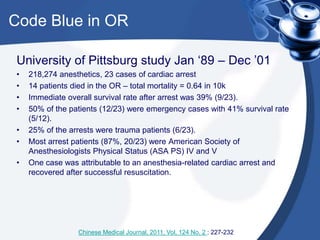
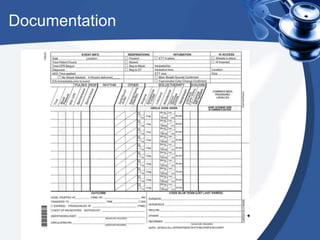
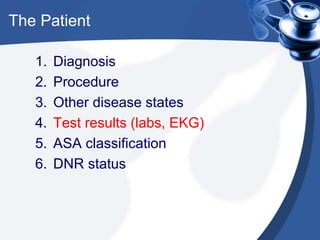
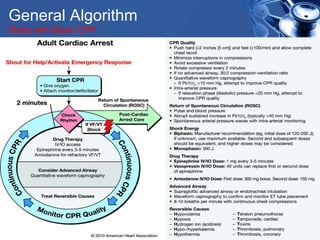
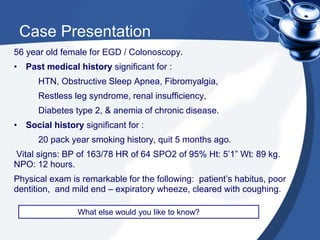
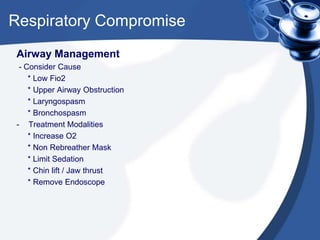
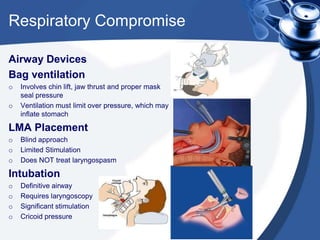
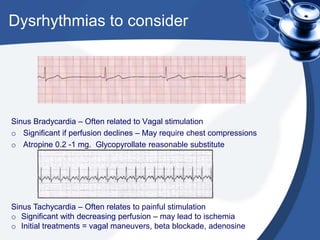
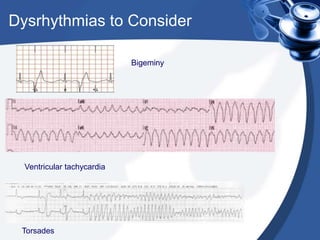
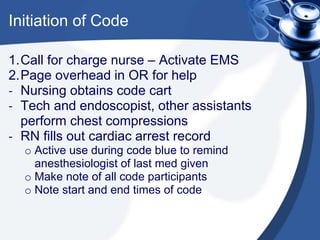
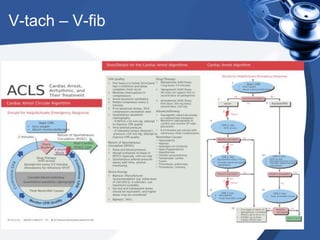
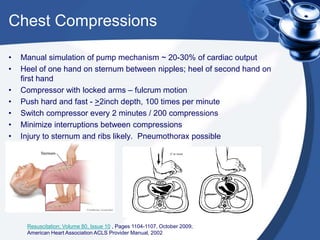
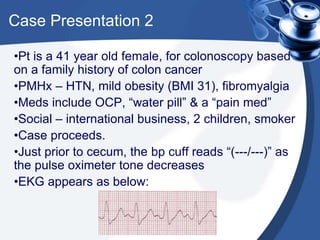
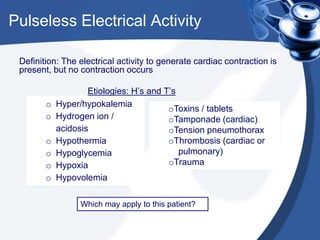
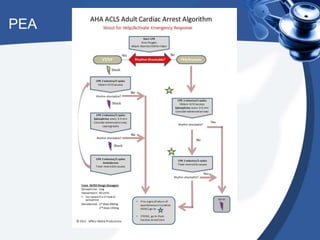
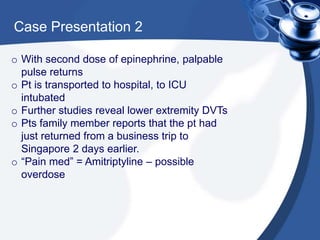
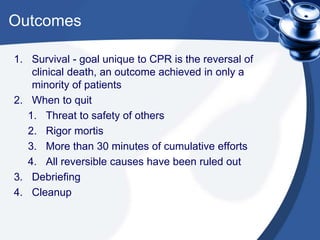
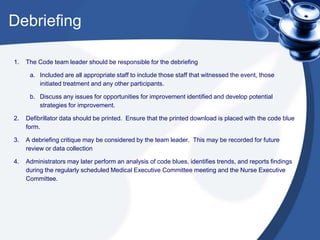
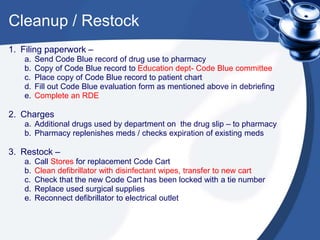
The document provides a comprehensive overview of the procedures and protocols related to managing a 'code blue' incident in the endoscopy suite, which refers to a state of cardiopulmonary arrest. It highlights the importance of preparation, recognizing the potential causes of respiratory compromise or cardiac arrest, and outlines the roles of team members during an emergency. Additionally, it emphasizes ethical considerations, documentation requirements, and post-code debriefing and cleanup processes.