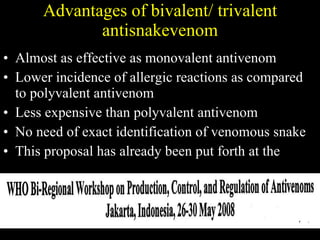
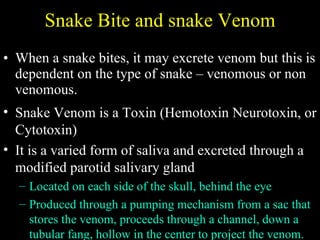
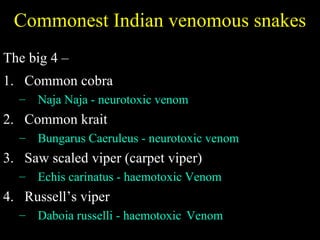
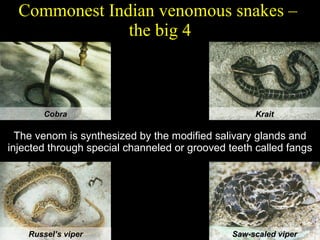
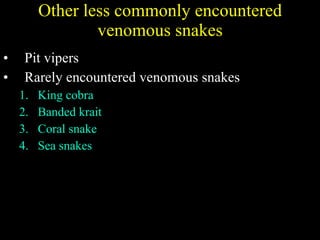
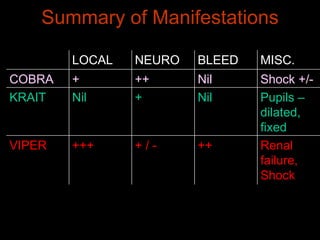
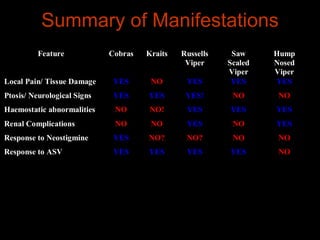
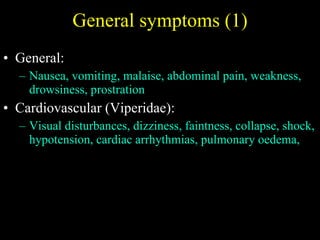
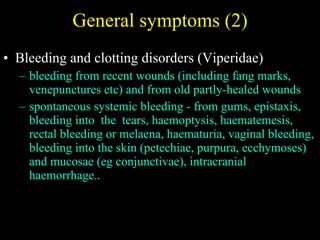
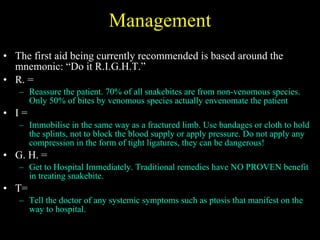
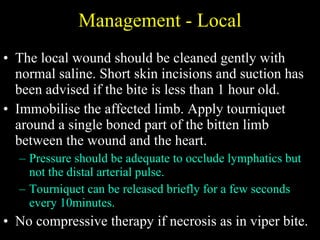
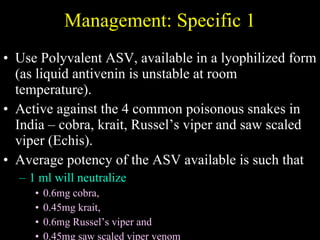
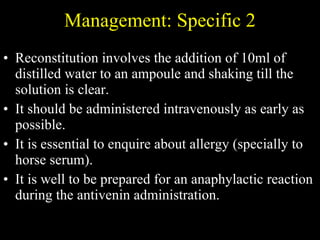
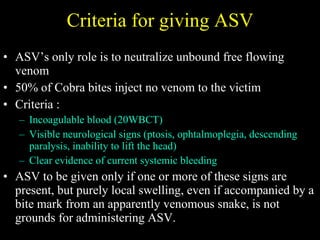
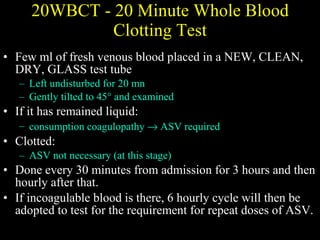
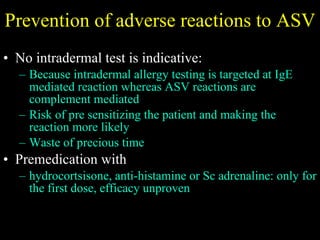
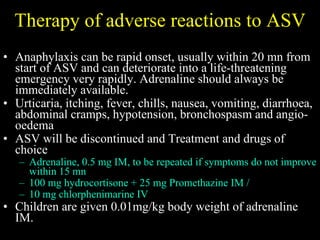
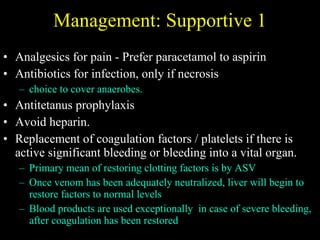
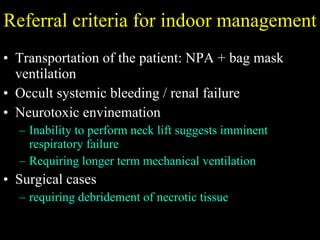
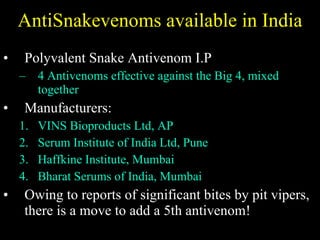
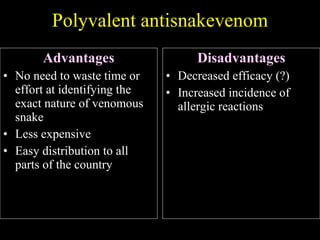
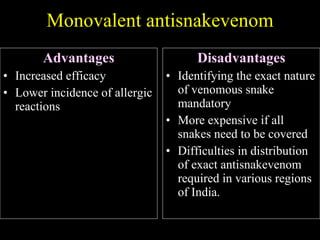
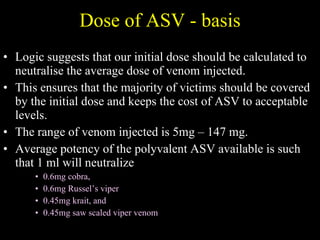
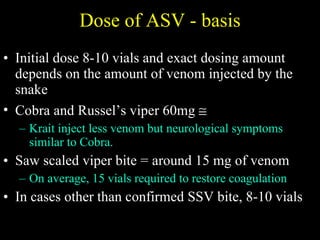
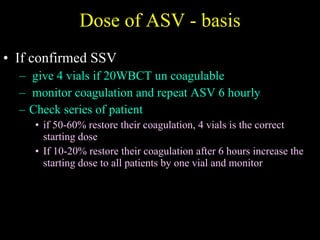
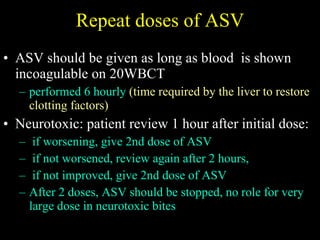
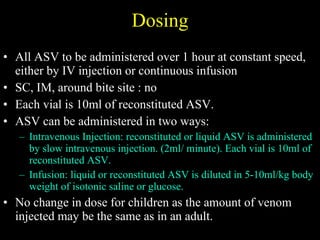
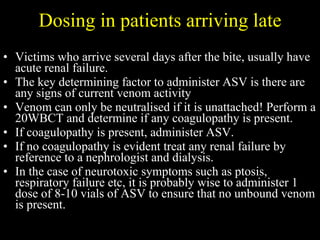
The document discusses various types of snakes found in India and anti-snake venom (ASV) preparations. It provides statistics on snake bites and deaths in India. It describes the types of venom, symptoms, and current treatment guidelines for common venomous snakes like cobras, kraits, Russell's vipers, and saw-scaled vipers. Current ASV therapy involves polyvalent antivenoms effective against these four snakes. Dosing and administration criteria for ASV are outlined.
![Statistics of relevance INDIA Records the highest annual incidence of total snake bites as well as fatal snake bites in the world 2,00,000 bites/year 15,000 deaths/year (some estimates put this at more than 50,000 deaths per year) Number of Indian snake species: 250 [ some say 272] Venomous species: 52](https://image.slidesharecdn.com/snakes1-091108215250-phpapp01/85/Snakes-1-7-320.jpg)
![Neurotoxic Envenomation Cobra venom is a post synaptic neurotoxin and blocks the nicotinic receptor causing acetylcholine to be unable to bind Neostigmine prolongs the life of acetylcholine by inhibiting cholinesterase, increasing the likelywood of acetylcholine binding with unblocked receptor Baseline test: single breath count, time upward gaze 1.5 mg neostigmine + 0.6 mg Atropine [Repeat tests] If objective improvement, repeat neostigmine + atropine every 30 min.](https://image.slidesharecdn.com/snakes1-091108215250-phpapp01/85/Snakes-1-53-320.jpg)