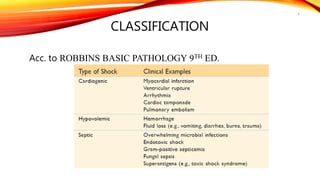
Shock is a complex multi-organ system response to perfusion inadequacy caused by various pathological states. The document outlines clinical features, classifications, pathogenesis, stages, complications, and management strategies of different types of shock. Treatment focuses on restoring adequate tissue perfusion and addressing the underlying causes.