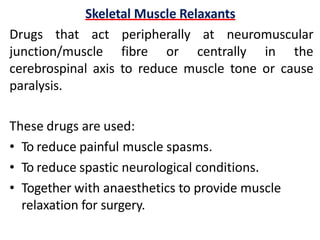
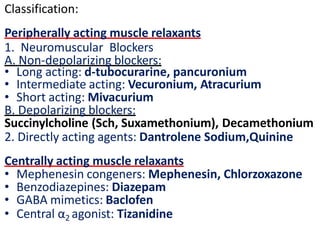
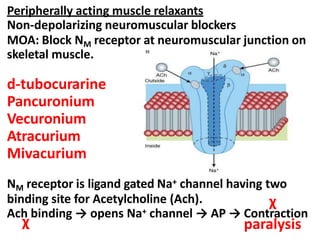
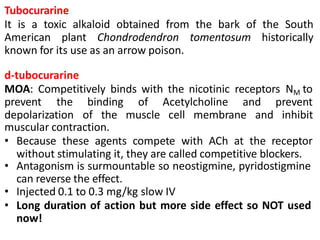
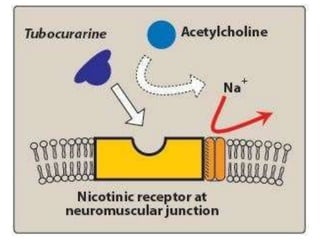
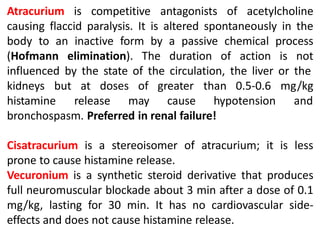
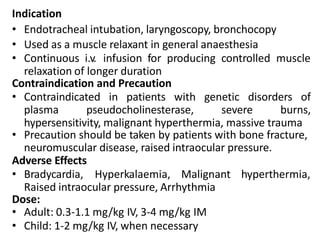
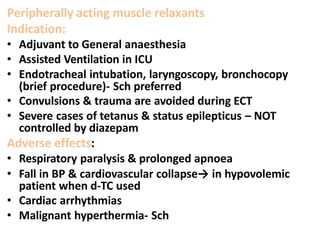
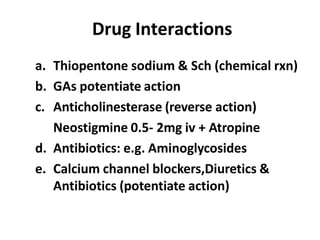
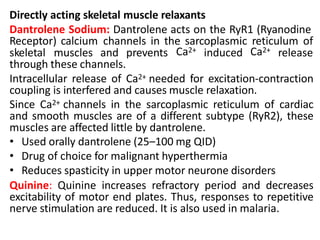
Skeletal muscle relaxants are categorized into peripherally acting and centrally acting agents, used primarily to reduce muscle tone, manage painful spasms, and provide relaxation during surgery. Peripherally acting agents include neuromuscular blockers and directly acting agents such as dantrolene, while centrally acting agents involve drugs like diazepam and baclofen that reduce muscle tone by selectively depressing reflexes in the central nervous system. Each agent has distinct mechanisms, indications, contraindications, and potential adverse effects that need to be carefully considered in clinical use.