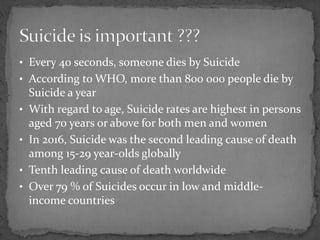
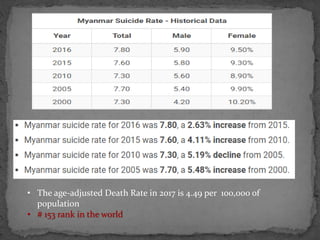
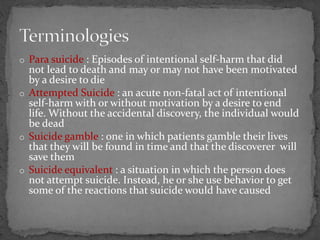
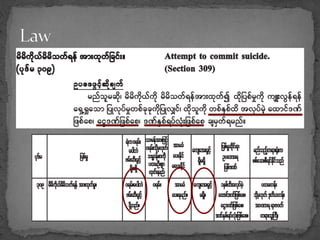
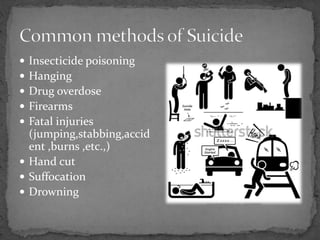
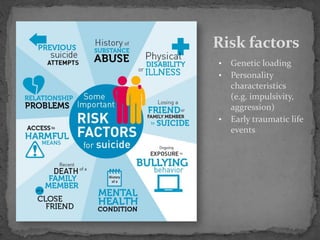
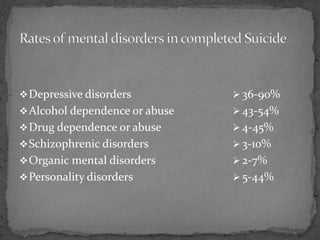
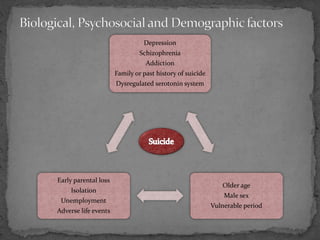
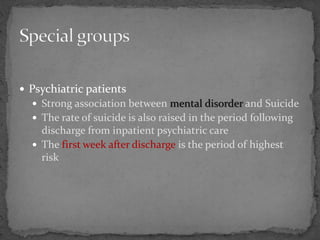
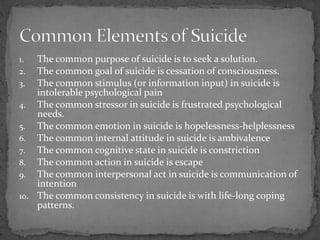
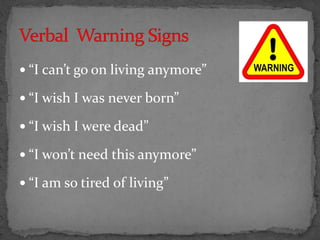
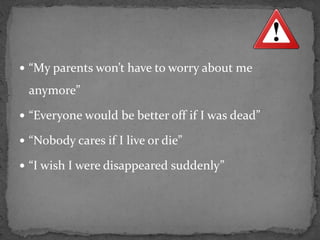
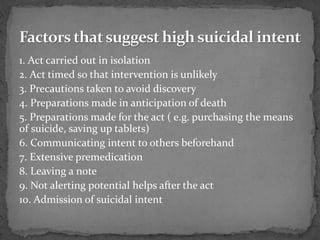
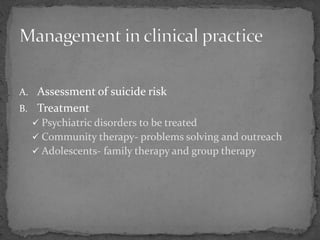
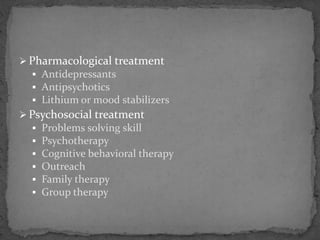
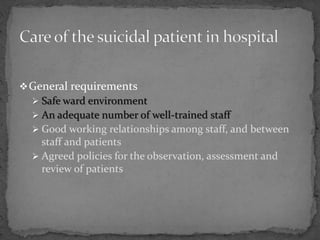
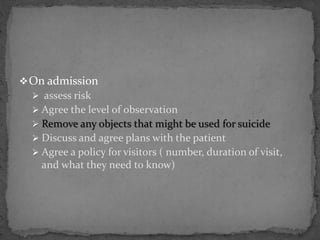
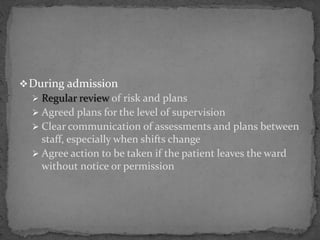
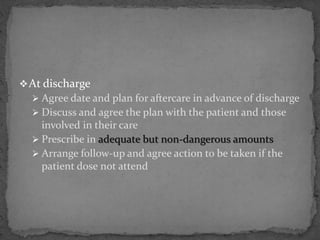
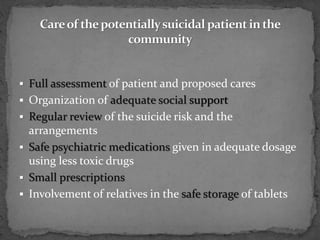
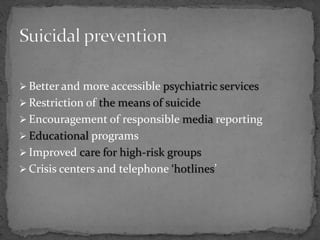
This document discusses suicide and its prevention. It provides information on risk factors for suicide like mental illness, past attempts, and life stressors. Common warning signs and methods are outlined. The assessment and management of suicidal patients is also described, including treatment, observation in hospitals, and ensuring community support after discharge. Suicide prevention strategies discussed include restricting access to lethal means, educating the public, and improving mental healthcare.