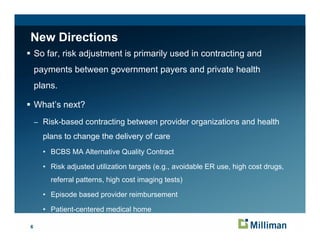
This document summarizes challenges in selecting a risk adjustment system for a new public health program. It discusses whether to use diagnosis-based or pharmacy-based models and whether to adjust for all members or a subset. It also addresses recalibrating existing models for new programs and ensuring proper weighting for members with partial eligibility periods. The document notes that while risk adjustment is not perfect, the benefits include encouraging market participation and competition to potentially lower costs and improve quality of care. It suggests risk-based contracting between health plans and providers may be a future direction for risk adjustment.