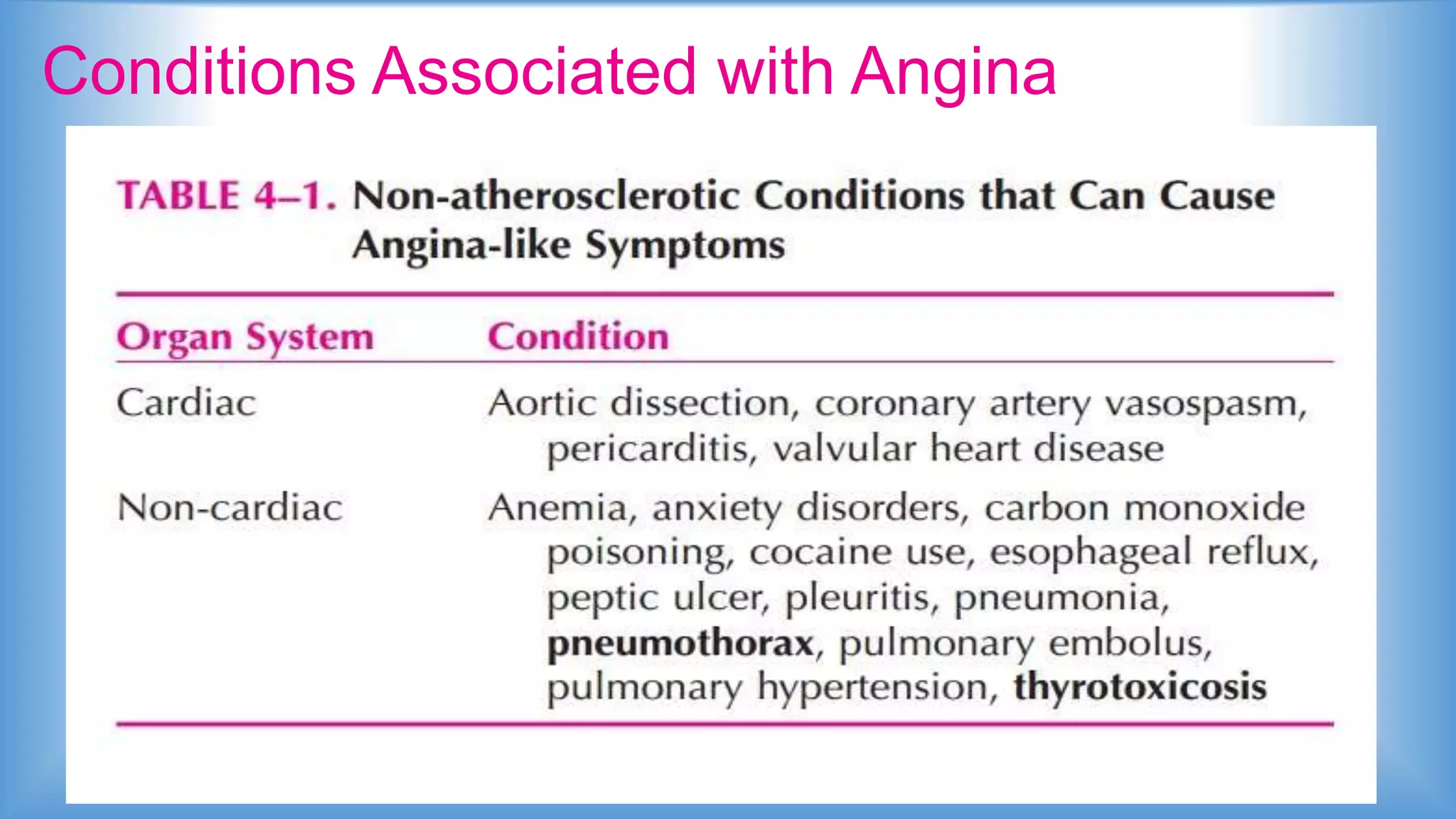
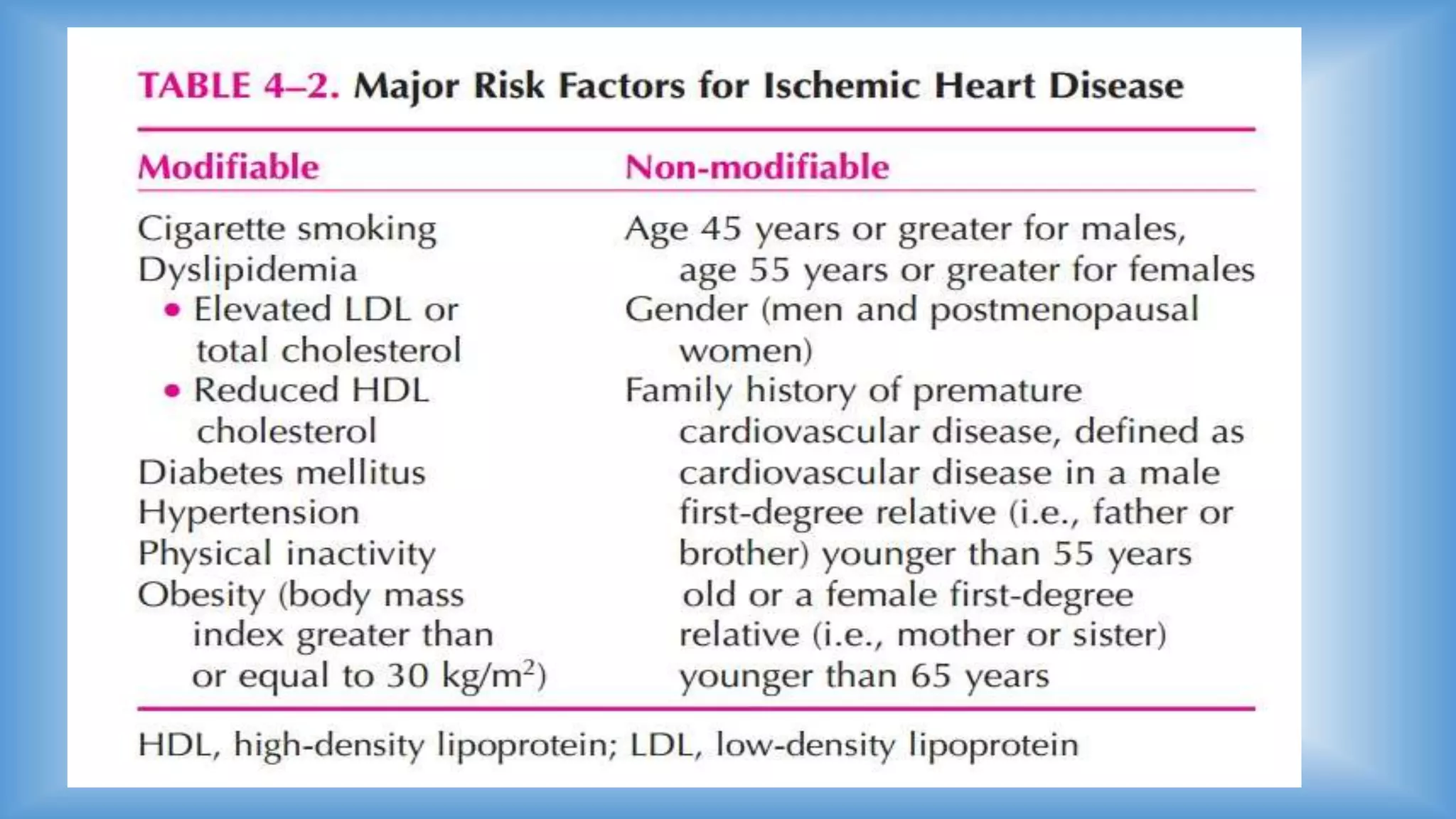
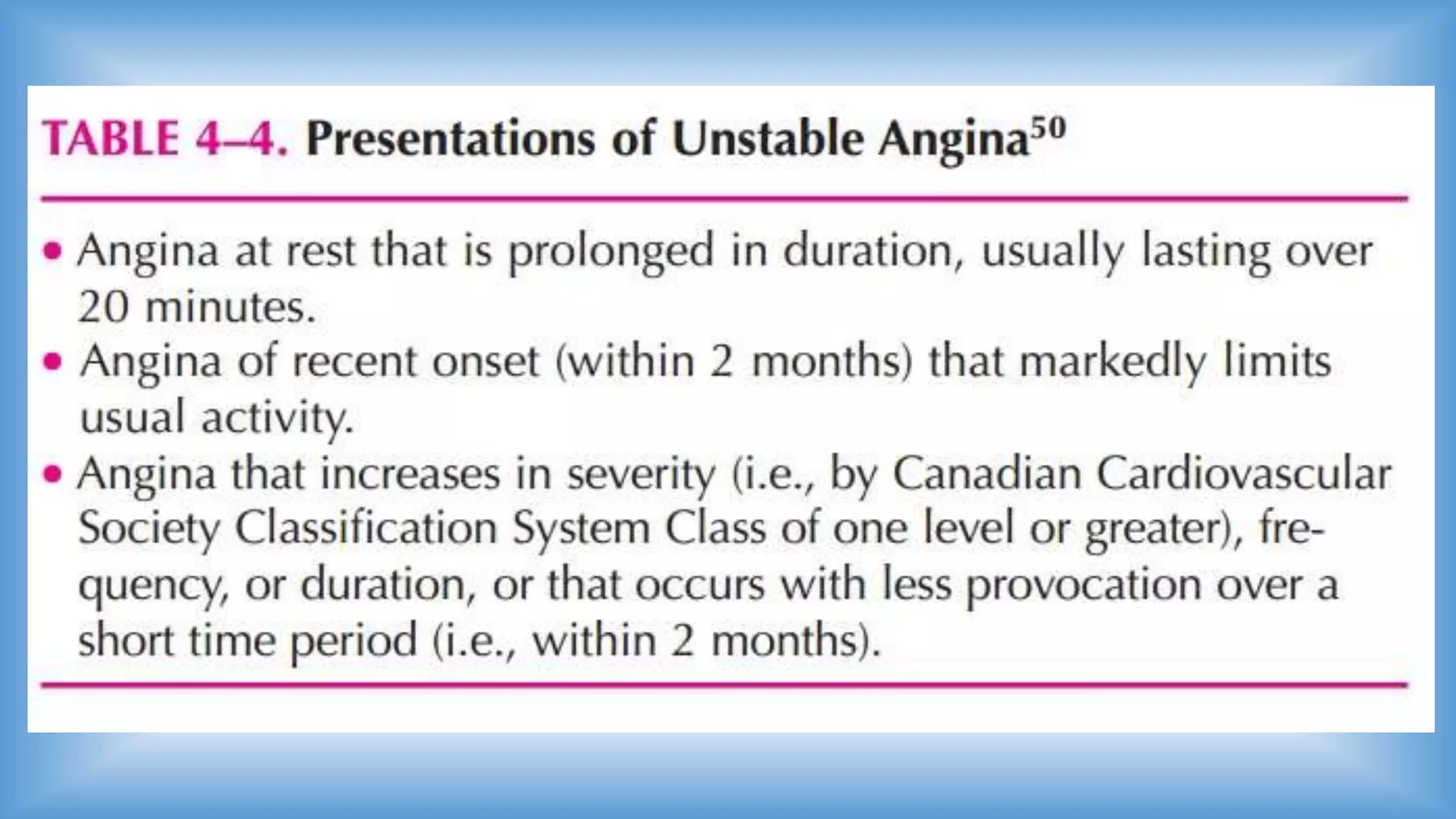
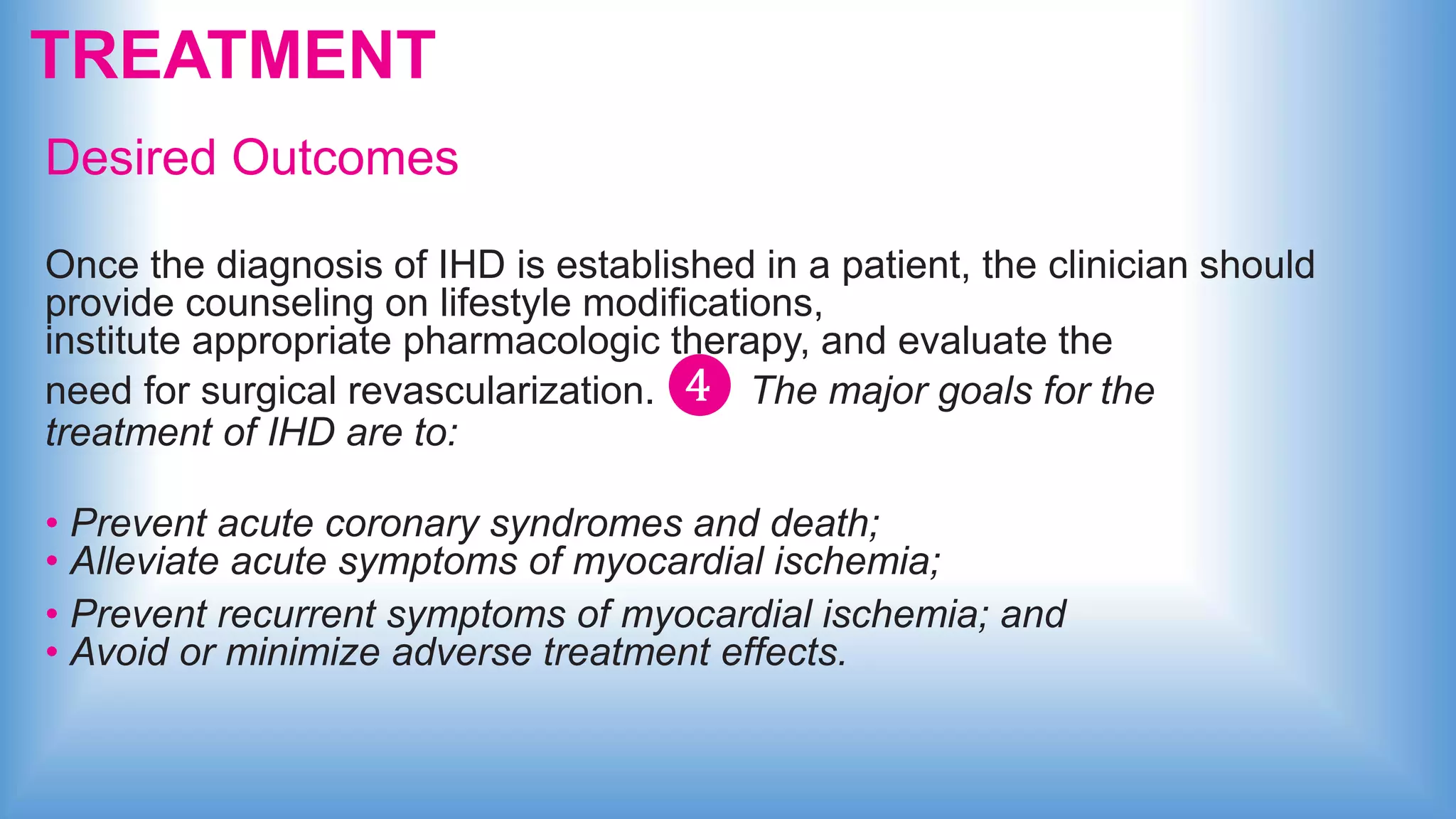
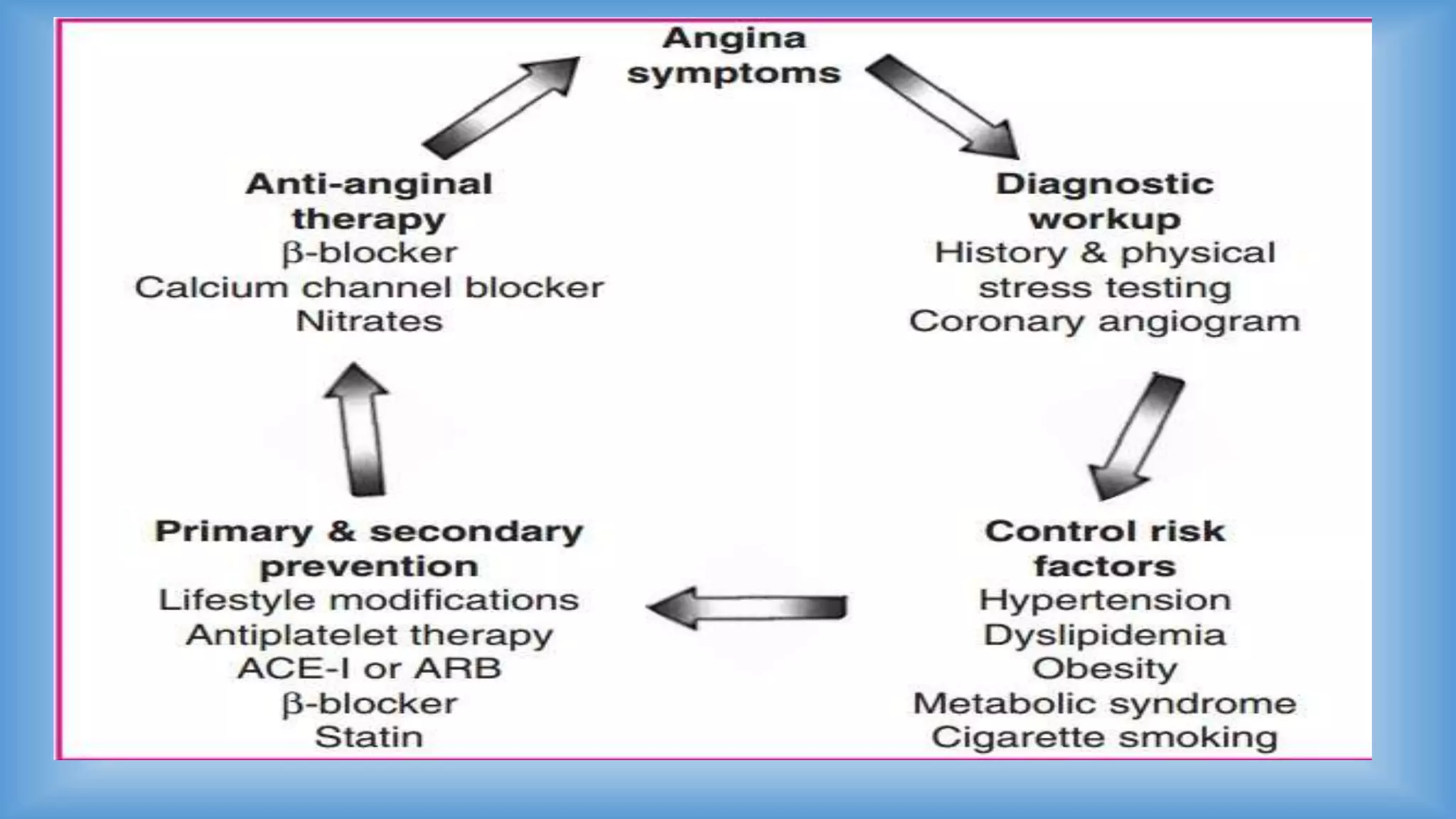
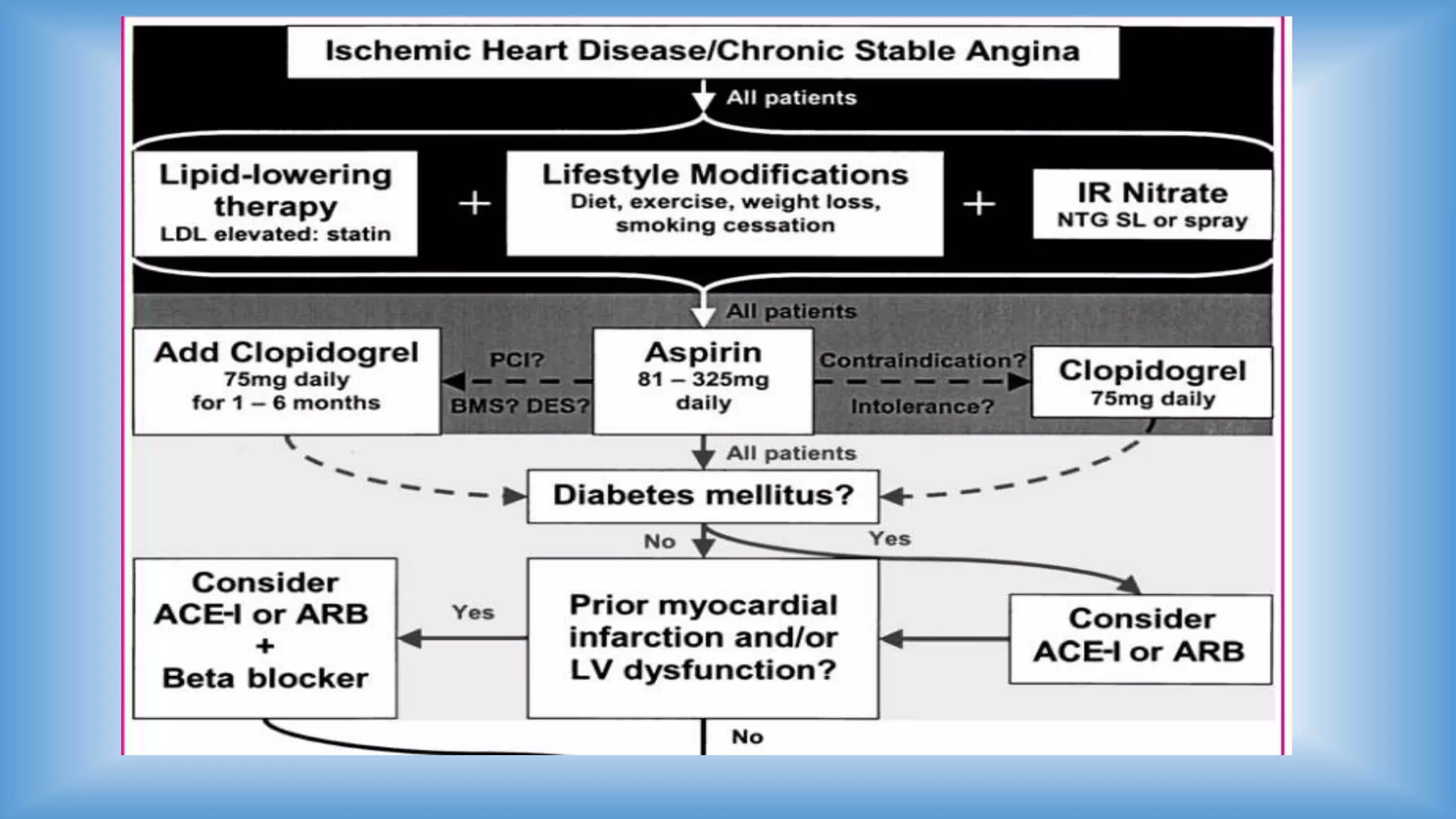
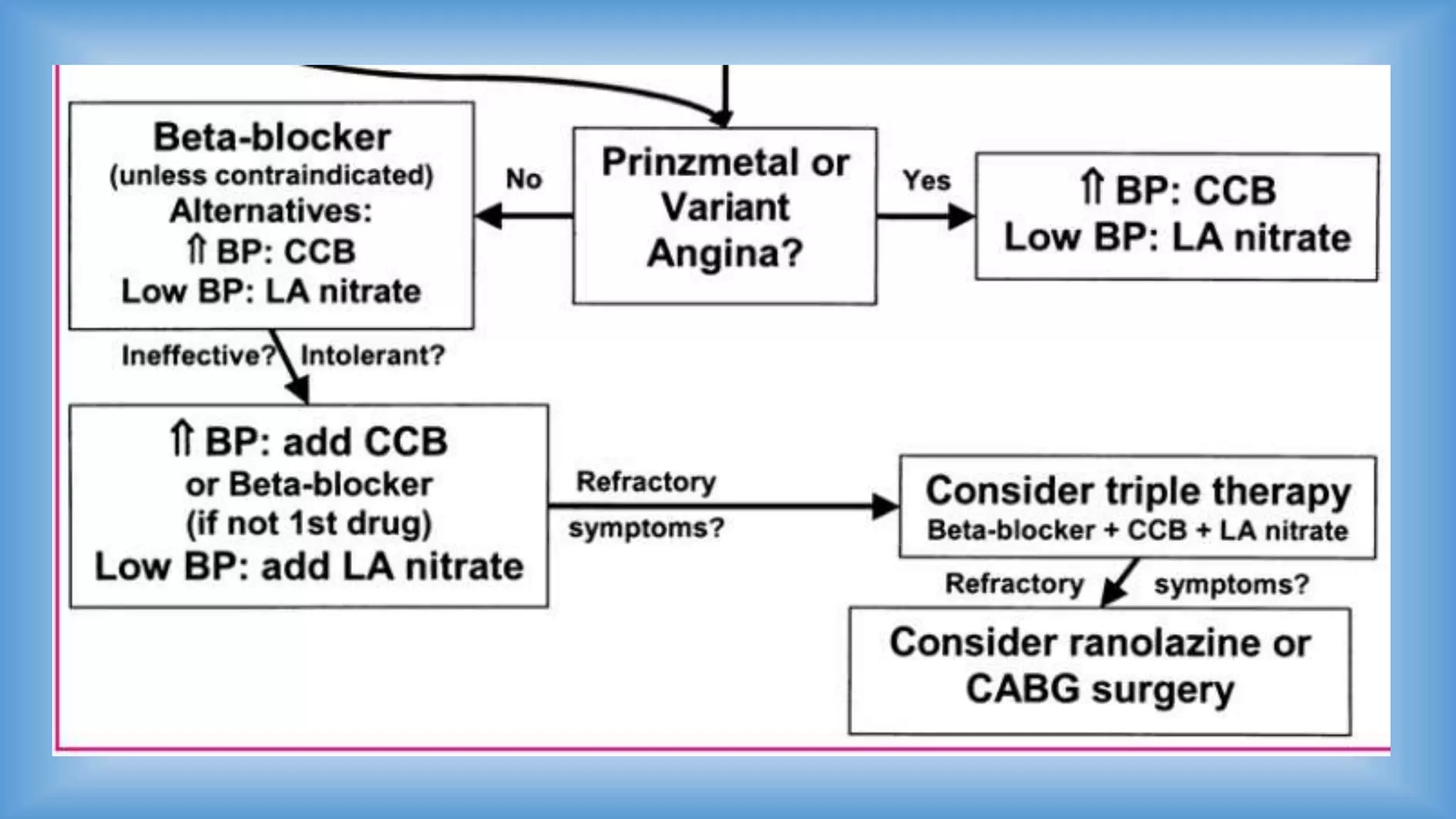
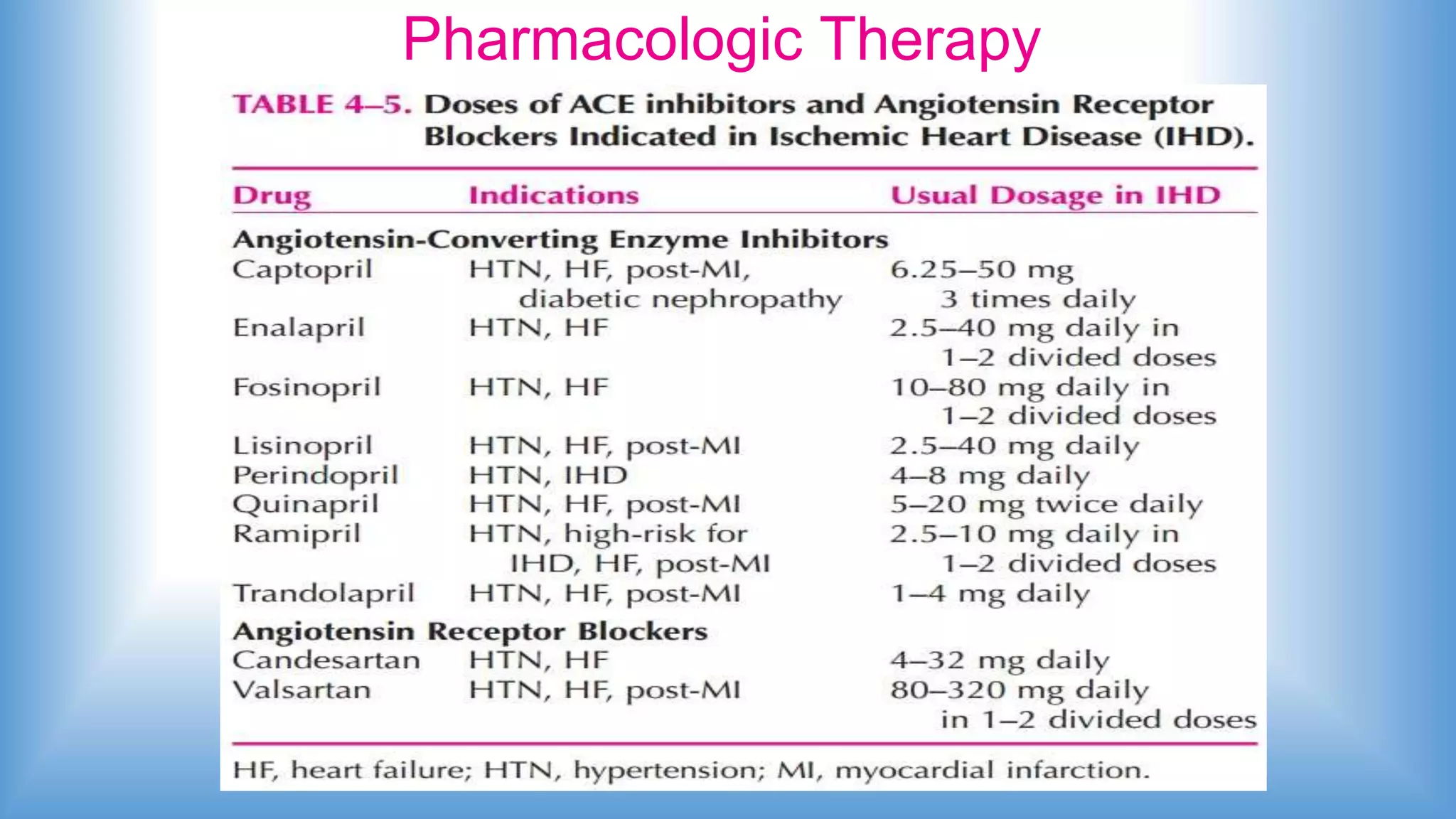
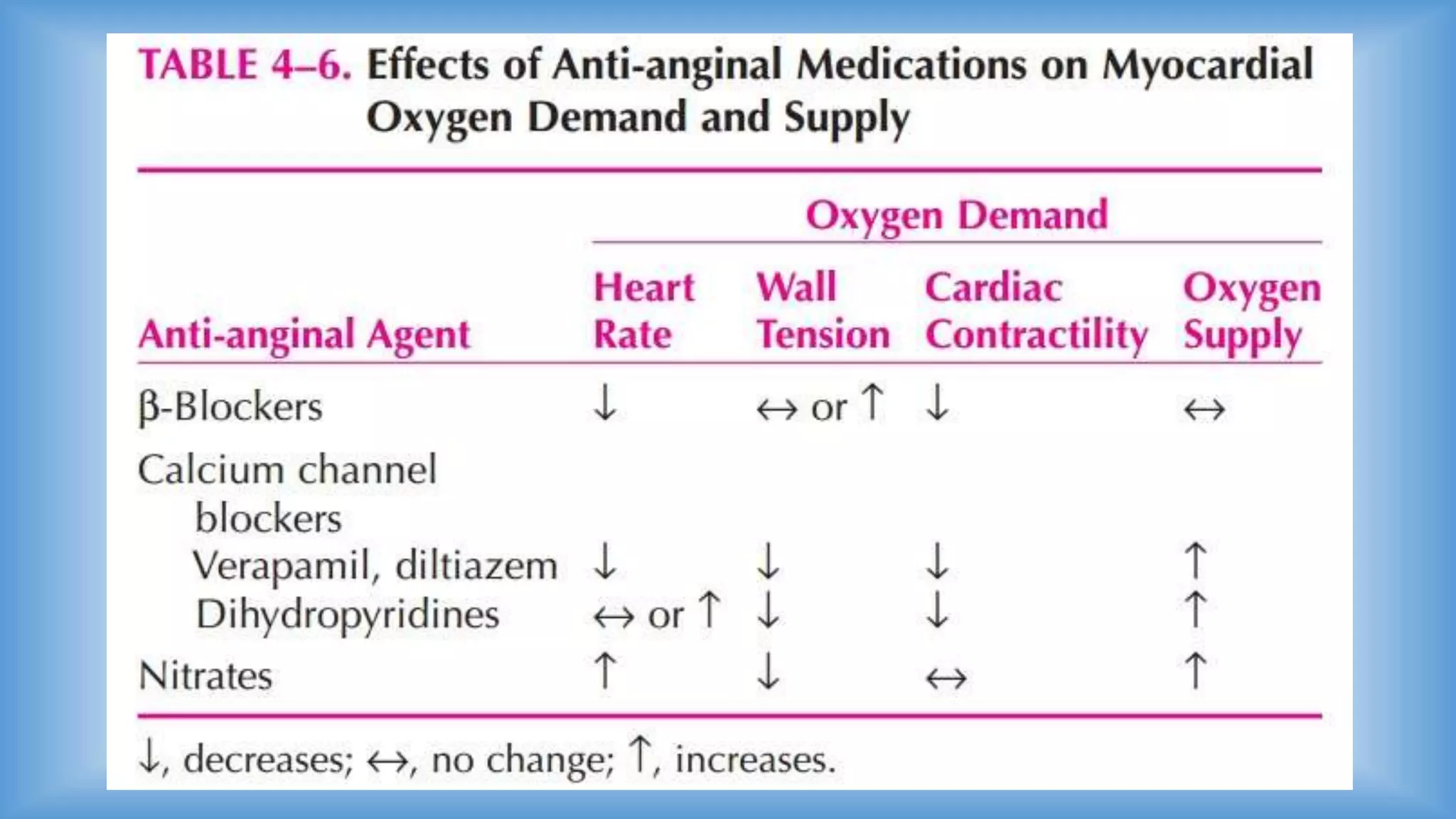
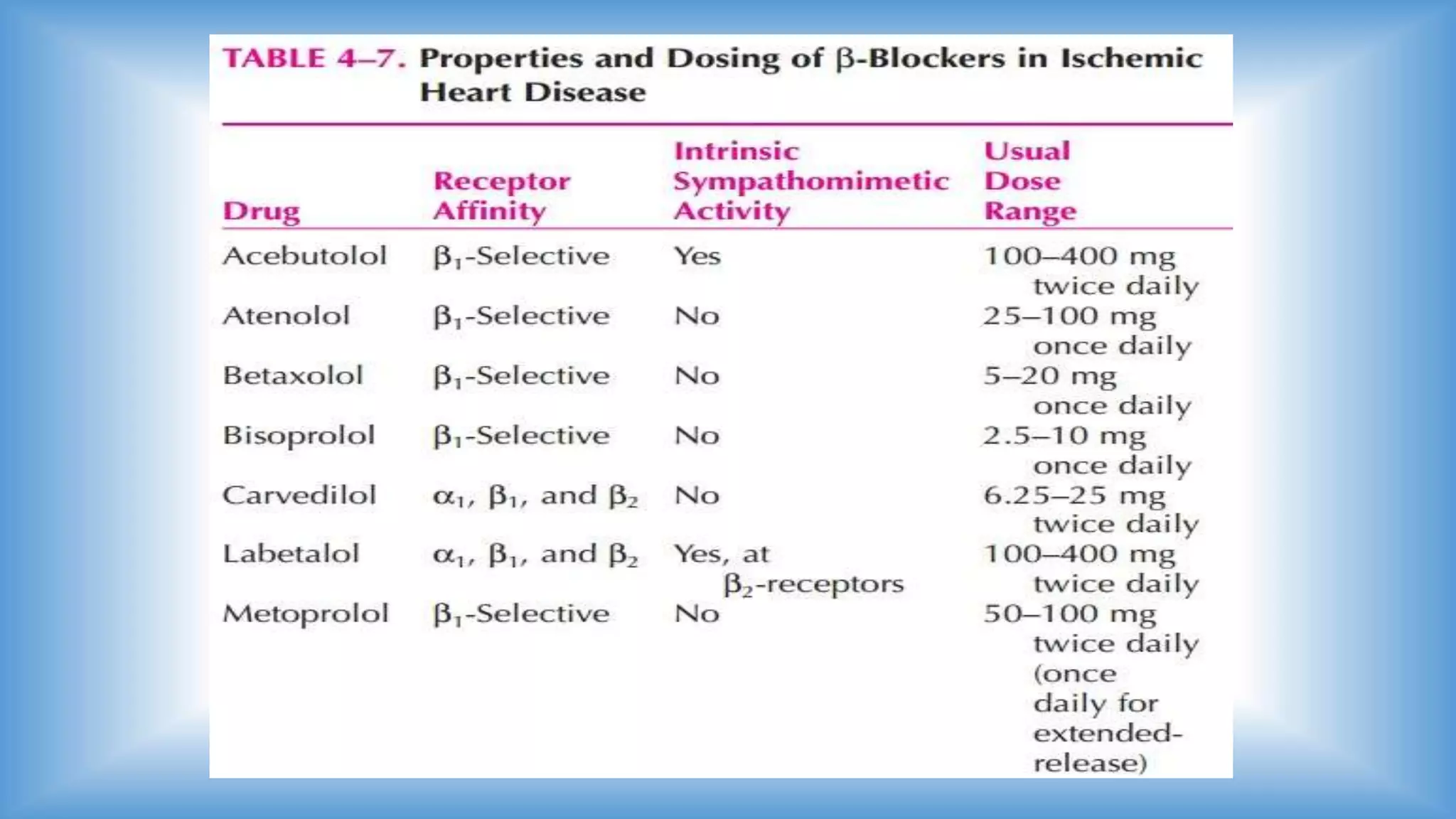
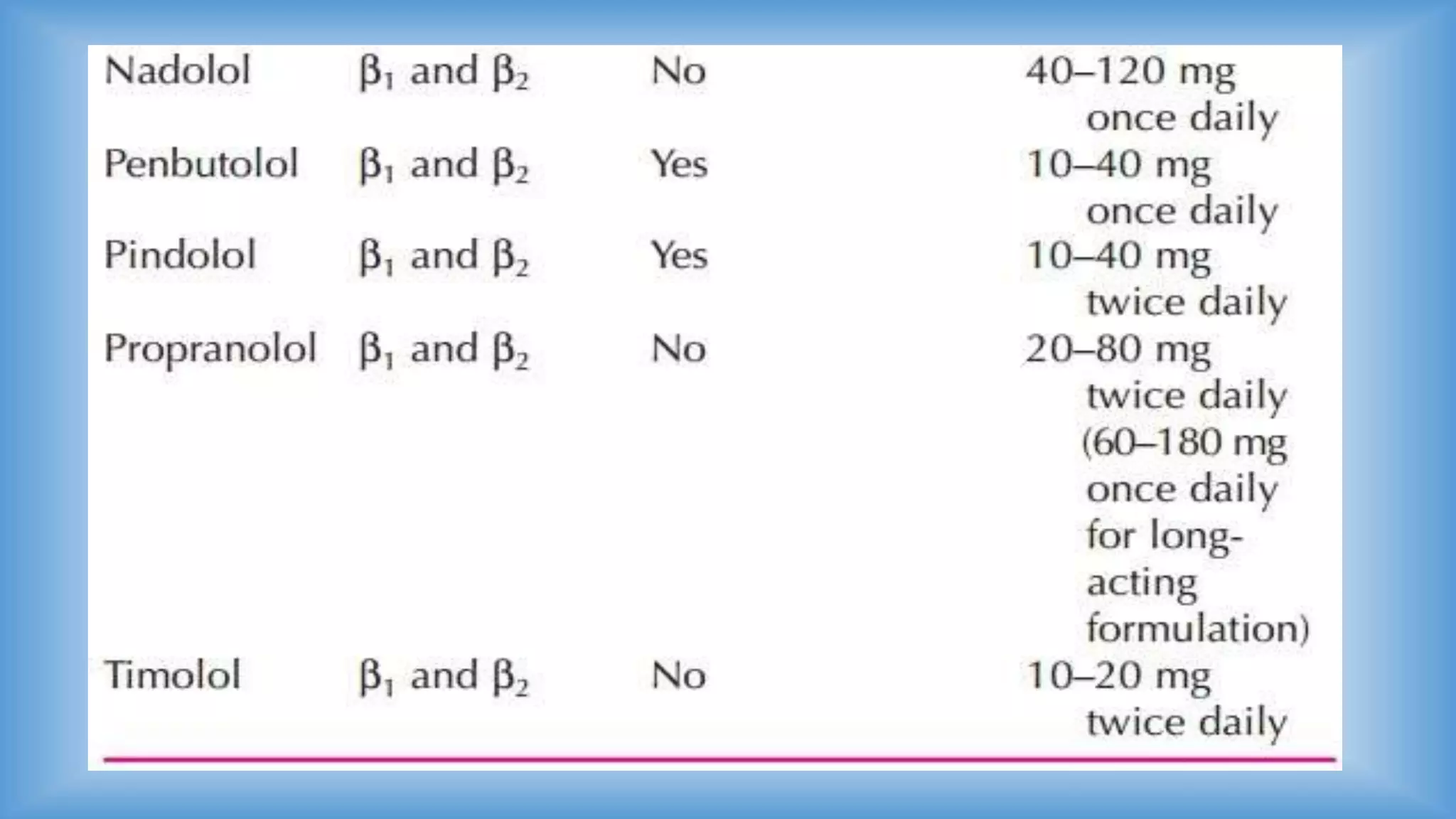
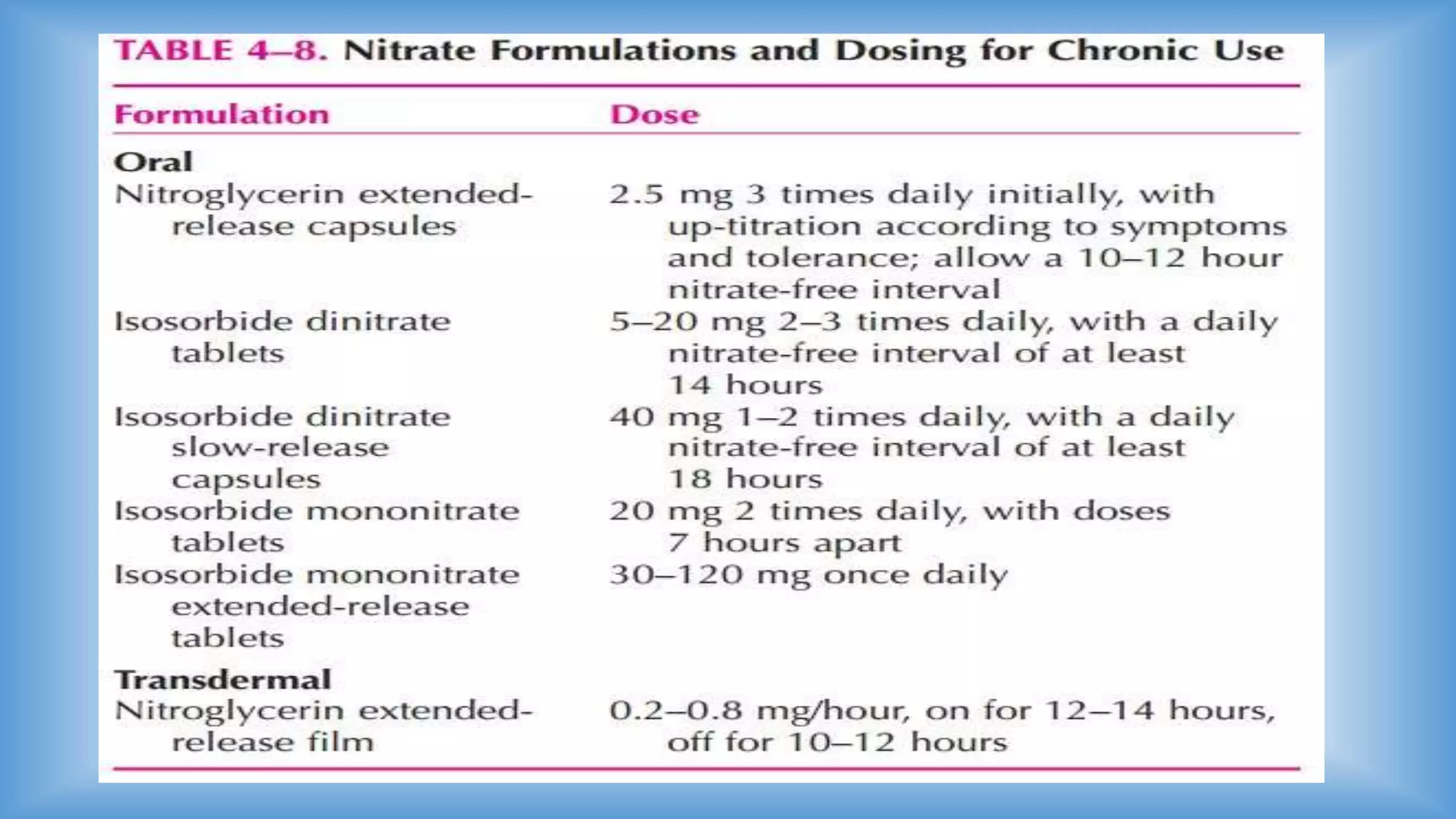
This document discusses cardiovascular disorders, specifically hyperlipidemia and coronary heart disease. It covers the pathophysiology of lipid metabolism and atherosclerosis, conditions that can cause angina, distinguishing characteristics of chronic stable angina versus unstable angina, and treatments including lifestyle modifications, pharmacotherapy, percutaneous coronary intervention, and coronary artery bypass graft surgery. The goal of treatment is to prevent acute coronary events and death, alleviate acute ischemic symptoms, prevent recurrent ischemia, and minimize adverse effects of treatment.