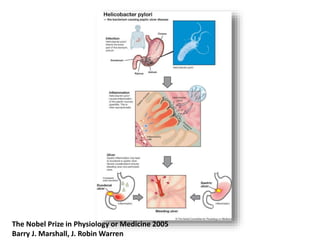
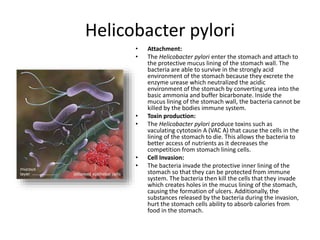
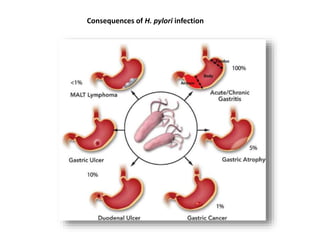
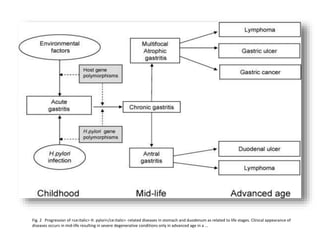
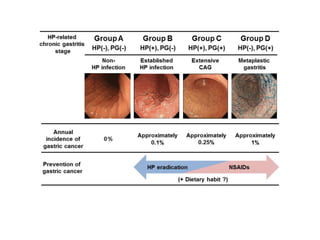
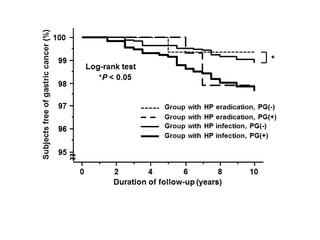
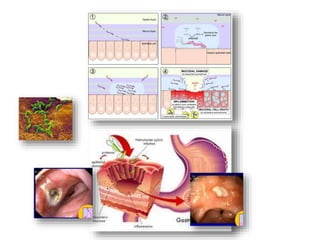
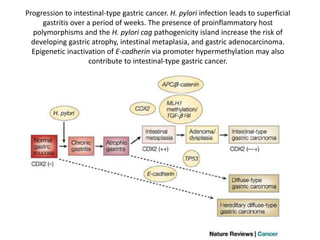
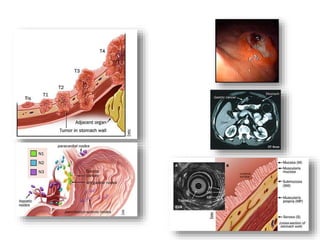
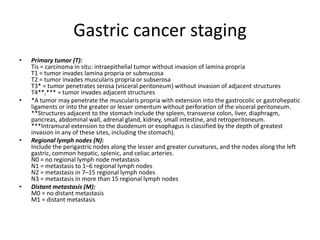
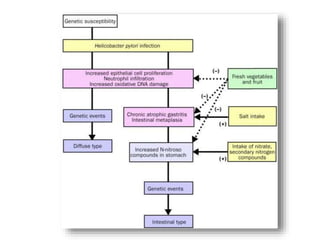
Gastritis is an inflammation of the stomach lining that can be caused by infection, autoimmune disorders, bile reflux, or pernicious anemia. Chronic gastritis refers to a wide range of disorders including those induced by H. pylori infection, NSAIDs, Crohn's disease, and more. H. pylori bacteria are able to attach to and invade the stomach lining, producing toxins that cause cell death and allow the bacteria to access nutrients while evading the immune system. Over time, prolonged H. pylori infection can potentially lead to gastric atrophy, intestinal metaplasia, and intestinal-type gastric cancer due to epigenetic changes. Gastric cancer staging evaluates the primary