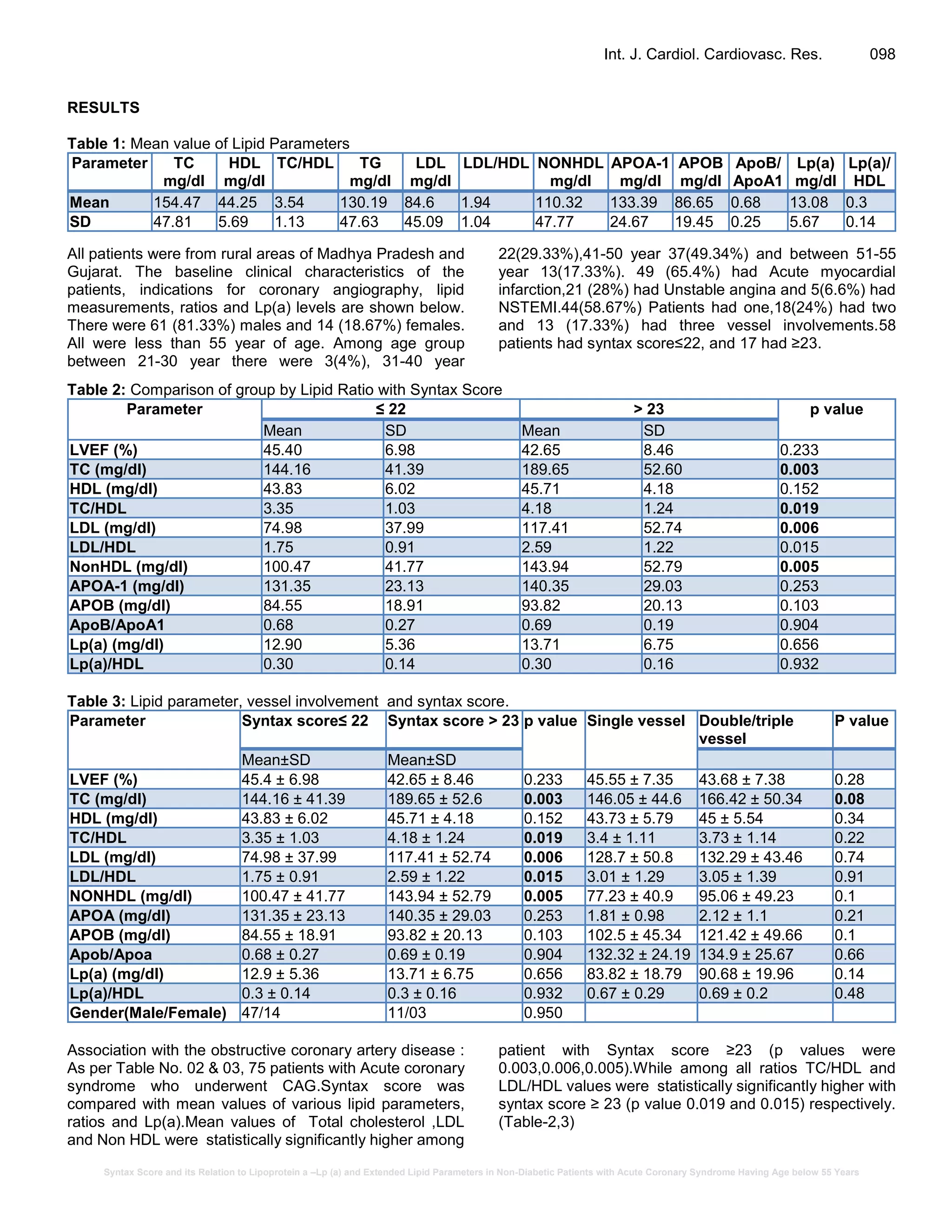
Syntax score is a semi-quantitative visual grading system for complex coronary artery disease
based on angiography findings. We investigated whether the severity of coronary artery disease
(Syntax score) correlates with Lipoprotein (a) {Lp (a)} value and lipid ratios.75 non-diabetic adult
patients, having age below 55 years, who presented with Acute Coronary Syndrome (ACS) were
included. Coronary angiography and Syntax Score calculation was done. Various lipid ratios and
Lp(a) were correlated with syntax score. Out of 75 patients ,61 (81.33%) were males and 14
(18.67%) females, having mean age of 44.37years. Majority (49.34%) having age between 41-50
years. Those 49 (65.4%) had acute myocardial infarction,21 (28%) had unstable angina and 5(6.6%)
had Non-ST-elevation myocardial infarction (NSTEMI). 44(58.67%) patients had one, 18(24%) had
two and 13 (17.33%) had three vessels disease.58 (77.33%) had syntax score ≤22 and 17 (26.67%)
had ≥ 23. Statistically significant difference (p < 0.05) was found in mean values of Total
cholesterol (TC), TC/HDL ratio, LDL, LDL/HDL and Non-HDL cholesterol in patients having syntax
score> 23. Mean values of other parameters like LVEF(Left ventricular ejection fraction),ApoA-1
,Apo B, Apo B/Apo A, Lp(a)/HDL did not differ in two groups. Lp(a) lipoprotein levels did not show
any association with the syntax score and extent of coronary artery disease. This study of western
Indian young non-diabetic patients having acute coronary syndrome found association of syntax
score with high non-HDL, TC, TC/HDL, LDL, LDL/HDL values. It was not correlating with LP (a)
levels.
Key Words: Syntax score, Lipid ratio, Lipoprotein, Acute Coronary Syndrome
INTRODUCTION
To quantify severity and extent of coronary artery disease
(CAD), SYNTAX (Synergy Between PCI With Taxus and
Cardiac Surgery) score was developed. This score was
used in SYNTAX trial which has shown ability to predict
adverse ischemic events in patients undergoing
percutaneous coronary intervention (PCI) [Mayank et al.,
2013]
Lipoprotein (a) [Lp(a)] is a plasma lipoprotein which
consists of elements; a central low-density lipoprotein
(LDL)-like core containing a single of apolipoprotein B100
(apoB) linked by a disulfide bridge to a signature protein
called apolipoprotein(a) [apo(a)] which is similar structure
wise to Plasminogen. [BERG K et al., 1963] It competes
with plasminogen for its binding site, leading to reduced
fibrinolysis, and as a result of the stimulation of secretion
*Corresponding Author: Dr Tejas Shah, Assistant
Professor, Department of Cardiology, Sumandeep
Vidyapeeth, At & Po Piparia, Ta. Waghodia, Vadodara
391760, Gujarat, India.
E-mail: tejaschaitri@gmail.com; Tel: +91 8951274202
Research Article
Vol. 5(2), pp. 096-102, June, 2019. © www.premierpublishers.org, ISSN: 3102-9869
International Journal of Cardiology and Cardiovascular Research](https://image.slidesharecdn.com/pdf-190610041739/75/Syntax-Score-and-its-Relation-to-Lipoprotein-a-Lp-a-and-Extended-Lipid-Parameters-in-Non-Diabetic-Patients-with-Acute-Coronary-Syndrome-Having-Age-below-55-Years-1-2048.jpg)
![Syntax Score and its Relation to Lipoprotein a –Lp (a) and Extended Lipid Parameters in Non-Diabetic Patients with Acute Coronary Syndrome Having Age below 55 Years
Shah et al. 097
of plasminogen activator inhibitor-1, Lp(a) leads to
thrombogenesis. [Danesh et al., 2000, Bennet et al., 2008,
Clayton et al., 2001, Kamstrup et al., 2009, Clarke et al.,
2009]. Lp(a) has found as a important risk factor for CVD
(Cardiovascular disease) including myocardial infarction
and valvular heart disease ie aortic stenosis. In addition to
the role of high Lp(a) levels in various vascular diseases,
low concentrations also seem to be important in vascular
medicine [Kotani K et al., 2012].Some authors have
suggested the existence of a J-curved phenomenon for
Lp(a)concentration with a slight increase of cardiovascular
andcerebrovascular outcomes in the group of patients with
verylow levels and a larger increase in the group of
patients with significantly increased Lp(a) levels.For
example decreased values of Lp(a) have been associated
with carotid atherosclerosis and have been proposed as
markers of cerebral hemorrhage risk. Thereare several
hypotheses relating to this phenomenon: oneassociated
with the induction of angionecrosis and impaired nutritional
metabolism within the vessels, another with theimpaired
metabolism of scavenging oxidized lipids. [Ishikawa S et
al.,2013]
The aim of the study was to evaluate, in judging the
severity of coronary artery disease, the association
between the level of Lp(a) and various lipid parameters.
METHODS
Study design
This was a cross sectional study in which we enrolled a
total of 75 consecutive patients with ACS, 18 to 55 years
of age, who underwent coronary angiography at
Department of cardiology, Dhiraj General Hospital,
Sumandeep Vidyapeeth between Feb-2017 to June-2018.
Patients who had history of Hypothyroidism, Chronic Liver
& Kidney Disease, Diabetes Mellitus and patients who
were on lipid lowering agents were excluded from the
study. For female patients we have enrolled only non
pregnant and non lactating women.
The study was approved by the Institutional Ethics
Committee, and all patients gave written informed consent.
Angiographic analysis:
Key angiographic features of syntax scoring system
include
- Right or Left dominant system
- Number of artery segments involved per atherosclerotic
lesion.
- Total occlusion:
a) Number of segments involved
b) Age of total occlusion
c) Presence of blunt stump
d) Presence of bridging collaterals
e) Antegrade vs retrograde filling of the first segment
beyond the occlusion.
f) Side branch involvement
- Trifurcation lesion: number of vessel segments
diseased
- Bifurcation lesion: angulation between the distal
main vessel and the side branch <700
- Presence of an aorto-ostial atherosclerotic lesion
- Presence of severe vessel tortuosity at lesion site
- Atherosclerotic lesion length>20 mm
- Presence of heavily calcified plaque
- Presence of thrombus
- Presence of diffuse or small vessel disease
The maximal stenosis in each of 27 coronary-artery
segments was assessed by a cardiologist.“According to
that, Syntax score(On line version 2.28) was calculated
.The score was divided into ≤22 and ≥23.The extent of
angiographically documented coronary artery disease was
quantified as follows: normal coronary arteries (with either
no stenosis or a stenosis of <10 percent of the luminal
diameter), mild disease (a stenosis of 10 to 50 percent of
the luminal diameter in one or more coronary arteries or
their major branches), or one vessel and more than one
vessel ie two or three-vessel disease, defined as a
stenosis of more than 50 percent of the luminal diameter
in one, two, or three coronary arteries or their major
branches.
Laboratory Analyses
For Acute MI patient venous sample was taken in less than
one hour and for other patients, fasting (>12 hour) venous
samples were obtained. Various Extended lipid values
were measured from sample, with Erba EM 200 Analyser.
Normal values for lipid profile which is established at our
institutional laboratory was taken as reference values
:Total cholesterol (TC)-<200 mg/dl, Triglyceride(TG)<160
mg/dl, High Density Lipoprotein(HDL)30-60 mg/dl, Low
Density Lipoprotein(LDL)-<110 mg/dl, Very Low Density
Lipoprotein(VLDL)-<32 mg/dl, Apo A-1 105-205 mg/dl,
Apo B-40-125 mg/dl and Lp(a) <30 mg/dl. Quantitative
determination of Lipoprotein (a) was performed with
turbidimetric immunoassay. LDL cholesterol was
estimated with the use of the Friedewald formula. Non-
HDL cholesterol was measured from Total cholesterol
minus HDL. Various lipid ratios like TC/HDL, LDL/HDL,
Apob/Apoa-1, TG/HDL and Lp(a)/HDL were calculated.
Statistical Analysis
Discrete data are presented as frequencies and
percentages, and continuous variables as mean and
standard deviation. Independent t test was used to find
significant mean difference of various lipid parameters
between two groups. Chi square test was used to find
association between two variables. P value < 0.05 has
been considered as significant value.](https://image.slidesharecdn.com/pdf-190610041739/75/Syntax-Score-and-its-Relation-to-Lipoprotein-a-Lp-a-and-Extended-Lipid-Parameters-in-Non-Diabetic-Patients-with-Acute-Coronary-Syndrome-Having-Age-below-55-Years-2-2048.jpg)
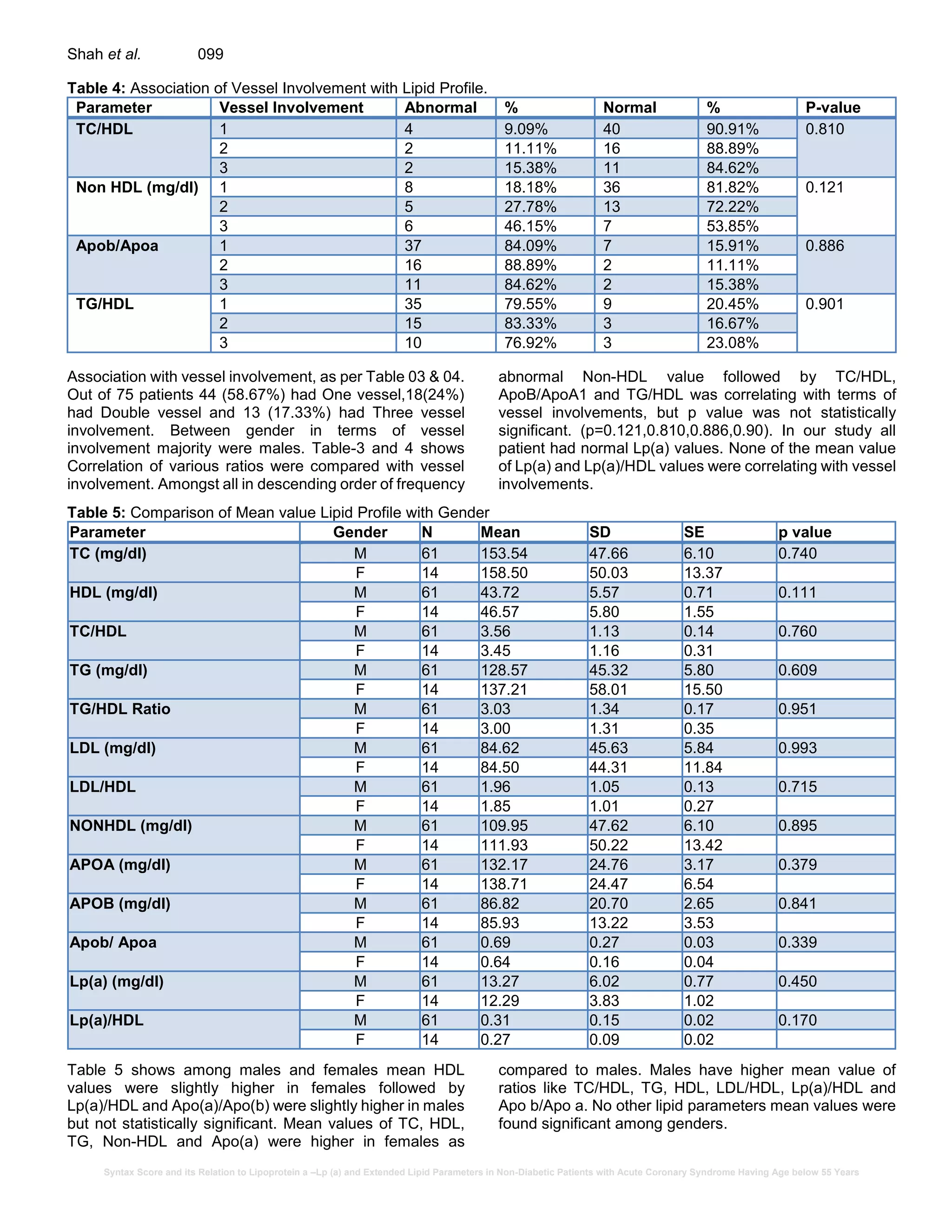
![Syntax Score and its Relation to Lipoprotein a –Lp (a) and Extended Lipid Parameters in Non-Diabetic Patients with Acute Coronary Syndrome Having Age below 55 Years
Int. J. Cardiol. Cardiovasc. Res. 100
DISCUSSION
In our study, ACS patients having age < 55 years with high
syntax score (≥ 23) had elevated lipid parameters like Total
cholesterol, TC/HDL ratio, LDL, LDL/HDL ratio and Non-
HDL. Irrespective of syntax score, i.e. Low or high Lp(a)
was not elevated in our ACS patients.
The extent of coronary disease affects clinical outcomes
and may predict the effectiveness of coronary
revascularization with either coronary artery bypass graft
(CABG) surgery or percutaneous coronary intervention
(PCI). The SYNTAX (Synergy Between Percutaneous
Coronary Intervention with Taxus and Cardiac Surgery)
score quantifies the extent of coronary disease. The
SYNTAX score was designed to predict outcomes related
to anatomical characteristics and, to a lesser extent, the
functional risk of occlusion for any segment of the
coronary-artery bed.
Human coronary atherosclerosis is a chronic inflammatory
disease that issuperimposed on a background of lipid
abnormalities. The Total cholesterol/High-density
lipoprotein (HDL) cholesterol ratio, known as the
atherogenic or Castelli index and the LDL/HDL cholesterol
ratio are two important components and indicators of
vascular risk, the predictive value of which is greater than
the isolated parameters. An increase in Total cholesterol
concentration, and specifically LDL cholesterol, is an
atherogenic lipid marker.[Ascaso J et al., 2007] When
Total cholesterol, HDL cholesterol, and Total/HDL
cholesterol ratio are compared between an apparently
healthy population and myocardial infarction survivors, the
Total/HDL cholesterol ratio is found to present less
superposition of populations.This illustrates the high
discriminatory power for coronary heart disease presented
by the Total/HDL cholesterol ratio, as well as its great
predictive capacity.
The LDL/HDL cholesterol ratio appears to be as useful as
the Total/HDL cholesterol ratio. Their similarity can be
explained by the fact that approximately two thirds of
plasma cholesterol are found in LDL and, Total and LDL
cholesterol are closely related. Like the Total/HDL
cholesterol ratio, LDL/HDL cholesterol may have more
predictive power if hypertriglyceridemia is taken into
account. Although, the increase in these ratios predicted a
greater cardiovascular risk in a wide range of cholesterol
or triglyceride concentrations, the risk is significantly
higher when hypertriglyceridemia is present, as shown by
the Helsinki Heart Study.[ Manninen V et al., 1992] when
there is no reliable calculation of LDL cholesterol, as when
triglyceridemia exceeds 300mg/dL (3.36 mmol/L), it is
preferable to use the Total/HDL cholesterol ratio. So
individuals with a high Total/HDL cholesterol or LDL/HDL
cholesterol ratio have greater cardiovascular risk due to
an increase in the atherogenic component contained in the
numerator, a decrease in the anti-atherosclerotic trait of
the denominator, or both.[Criqui MH et al., 1998]
ApoB/ApoA-I ratio
Apolipoprotein (apo) B represents most of the protein
content in LDL and intermediate-density lipoproteins (IDL)
and VLDL. ApoA-I is the principal apolipoprotein in HDL.
Both apolipoproteins, therefore, separately provide
information for detecting high-risk individuals. ApoA-I is
also believed to be a more reliable parameter for
measuring HDL than cholesterol content since it is not
subject to variation. Therefore, the apoB/apoA-I ratio is
also highly valuable for detecting atherogenic risk, and
there is currently sufficient evidence to demonstrate that it
is better for estimating vascular risk than the Total/HDL
cholesterol ratio. [Walldius et al 2004, Sniderman AD et al.,
2006, Wallidius G et al., 2006, Holme I et al.,2008] The
greater the ApoB/ApoA-I ratio, the larger will be the
amount of cholesterol from atherogenic lipoproteins
circulating through the plasma compartment and likely to
induce endothelial dysfunction and trigger the atherogenic
process. On the other hand, a lower ApoB/ApoA-I ratio will
lead to less vascular aggression by plasma cholesterol
and increased and more effective reverse transport of
cholesterol, as well as other beneficial effects, thereby
reducing the risk of cardiovascular disease.
The association between triglycerides and HDL
cholesterol reflected by this ratio (TG/HDL) depicts the
balance between atherogenic and protective lipoproteins.
Known as the atherogenic plasma index, it shows a
positive correlation with the HDL esterification rate
(FERHDL) and an inverse correlation with LDL size.
[Dobiásová M et al., 2001] Hypoalphalipoproteinemia and
hypertriglyceridemia both induce an increase in the
percentage of small HDL and small, dense LDL particles.
Ultimately, the simultaneous use of triglycerides and HDL
cholesterol in this ratio reflects the complex interactions of
lipoprotein metabolism overall and can be useful for
predicting plasma atherogenicity.[ Dobiásová M et al.,
2004] An atherogenic plasma index [log (triglycerides/HDL
cholesterol)] over 0.5 has been proposed as the cut-off
point indicating atherogenic risk.[ Dobiásová M et al.,
2001]
Non-HDL cholesterol
Non-HDL cholesterol, which is total cholesterol minus HDL
cholesterol, is a measure of the cholesterol in LDL, IDL and
VLDL particles. Non-HDL cholesterol has been
recommended as a secondary therapeutic target in
individuals with high triglyceride concentration, and it has
been suggested that it could be a surrogate marker of
serum apoB concentration. However, non-HDL cholesterol
is not always strongly associated with apoB, particularly in
the presence of hypertriglyceridemia. [Sniderman AD et
al., 2003] In patients with elevated TG levels (200-499
mg/dL), treatment of the non-HDL-C level is a secondary
target after the LDL-C target has been reached.](https://image.slidesharecdn.com/pdf-190610041739/75/Syntax-Score-and-its-Relation-to-Lipoprotein-a-Lp-a-and-Extended-Lipid-Parameters-in-Non-Diabetic-Patients-with-Acute-Coronary-Syndrome-Having-Age-below-55-Years-5-2048.jpg)
![Syntax Score and its Relation to Lipoprotein a –Lp (a) and Extended Lipid Parameters in Non-Diabetic Patients with Acute Coronary Syndrome Having Age below 55 Years
Shah et al. 101
Lp(a)
The study [Afshar M et al., 2016] verified the current
recommendations for Lp(a)and suggested that treatment
should focus on the control ofother risk factors first,
including lowering LDL-C, andassumed that identifying
interactions between Lp(a) and other risk factors could
identify individuals at increased risk for Lp(a)-mediated
disease. There was higher prevalence of elevated Lp(a)
levels (>50 mg/dL) in study participants as compared to
the general population. Young ACS patients (<55 years),
high Lp(a) was strongly associated with high LDL-C levels,
and Lp(a) confers greater risk forpremature ACS when
LDL-C is elevated. [Afshar et al. 2016] This study clearly
confirms that elevated Lp(a) might often be present in
relatively young individuals without any other important
risk factors. Lp(a) and LDL-Care strongly associated in
young ACS individuals suggest that Lp(a) excess may
promote initiation and early development ofatheromatous
plaques, which may be accelerated by the presence of a
high level of LDL-C (especially above 3.5 mmol/L).
[Sniderman AD et al., 2003]
Study conducted by Dr Ashfaq F. et al from North India
found significant correlation of Lp(a) value with syntax
score and vessel involvement.[ Fauzia Ashfaq et al., 2012]
While Recent study publish in JACC by Nancy et al
concluded that Lp(a) was associated with CVD only
among those with high TC and improvement in prediction
was minimal particularly in women.[ Nancy R et al., 2018]
Study conducted by Sotirios Tsimikas et al, which was
published in NEJM 2005 [Sotirios Tsimikas et al., 2005]
showed High Lp(a) with oxidized phospholipid of LDL with
significant coronary artery disease with age less than 60.
The guidelines have recommended Lp(a)measurement to
be done in patients having pre mature CAD, high
cholesterol level especially females as well as in cases
having family history of CAD. Though we recommend
broad base study to find out association between Lp(a)
levels and severity as well as extent of coronary artery
disease in patients with/without comorbidities, our study
found normal Lp(a) levels in our non diabetic CAD patients
who were below 55 years of age.
CONCLUSION
LDL cholesterol is the main risk factor for cardiovascular
disease. It should be measured in patient with CAD. In our
population with syntax score ≥23both ratios TC/HDL and
LDL/HDL were higher. Though in our study higher syntax
score i.e. ≥ 23 was associated with higher mean TC, Non-
HDL and LDL values but Lp(a) was relatively normal in all
population. Lp(a) was not able to predict severityof
coronary artery disease.
STUDY LIMITATIONS
Sample size is very small. No control population was
taken.
REFERENCES
Afshar M, Pilote L, Dufresne L, Engert JC, Thanassoulis
G. Lipoprotein(a) interactions with low-density
lipoprotein cholesterol and other cardiovascular risk
factors in premature acute coronary syndrome (ACS).
J Am Heart Assoc.2016;5:e003012 doi:
10.1161/JAHA.115.003012.
Ascaso J, González Santos P, Hernández Mijares A, et al.
Management of dyslipidemia in the metabolic
syndrome. Recommendations of the Spanish HDL
Forum. Am J Cardiovasc Drugs. 2007;7:39–58.
Bennet, A., E. Di Angelantonio, S. Erqou, G. Eiriksdottir,
G. Sigurdsson, M. Woodward, A. Rumley, G. D. O.
Lowe, J. Danesh, and V. Gudnason.. Lipoprotein(a)
levels and risk of future coronary heart disease: large-
scale prospective data. Arch Intern Med. 2008 Mar
24;168(6):598-608.
BERG K. A NEW SERUM TYPE SYSTEM IN MAN—THE
LP SYSTEM. Acta Pathol Microbiol Scand. 1963; 59:
369-82.
Clarke, R., J. F. Peden, J. C. Hopewell, T. Kyriakou, A.
Goel, S. C. Heath, S. Parish, S. Barlera, M. G. Franzosi,
S. Rust, D. Bennett, A. Silveira, A. Malarstig, F. R.
Green, M. Lathrop, B. Gigante, K. Leander, U. De Faire,
U. Seedorf, A. Hamsten, R. Collins, H. Watkins, M.
Farrall, and PROCARDIS Consortium. Genetic variants
associated with Lp(a) lipoprotein level and coronary
diseaseNEngl J Med. 2009 Dec 24;361(26):2518-28.
Clayton, D., and P. M. McKeigue. Epidemiological
methods for studying genes and environmental factors
in complex diseases. Lancet. 2001 Oct 20; 358 (9290):
1356-60.
Criqui MH, Golom BA. Epidemiologic aspects of lipid
abnormalities. Am J Med. 1998;105(Suppl 1A):48S–
57S.
Danesh, J., R. Collins, and R. Peto. Lipoprotein(a) and
coronary heart disease. Meta-analysis of prospective
studies. Circulation. 2000 Sep 5;102(10):1082-5.
Dobiásová M, Frohlich J. The plasma parameter log
(TG/HDL-C) as an atherogenic index: correlation with
lipoprotein particle size and esterification rate in apoB-
lipoprotein-depleted plasma (FERHDL). Clin Biochem.
2001;34:583–588.
Dobiásová M. Atherogenic index of plasma [Log
(triglycerides/ HDL-cholesterol)]: theoretical and
practical implications. Clin Chem. 2004;50:1113–1115.
Fauzia Ashfaq,P.K. Goel, Nagraja Moorthy,1 Rishi
Sethi,2Mohammed Idrees Khan, Mohammed Zafar
Idris. Lipoprotein(a) and SYNTAX Score Association
with Severity of Coronary Artery Atherosclerosis in
North India. Clinical and basic research, Sultan Qaboos](https://image.slidesharecdn.com/pdf-190610041739/75/Syntax-Score-and-its-Relation-to-Lipoprotein-a-Lp-a-and-Extended-Lipid-Parameters-in-Non-Diabetic-Patients-with-Acute-Coronary-Syndrome-Having-Age-below-55-Years-6-2048.jpg)