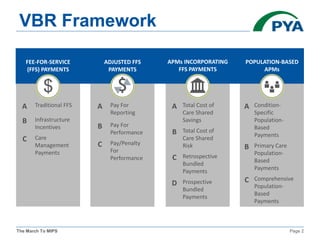
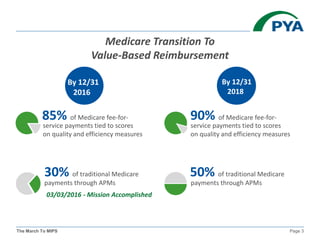
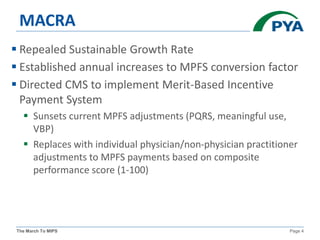
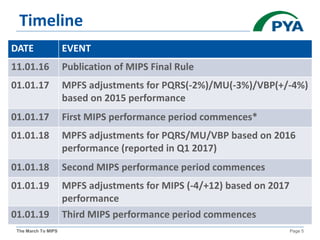
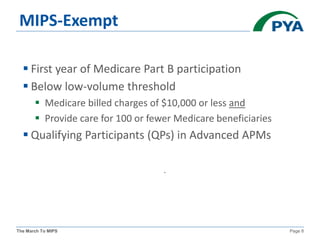
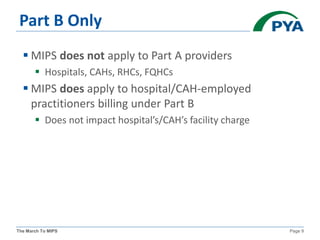
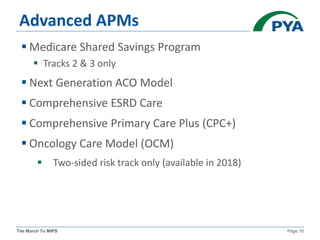
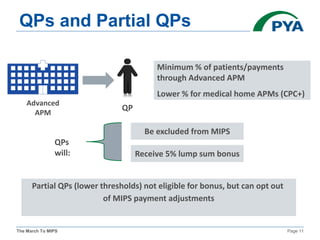
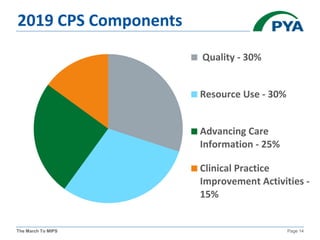
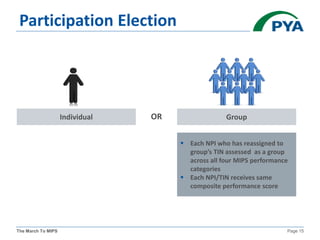
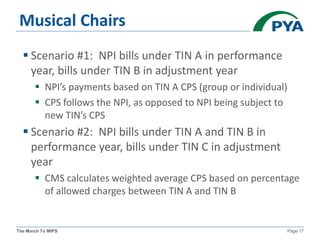
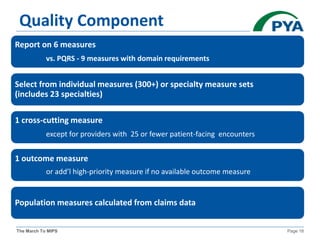
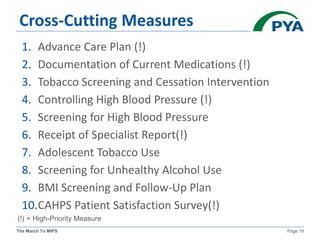
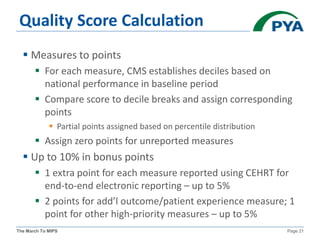
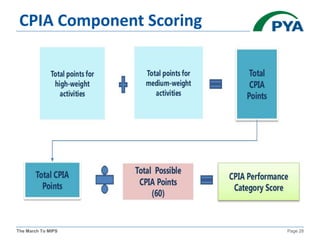
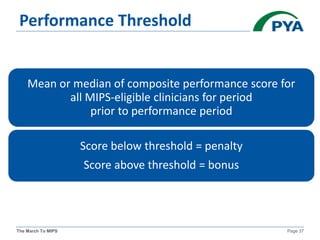
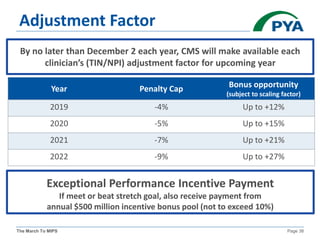
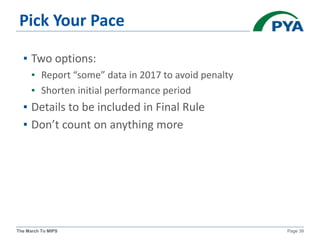
The KMGMA Fall Conference on September 22, 2016, focused on the transition to value-based reimbursement under the MACRA legislation and the implementation of the MIPS proposed rule. Key points included the urgency of adapting to new payment models, awareness levels among physicians regarding MACRA, and the structure and components of MIPS affecting eligible clinicians. The document outlined timelines, scoring components, and compliance measures critical for healthcare providers navigating the changes in Medicare reimbursements.