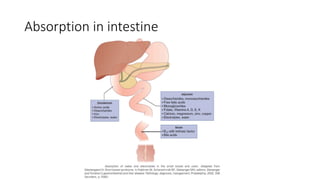
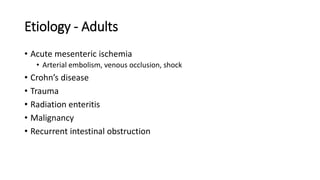
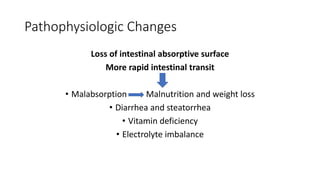
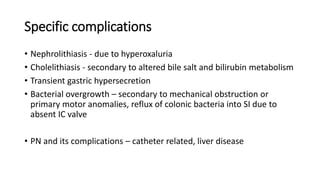
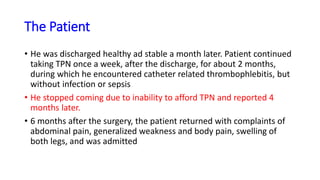
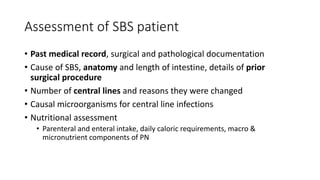
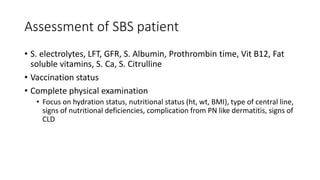
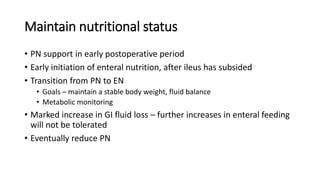
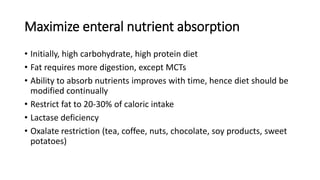
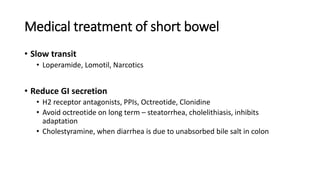
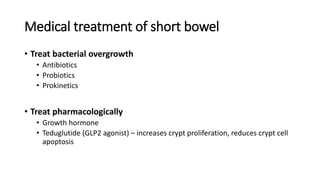
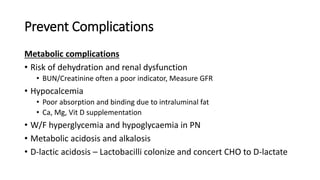
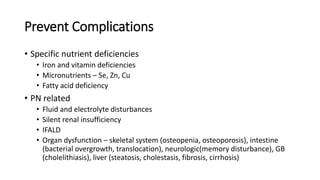
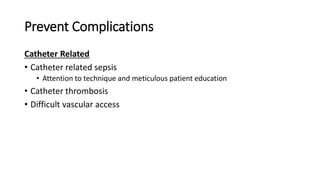
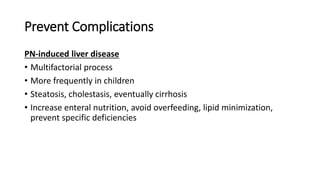
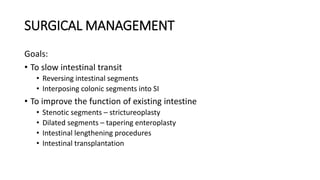
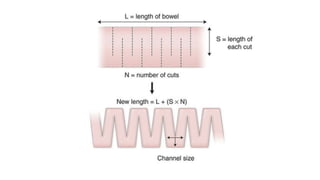
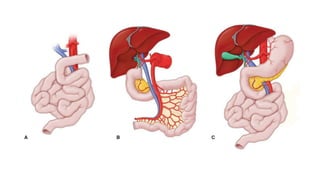
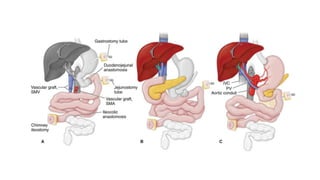
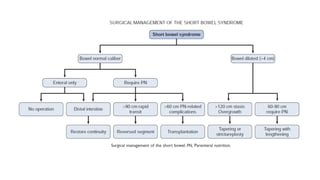
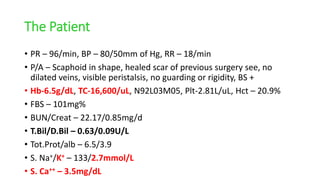
The patient, a 47-year-old man, presented with abdominal pain and shock. Imaging showed occlusion of the SMA and small bowel ischemia requiring resection of the jejunum, ileum, ascending colon and half of transverse colon, leaving only a short remnant. He required TPN, developed complications, and returned months later with new symptoms. Assessment found malnutrition, electrolyte imbalances, and infections. Management of short bowel syndrome focuses on nutrition, maximizing absorption, and preventing complications through medical and surgical interventions.