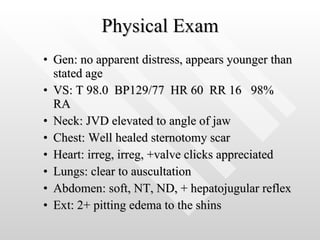
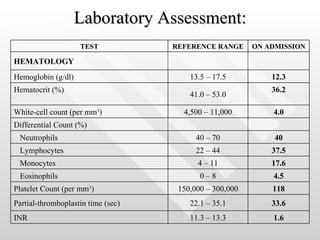
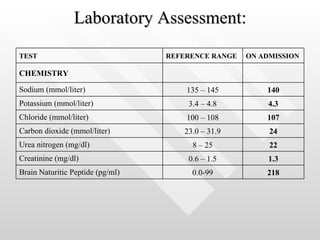
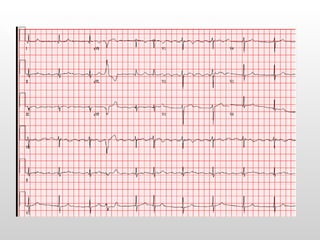
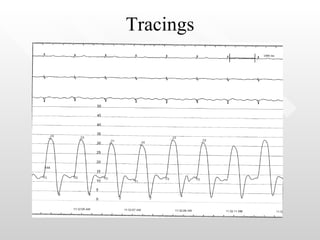
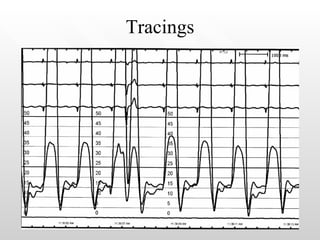
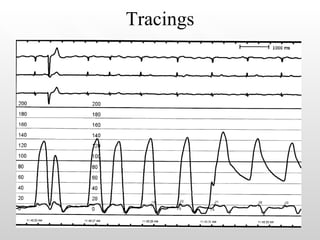
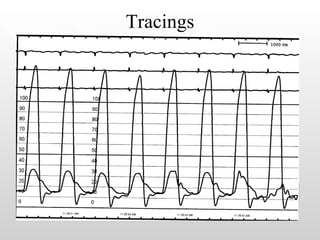
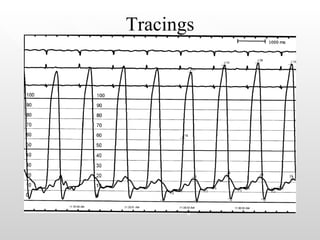
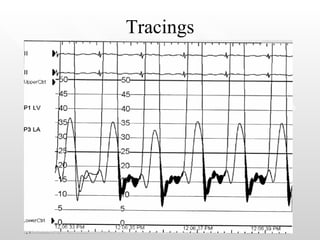
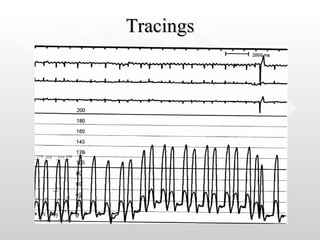
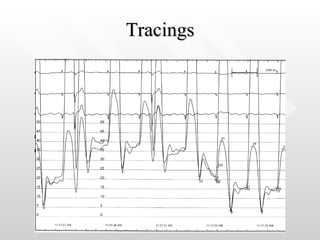
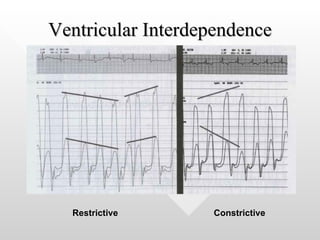
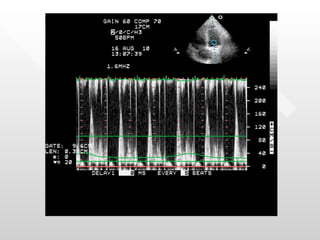
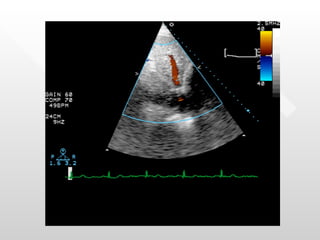
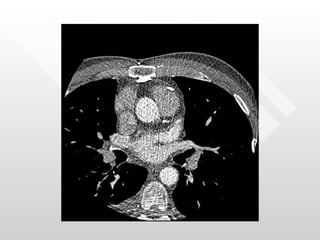
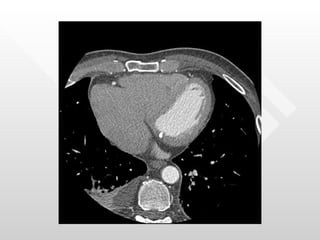
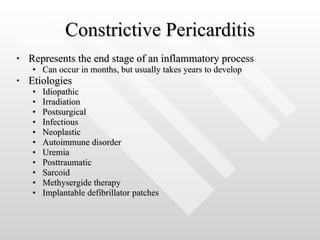
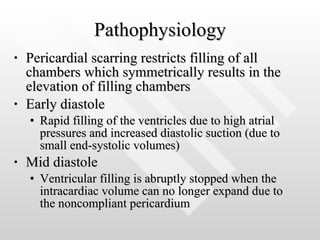
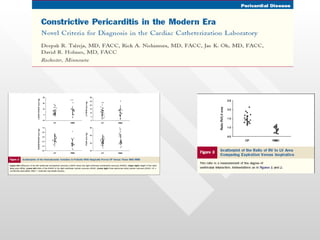
A 65-year-old male with a history of mitral valve replacement in 1975 presents with decreased exercise tolerance over the past two months. He has a history of paroxysmal atrial fibrillation for 10 years. Cardiac catheterization was ordered to assess his coronary arteries and measure the gradient across his mitral valve. Tracings from the catheterization show early rapid filling of the ventricles followed by abrupt stopping of ventricular filling in mid diastole, consistent with constrictive pericarditis.