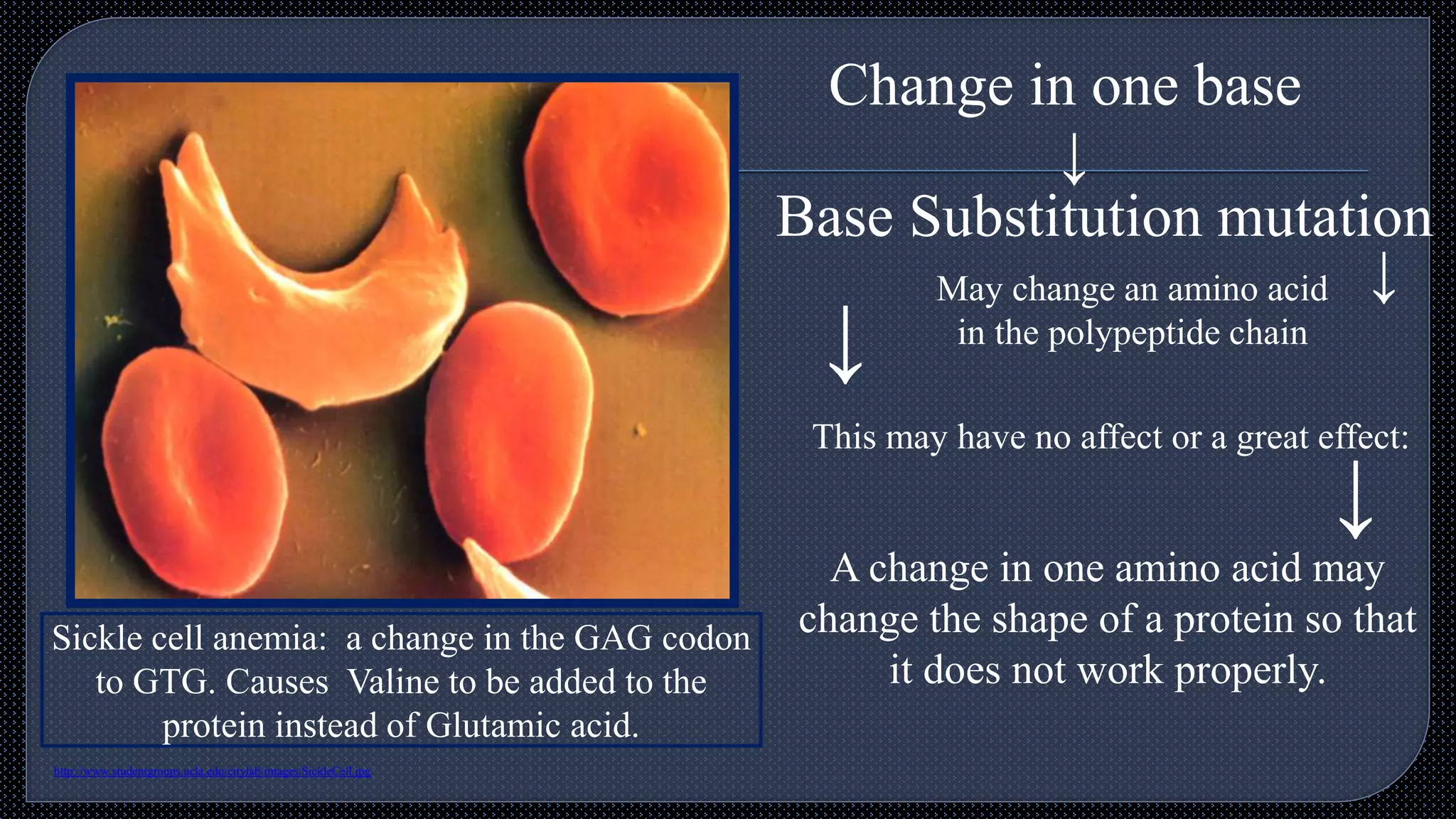
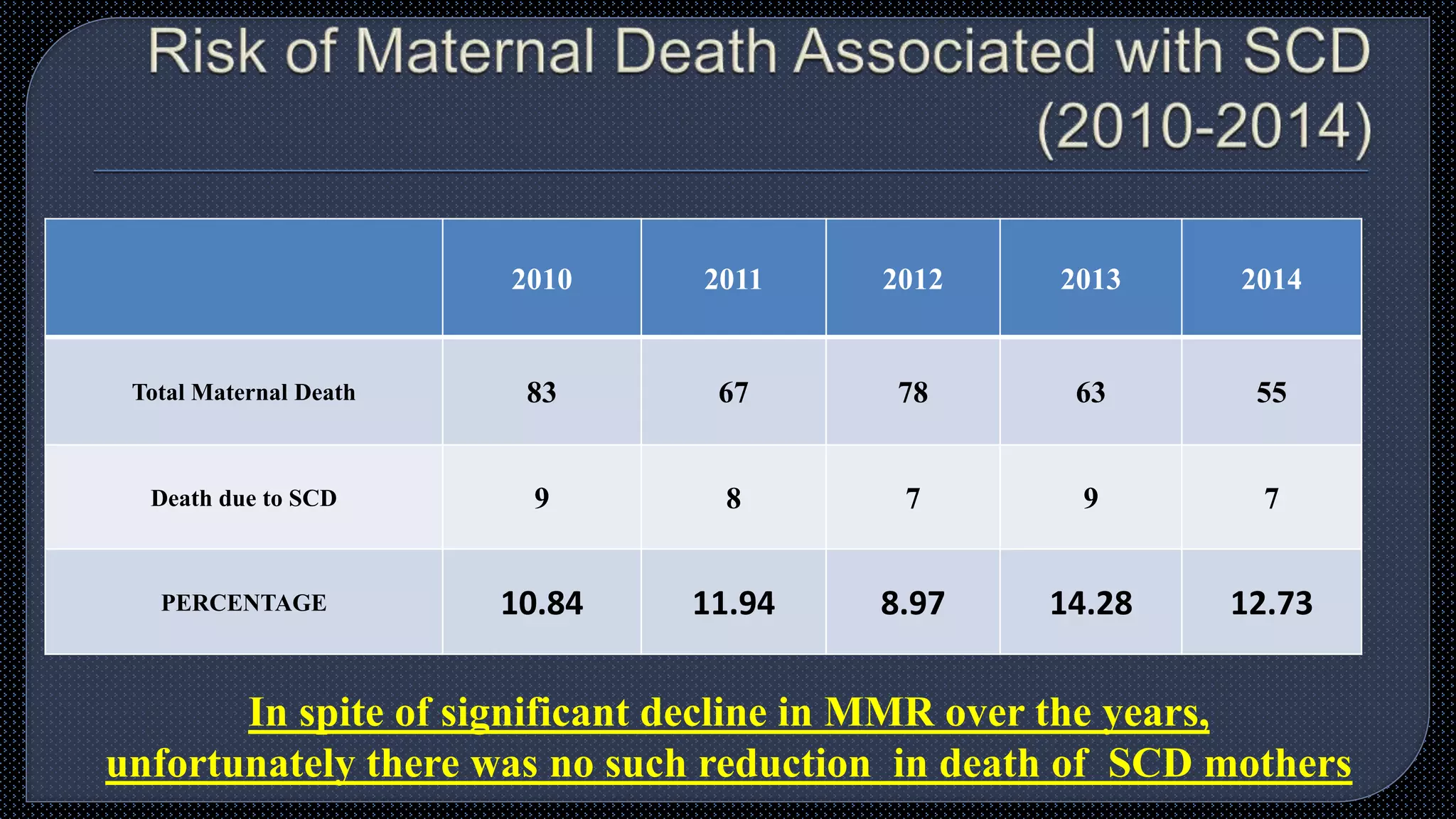
Sickle cell disease (SCD) and thalassemia are major global health issues, particularly in Odisha, India, where approximately 6 lakh individuals are affected. Genetic counseling and education on the inheritance of SCD are crucial for prevention, as many adolescents lack knowledge about the disorder and its implications. Promoting premarital and prenatal screening programs can significantly reduce sickle cell-related maternal deaths and improve health outcomes for future generations.