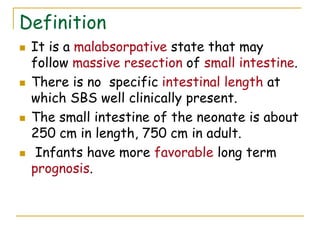
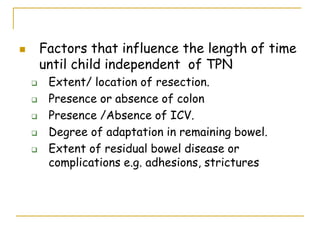
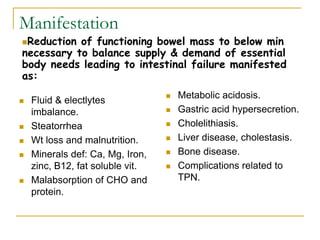
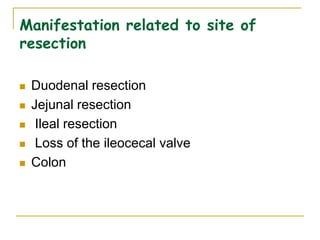
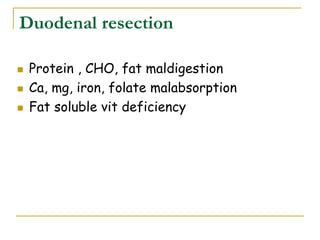
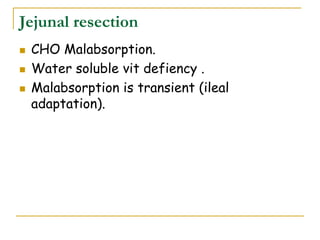
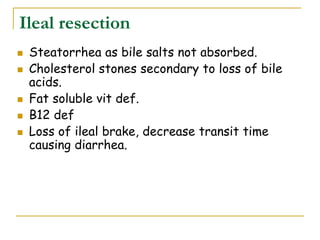
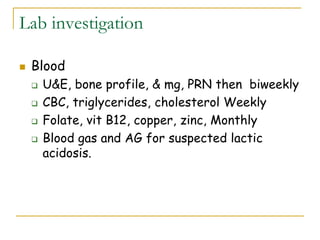
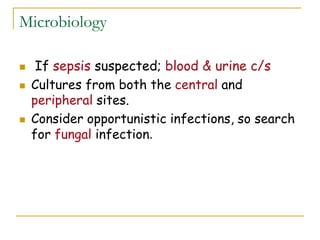
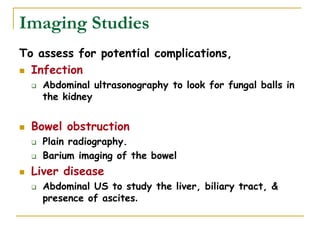
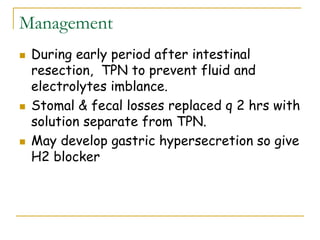
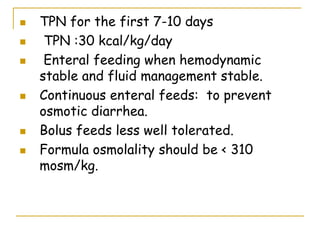
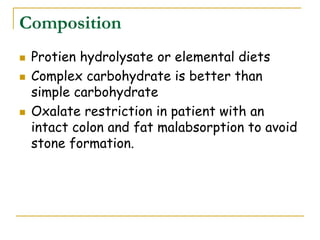
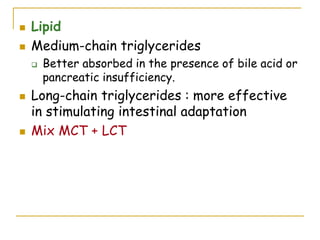
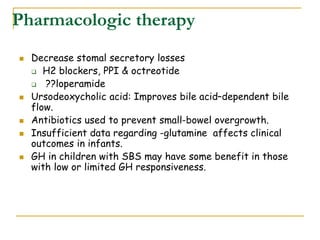
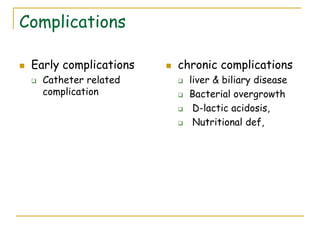
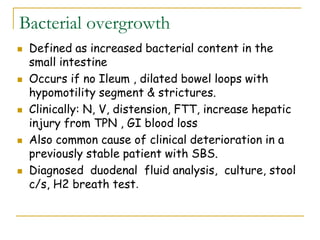
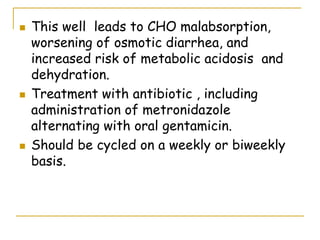
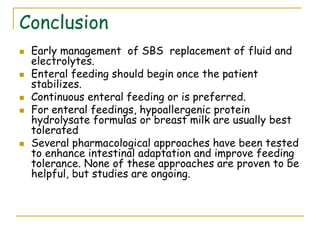
Short bowel syndrome (SBS) is a malabsorptive condition that can arise after extensive small intestine resection, affecting fluid and electrolyte balance, nutrition, and leading to potential complications. Key factors influencing prognosis include congenital anomalies or acquired conditions leading to bowel resection, and management focuses on nutritional support through total parenteral nutrition (TPN) and gradual enteral feeding to promote intestinal adaptation. Long-term success may involve eventual independence from TPN, with surgical interventions considered when necessary.