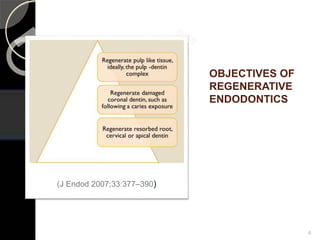
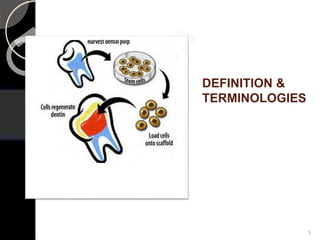
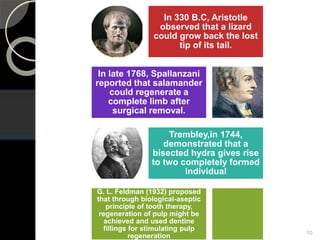
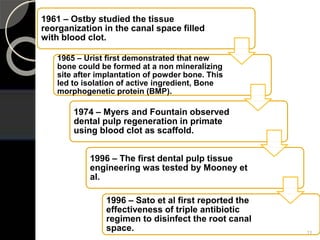
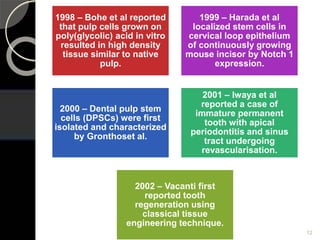
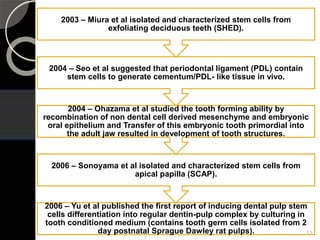
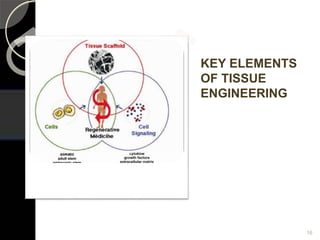
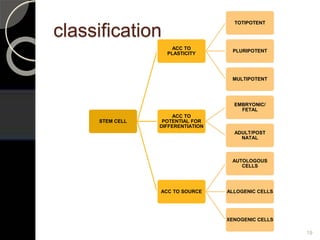
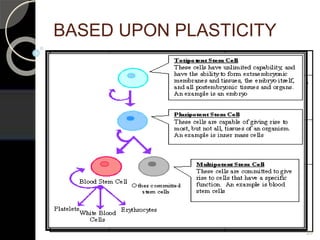
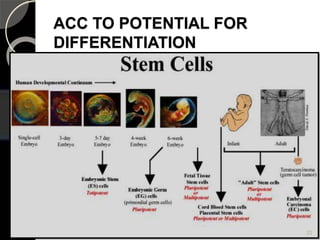
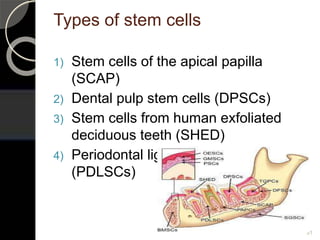
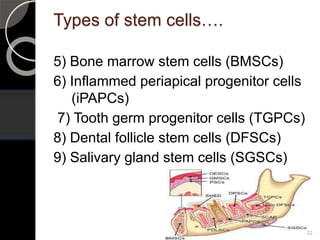
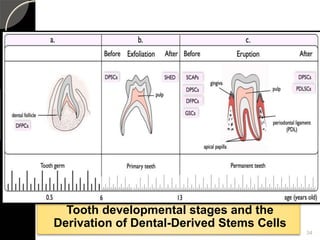
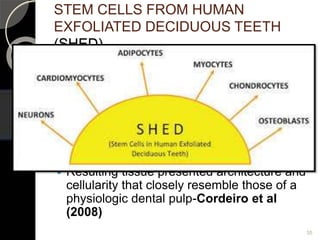
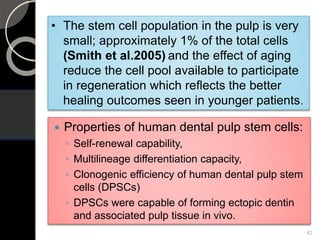
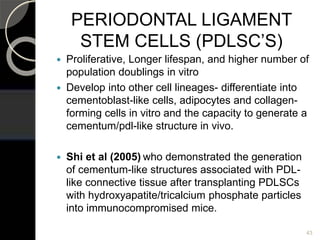
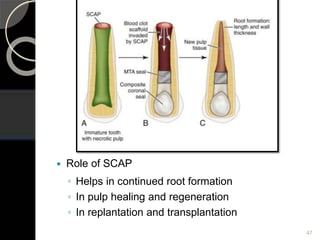
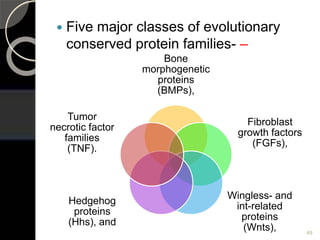
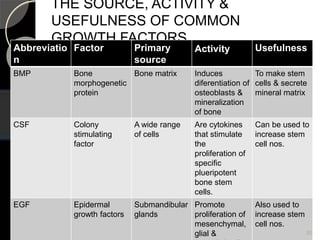
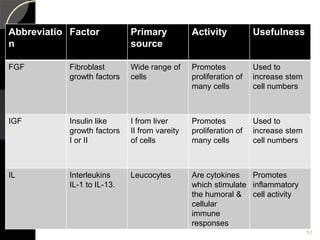
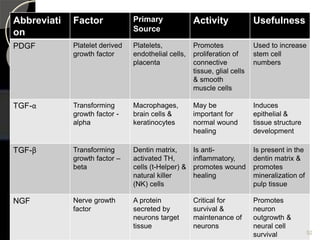
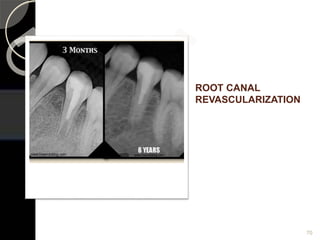
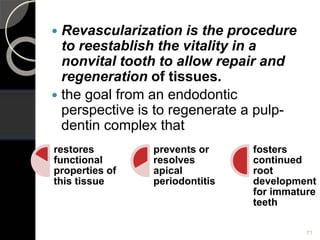
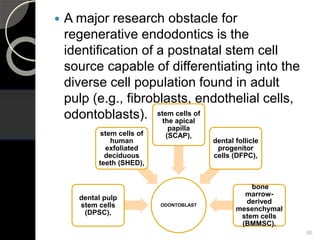
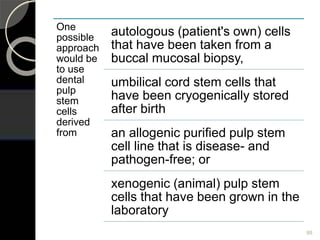
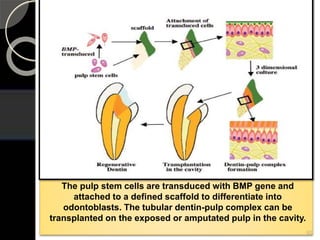
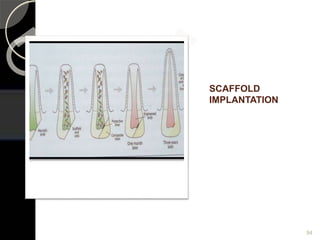
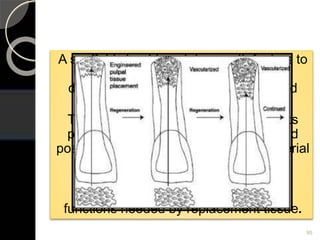
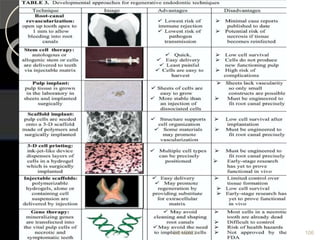
The document outlines regenerative endodontics, focusing on biologically-based procedures aimed at replacing damaged dental structures and promoting tissue regeneration. It details key concepts such as stem cells, tissue engineering, and the historical progress of regenerative techniques, culminating in current practices recognized by the American Dental Association. The document serves as a comprehensive overview of the definitions, objectives, methods, and advancements in the field of regenerative dentistry.