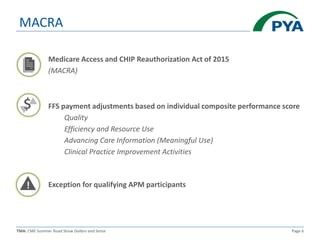
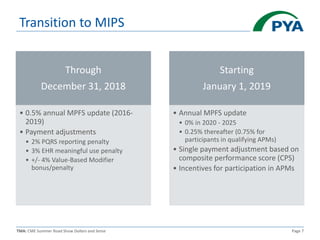
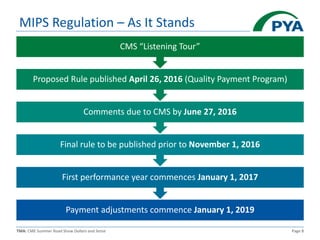
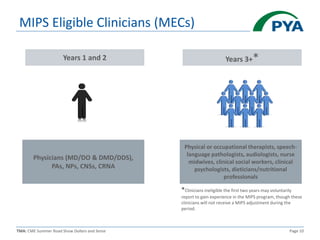
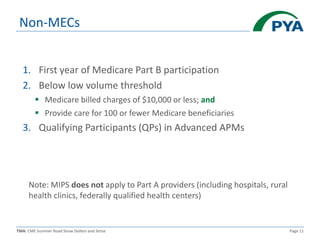
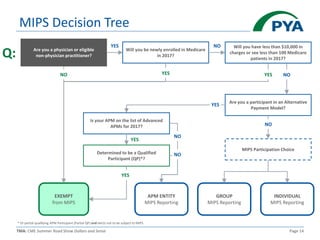
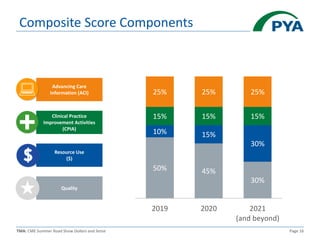
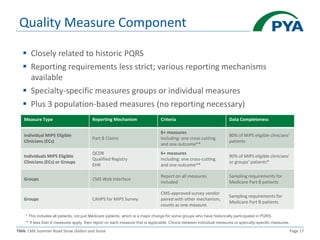
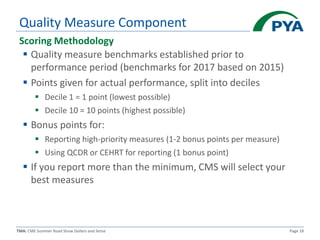
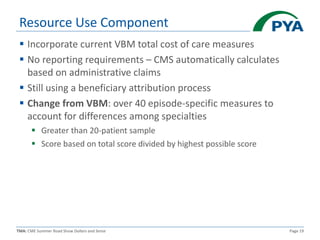
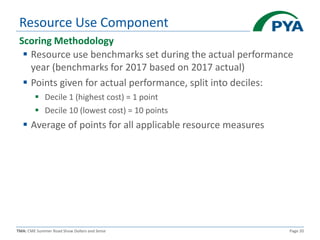
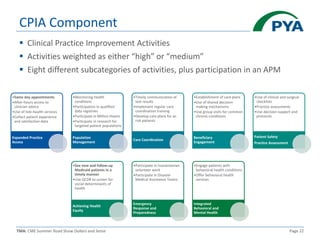
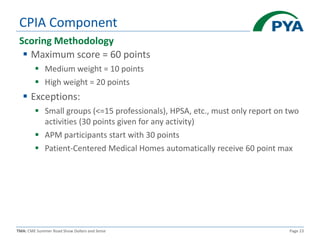
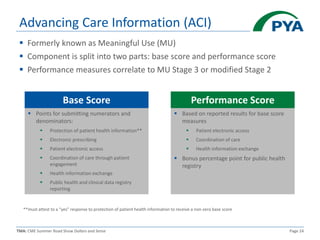
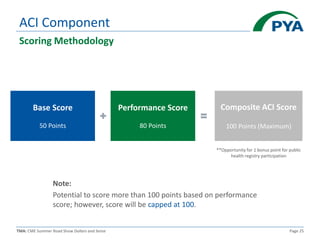
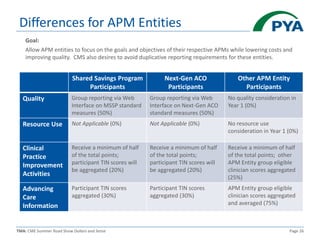
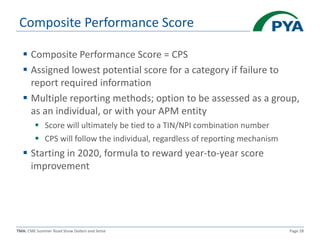
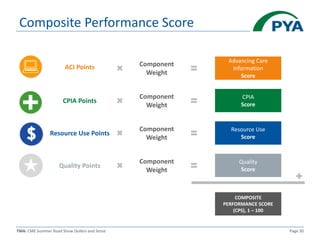
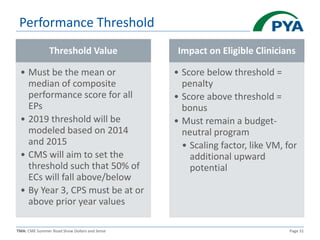
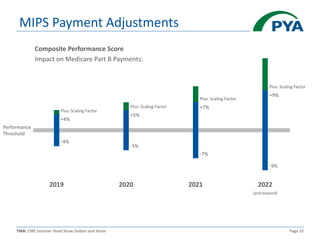
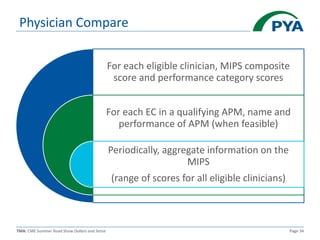
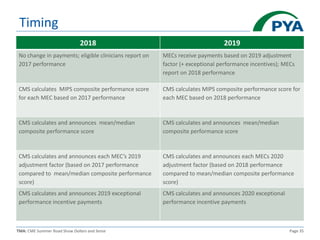
This document provides an overview of the Merit-based Incentive Payment System (MIPS) under the Medicare Access and CHIP Reauthorization Act (MACRA). MIPS replaces previous quality reporting programs and includes four components that determine a Composite Performance Score: Quality, Resource Use, Clinical Practice Improvement Activities, and Advancing Care Information. Scores will determine payment adjustments beginning in 2019, with the potential for bonuses or penalties up to 9% by 2022 based on performance compared to benchmarks and thresholds. The document reviews the scoring methodology and reporting requirements for each MIPS component.