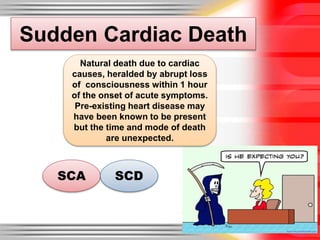
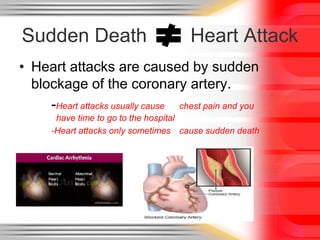
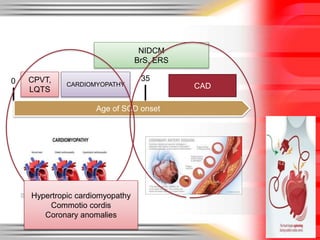
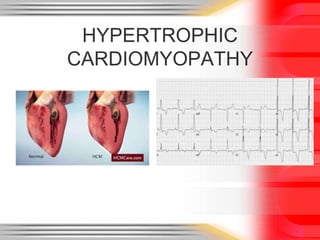
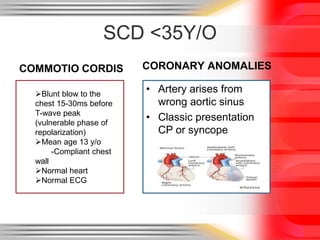
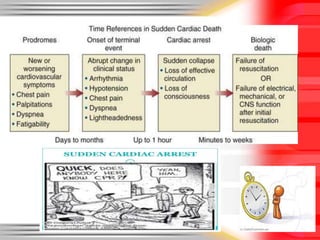
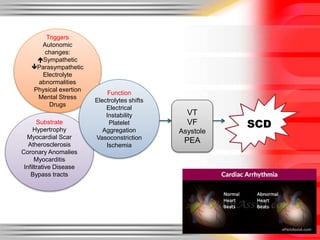
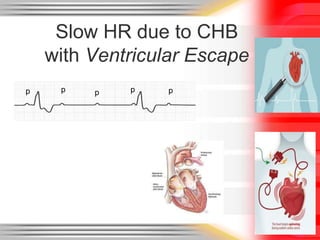
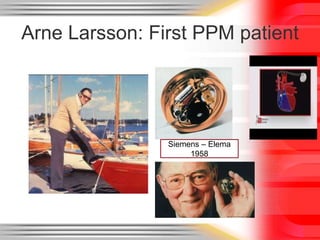
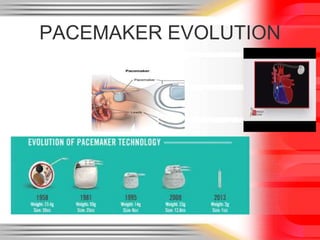
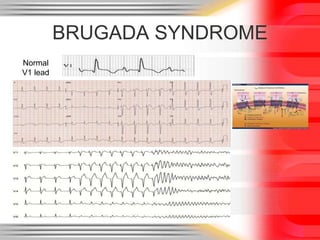
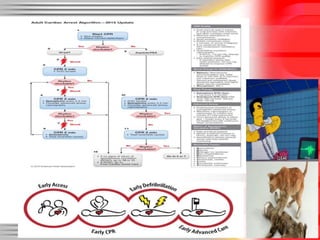
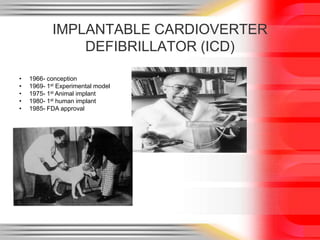
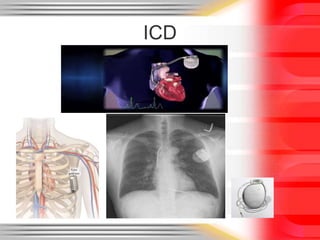
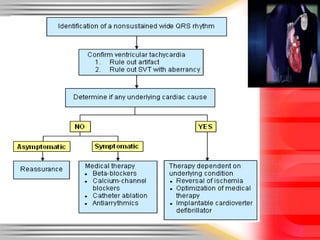
Sudden cardiac death is defined as a natural death from cardiac causes within one hour of the onset of symptoms. It can occur unexpectedly in people with known or unknown pre-existing heart disease. The main causes of sudden cardiac death are heart attacks in those over 35 and hypertrophic cardiomyopathy, commotio cordis, and coronary anomalies in those under 35. Pacemakers and implantable cardioverter-defibrillators have been developed to treat arrhythmias and help prevent sudden cardiac death.