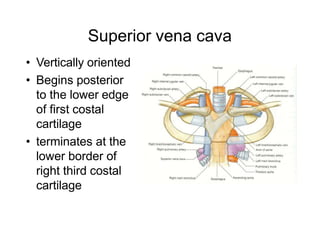
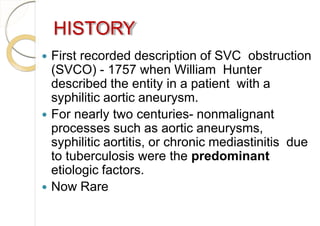
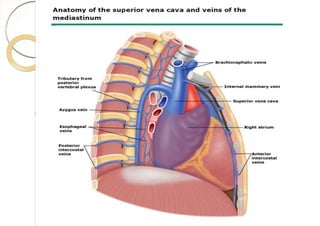
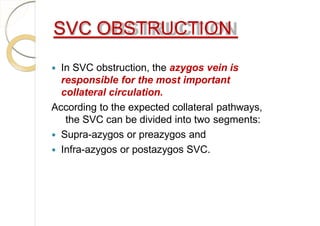
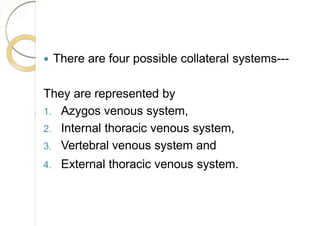
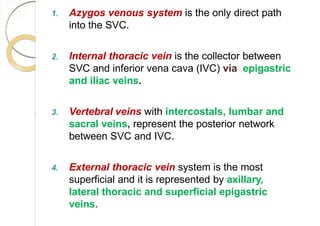
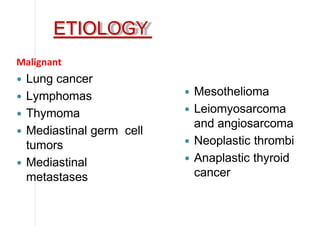
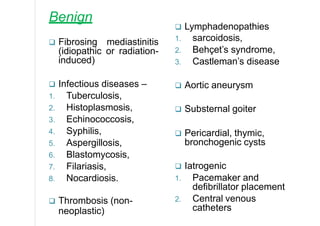
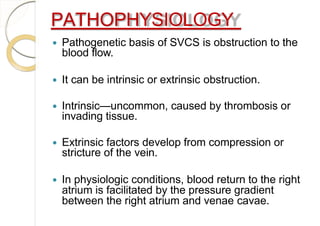
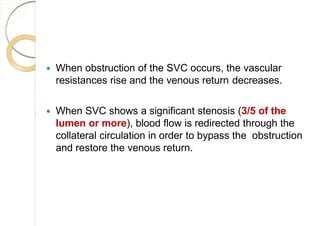
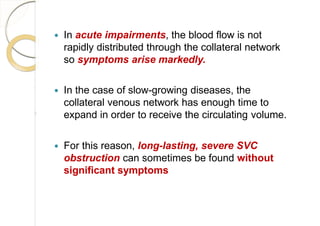
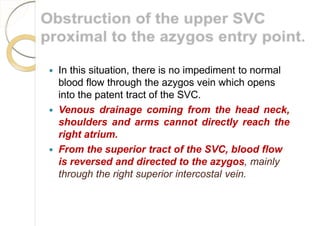
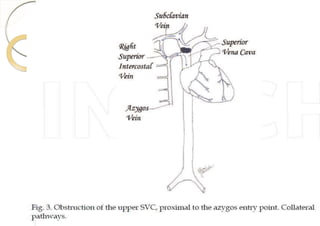
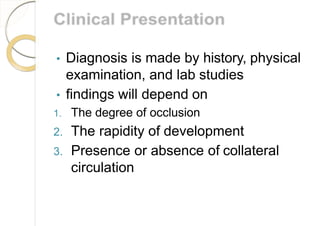
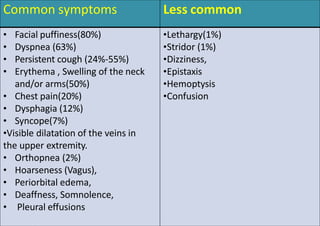
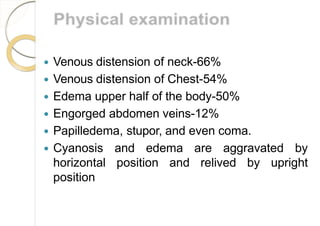
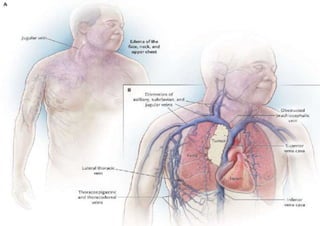
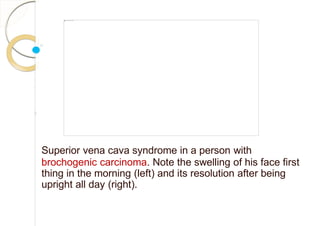
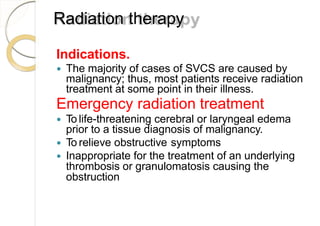
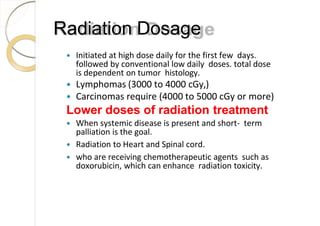
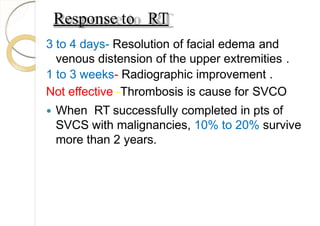
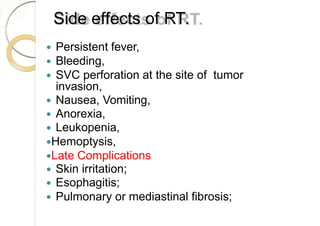
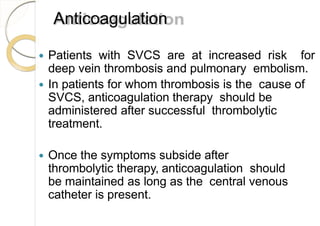
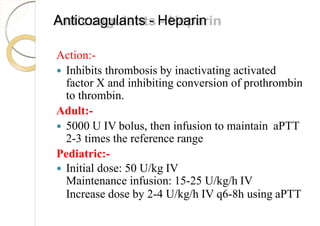
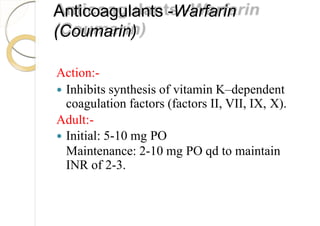
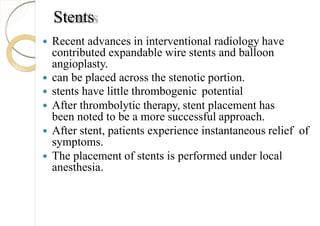
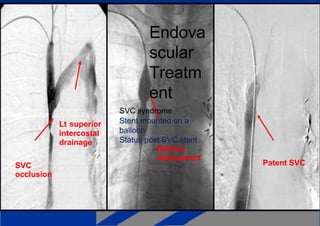
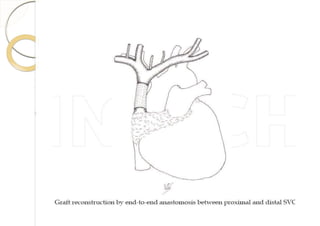
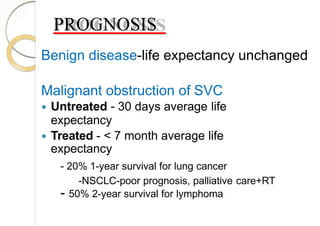
Superior vena cava syndrome is caused by obstruction of blood flow through the superior vena cava. The most common causes are lung cancer and lymphomas. Symptoms arise when collateral circulation is unable to compensate for the obstruction. Malignant causes are more frequent than benign etiologies such as fibrosing mediastinitis or infectious diseases. Treatment depends on relieving the obstruction through methods such as stenting or chemotherapy.