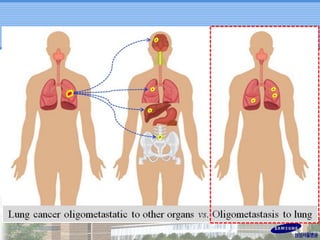
- Oligometastatic disease refers to a limited number of metastases that may be amenable to local treatment.
- Stereotactic body radiation therapy (SBRT) for lung oligometastases from various primary cancers can achieve high rates of local control with minimal toxicity.
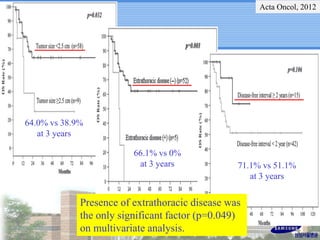
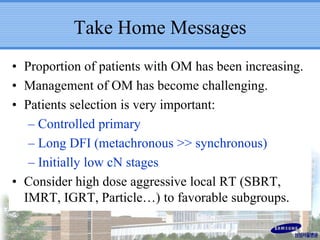
- Patient selection is important, with longer disease-free interval, fewer metastatic sites, and controlled primary tumor associated with improved outcomes after aggressive local therapy of oligometastases.
- Ongoing clinical trials are investigating SBRT for synchronous and metachronous oligometastatic disease to define optimal patient populations and treatment approaches.