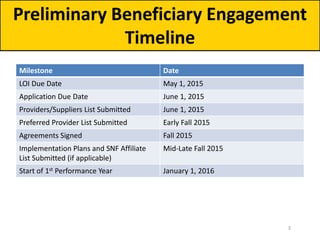
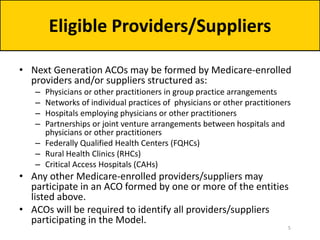
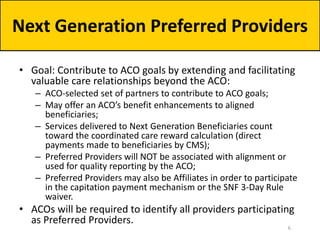
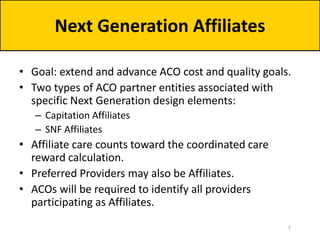
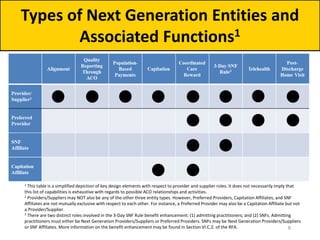
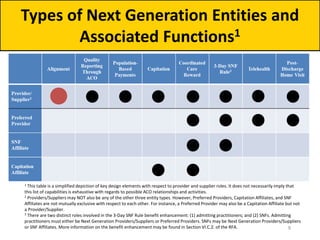
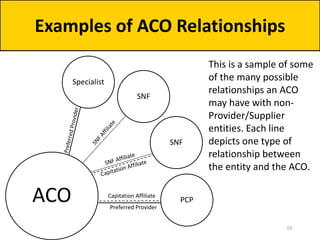
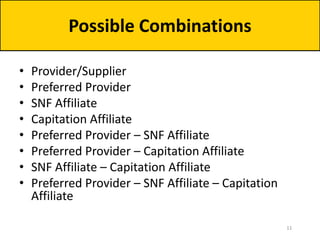
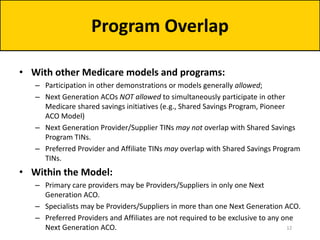
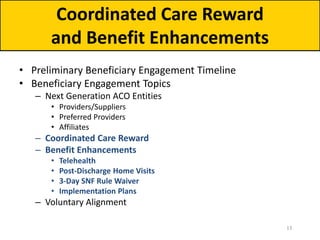
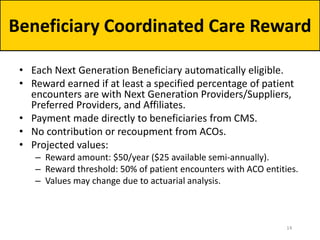
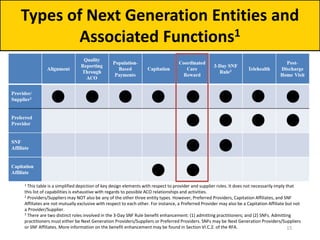
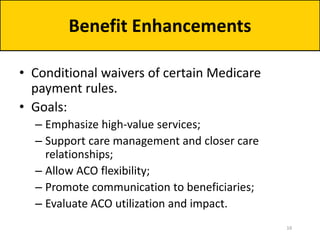
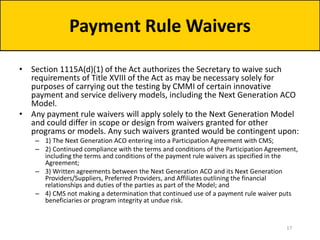
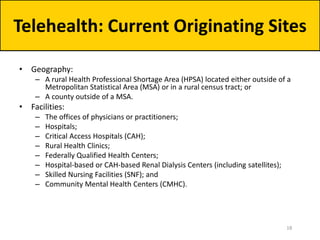
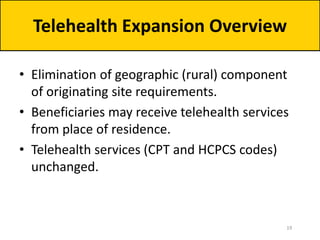
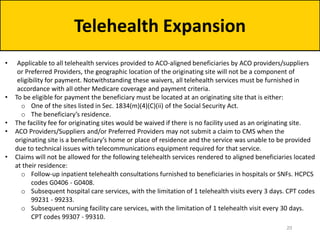
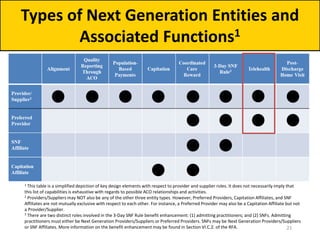
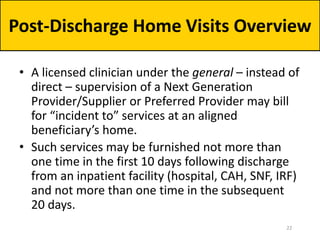
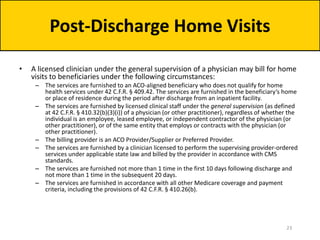
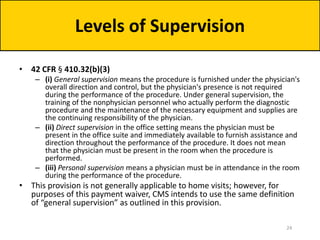
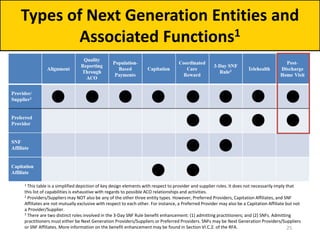
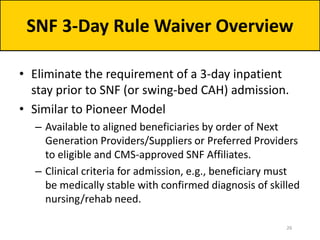
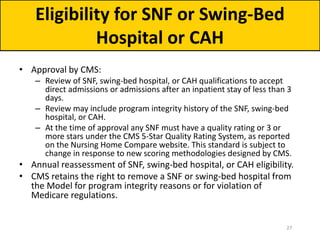
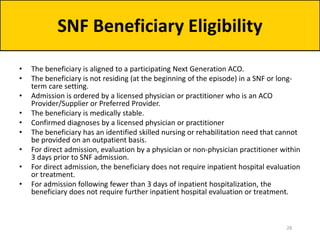
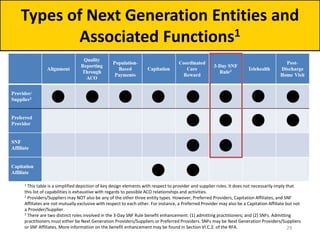
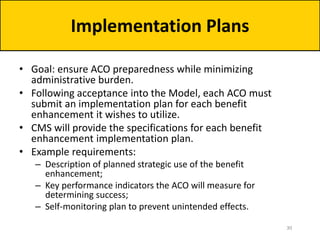
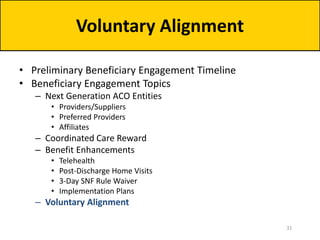
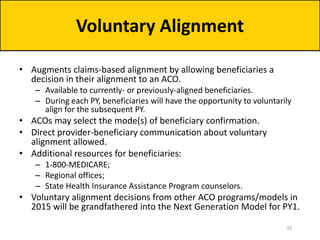
The document outlines the Next Generation Accountable Care Organization (ACO) model, focusing on beneficiary engagement and implementation timelines for 2015. It details the roles of various healthcare providers, including managed care relationships and coordinated care rewards, as well as specific enhancements such as telehealth and post-discharge home visits. Key deadlines for provider applications and agreements leading into the first performance year starting January 1, 2016, are also highlighted.