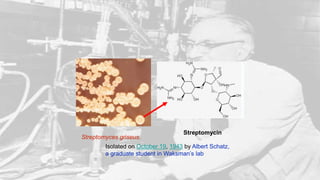
Streptomycin was the first effective treatment for tuberculosis. It was discovered in 1943 by Albert Schatz, a graduate student working in Selman Waksman's laboratory. Schatz isolated streptomycin from the soil microbe Streptomyces griseus. Animal testing showed it cured tuberculosis in guinea pigs. Clinical trials then found it successfully treated TB patients. Mass production of streptomycin was undertaken by the Merck pharmaceutical company. It revolutionized TB treatment and marked an important milestone in the discovery of antibiotics.



![OK, but how about people?
In August 1945 Hinshaw reported that
thirty-three patients had been treated
"and [we] continue to be quite optimistic”.
Streptomycin
appeared to be a miracle cure
• After Feldman and Hinshaw carried out animal testing ,they treated
"Patricia T." between November 1944 and February 1945. She was
streptomycin's first success against TB.](https://image.slidesharecdn.com/pptofantibiotics-170516090306/85/STREPTOMYCIN-24-320.jpg)
![• At the end of World War II, the United States Army experimented with
streptomycin to treat life-threatening infections at a military hospital
in Battle Creek, Michigan. The first patient treated did not survive; the
second patient survived but became blind as a side effect of the treatment.
In March 1946, the third patient—Robert J. Dole, later Majority Leader of
the United States Senate and Presidential nominee—experienced a rapid
and robust recovery.[24]](https://image.slidesharecdn.com/pptofantibiotics-170516090306/85/STREPTOMYCIN-25-320.jpg)
![• The first randomized trial of streptomycin against pulmonary tuberculosis
was carried out in 1946 through 1948 by the MRC Tuberculosis
Research Unit under the chairmanship of Geoffrey Marshall (1887–
1982). The trial was both double-blind and placebo-controlled. It is widely
accepted to have been the first randomized curative trial.
• Results showed efficacy against TB, albeit with minor toxicity and
acquired bacterial resistance to the drug.[26]](https://image.slidesharecdn.com/pptofantibiotics-170516090306/85/STREPTOMYCIN-26-320.jpg)