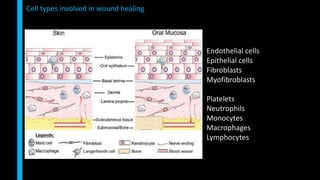
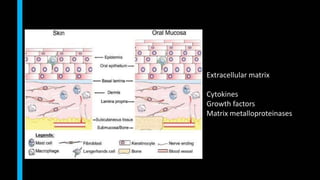
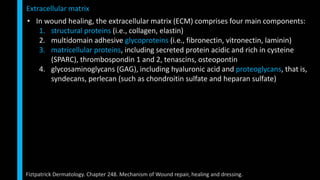
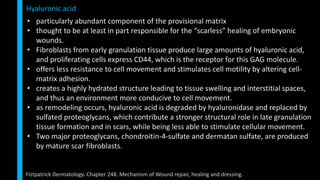
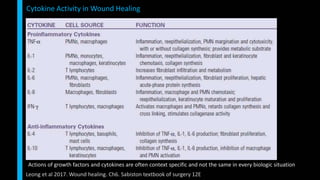
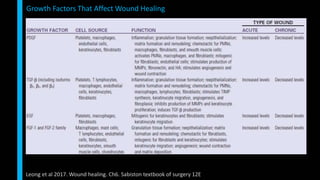
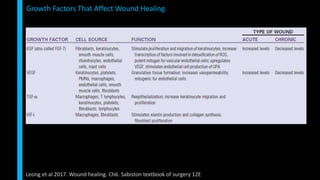
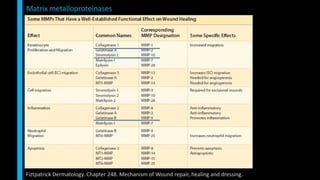
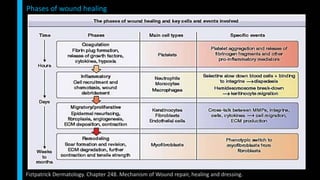
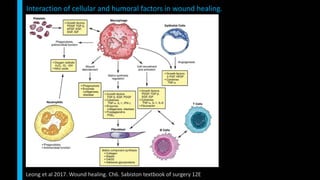
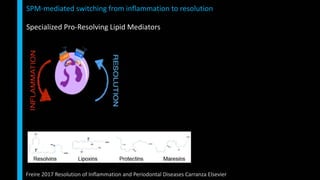
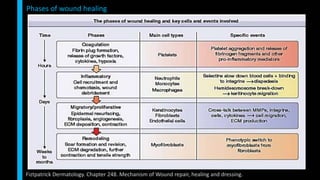
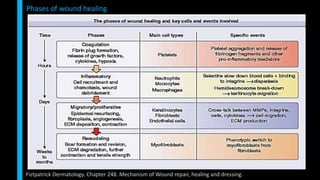
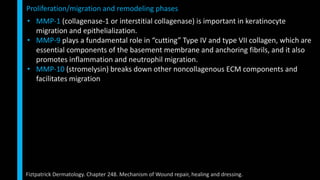
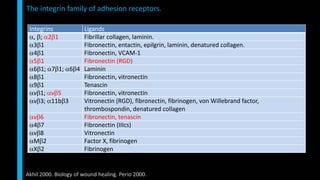
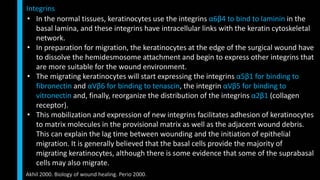
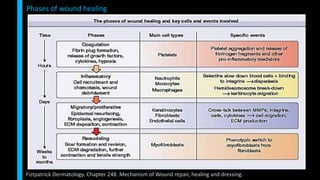
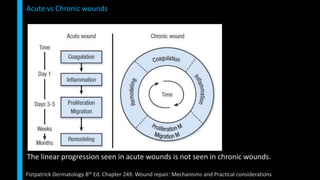
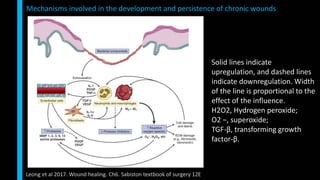
This document summarizes the key cellular and molecular processes involved in soft tissue wound healing. It discusses the cell types involved including endothelial cells, fibroblasts, epithelial cells, platelets, neutrophils, monocytes, macrophages and lymphocytes. It also describes the extracellular matrix components, cytokines, growth factors and matrix metalloproteinases that regulate wound healing. Finally, it outlines the typical phases of wound healing including hemostasis, inflammation, proliferation and remodeling.