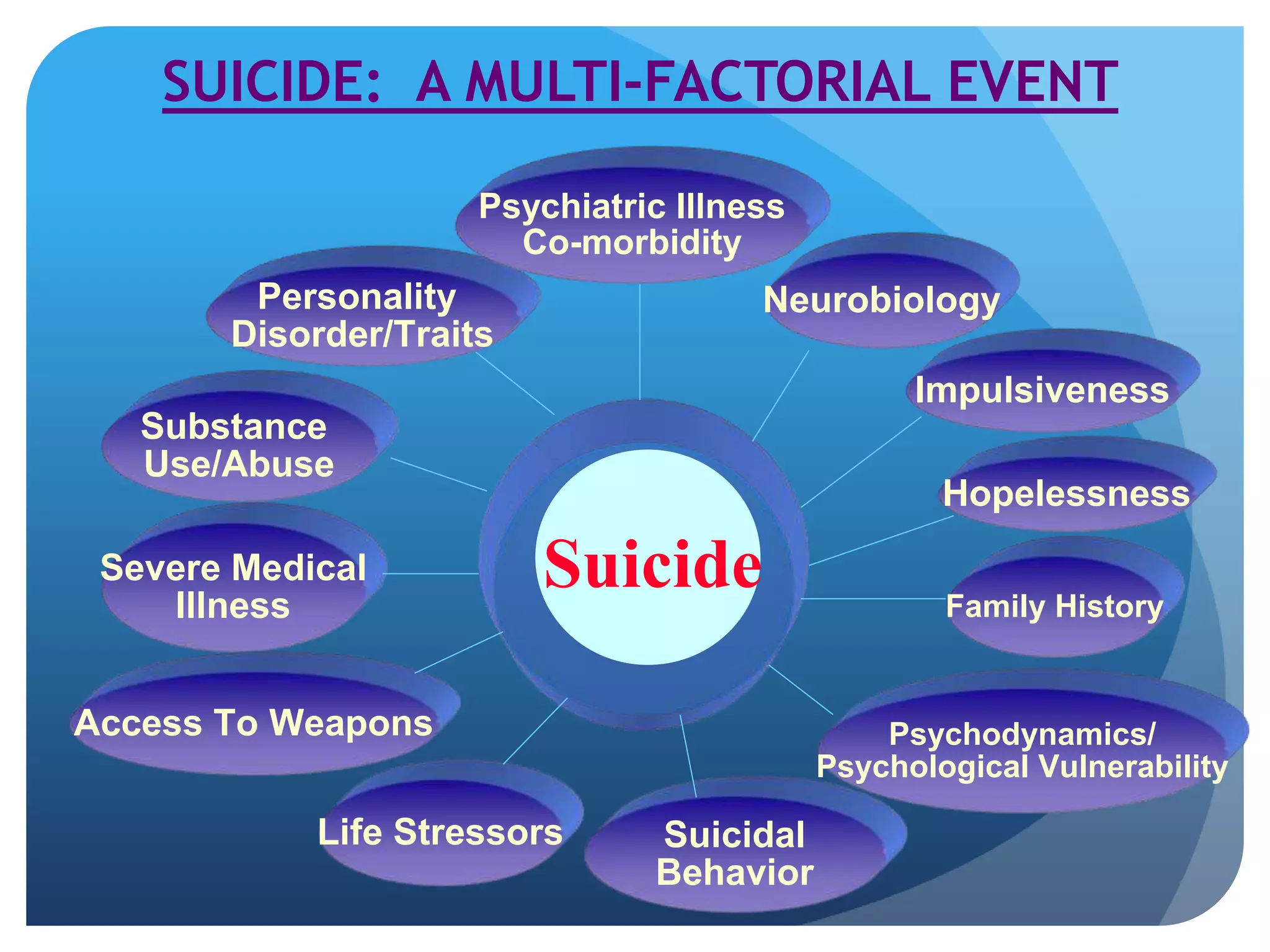
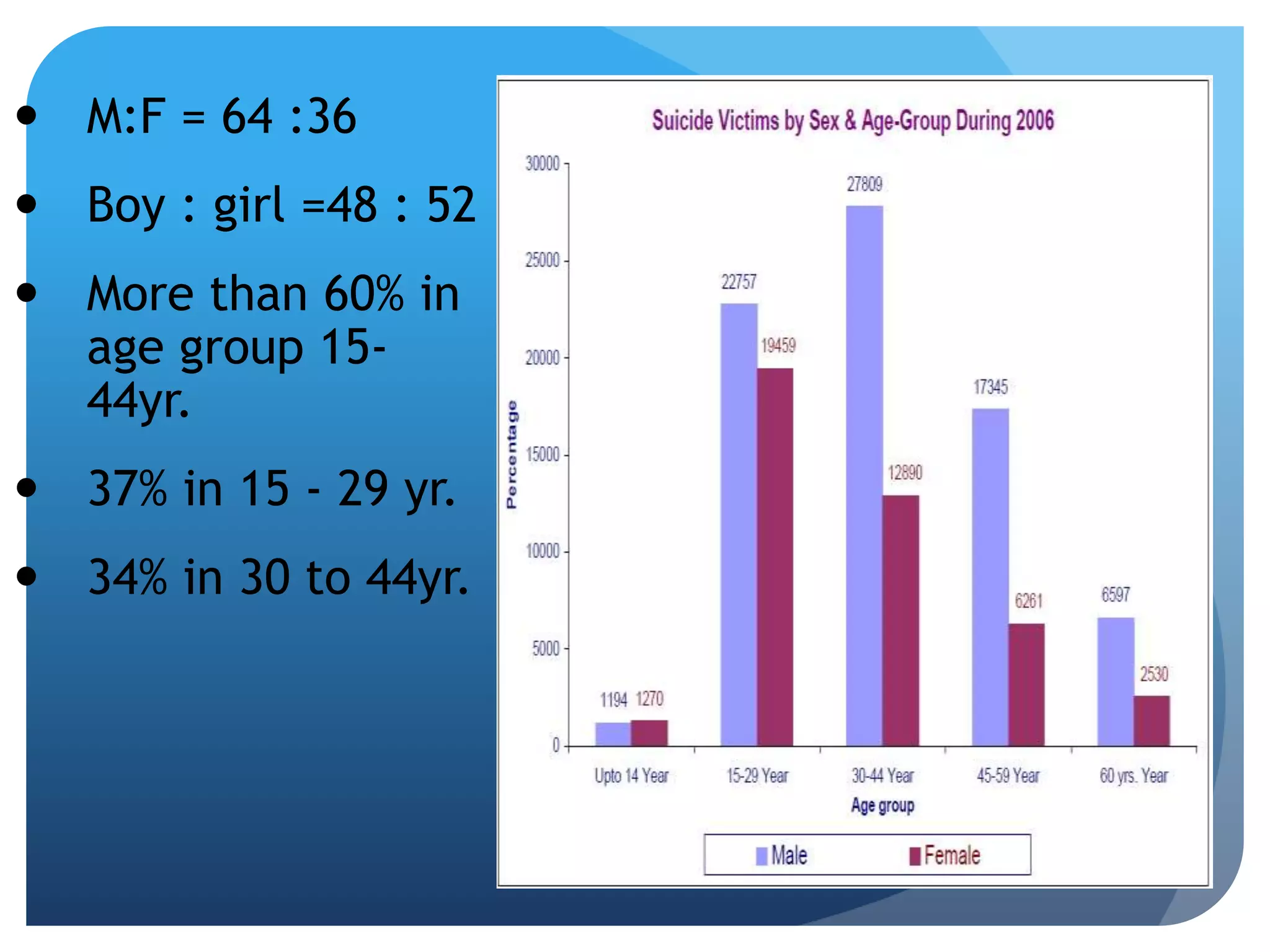
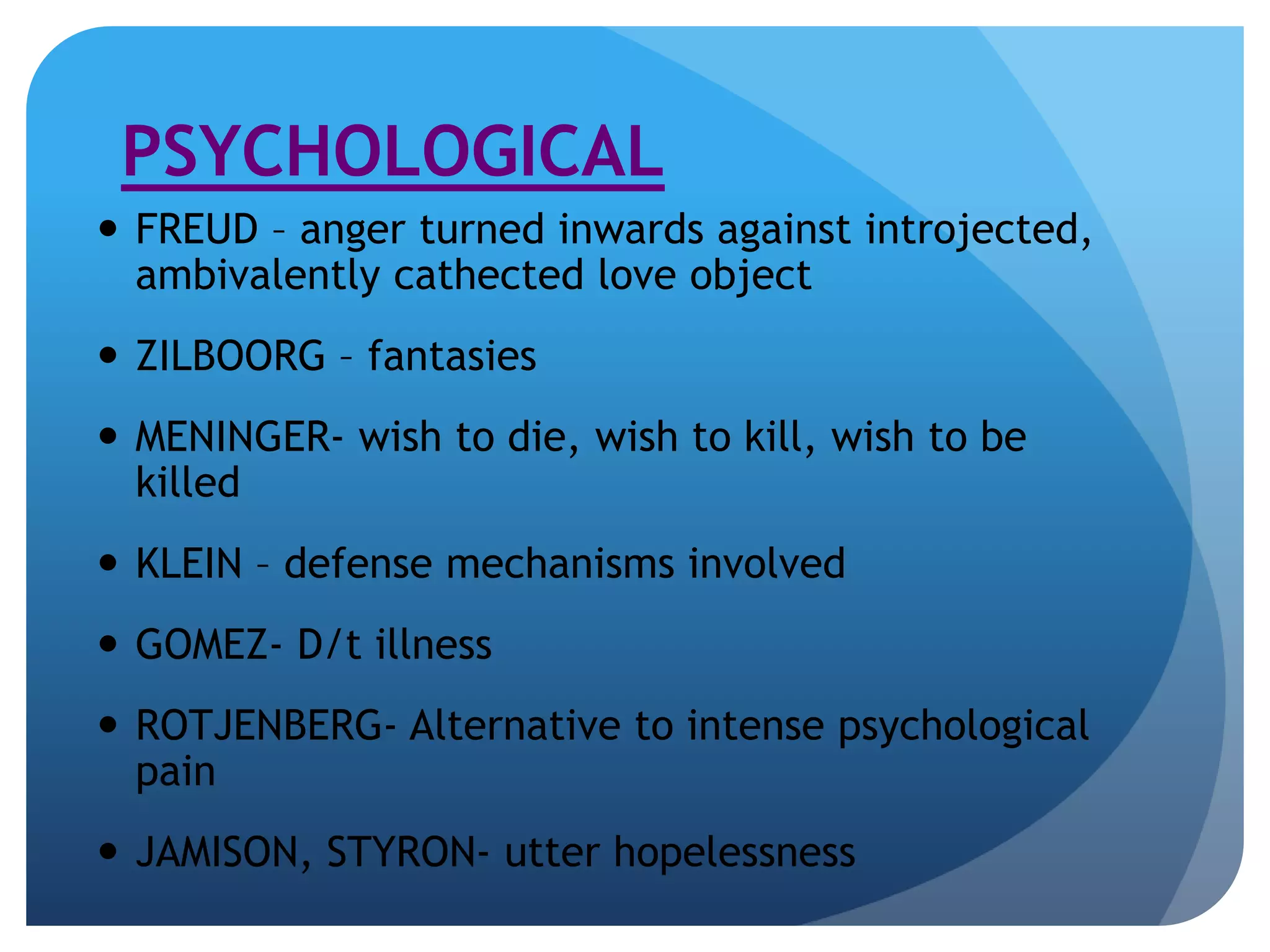
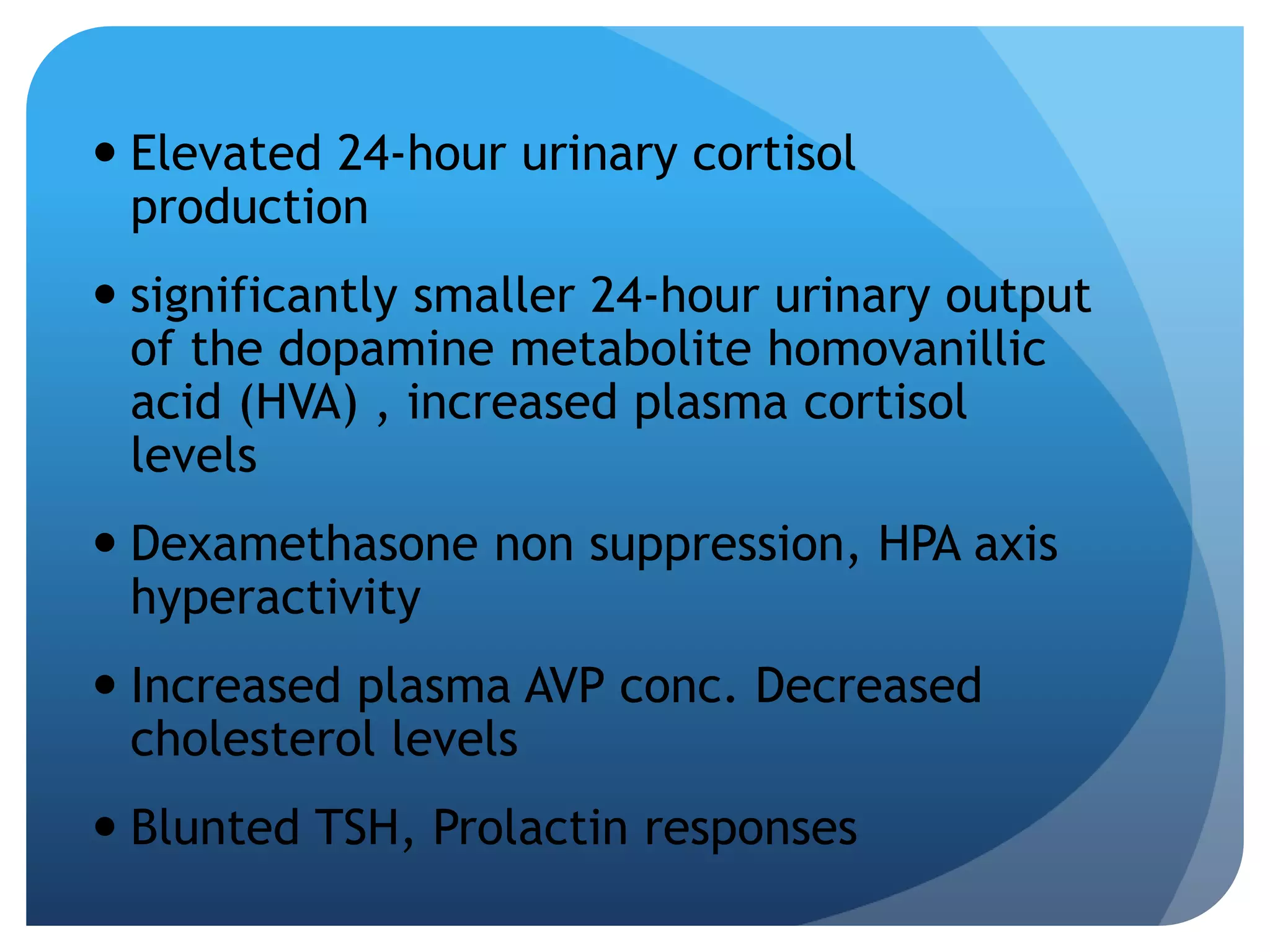
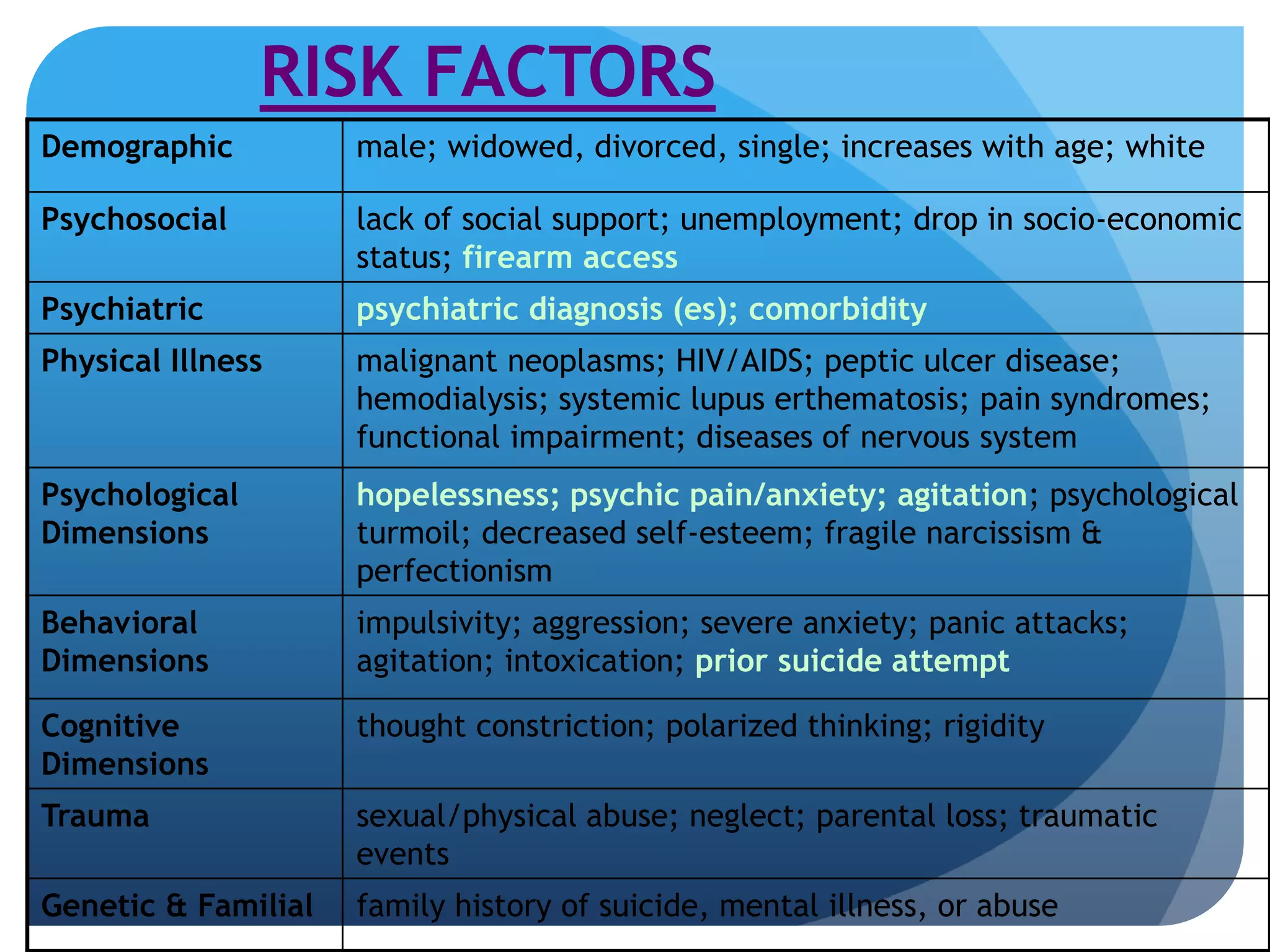
This document defines various terms related to suicide and discusses suicide from epidemiological, etiological, and clinical perspectives. It notes that over 90% of suicides are associated with psychiatric disorders like depression and substance abuse. Key risk factors include male gender, older age, social isolation, impulsivity, and a family history of suicide. A comprehensive suicide assessment evaluates psychiatric illnesses, risk and protective factors, and determines the level of risk to guide treatment and safety planning.