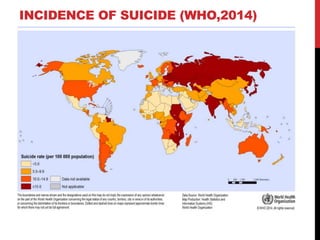
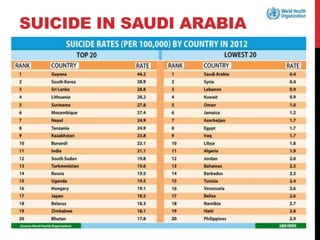
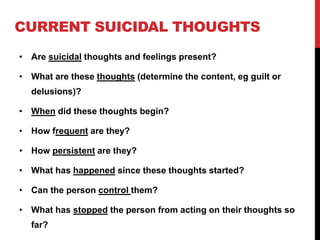
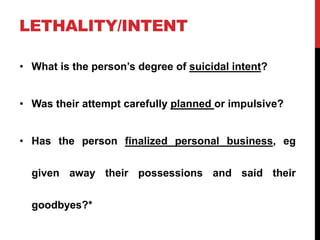
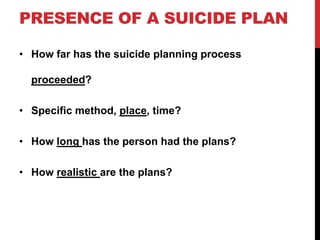
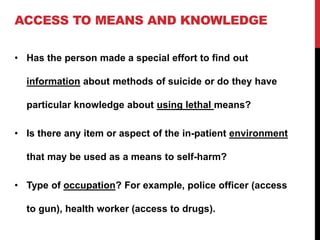
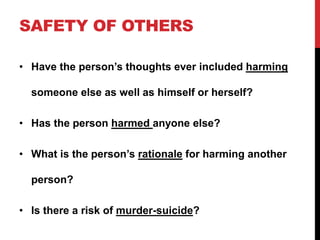
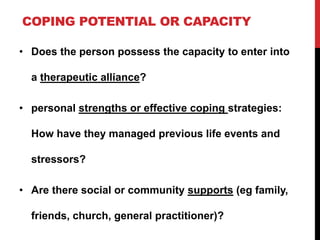
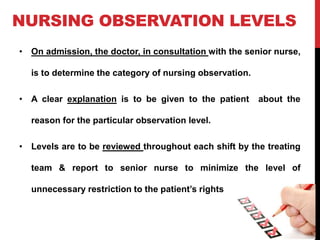
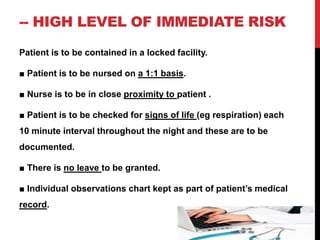
This document discusses suicide, highlighting its definition, prevalence, factors affecting rates, modes, warning signs, and prevention measures. It emphasizes that suicides are largely preventable with effective interventions and outlines nursing assessments and interventions for patients with suicidal ideation. The content aims to equip healthcare providers with knowledge to better support and assess individuals at risk.