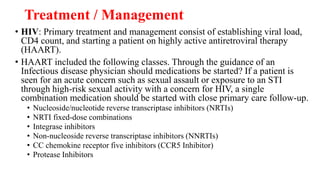
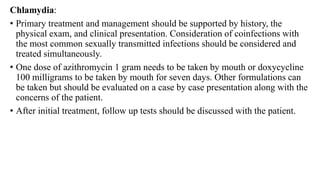
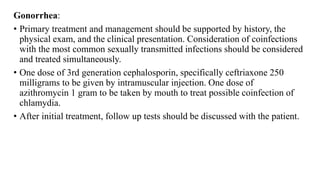
This document provides information about sexually transmitted infections (STIs), including their etiology, epidemiology, pathophysiology, and presentations. It discusses the most common STIs such as HIV, gonorrhea, chlamydia, HPV, syphilis, herpes, and trichomoniasis. STIs are transmitted through sexual contact and can cause infections in the genital area, cervix, urethra, and anus. Physical exams for STIs depend on the suspected infection and may involve inspection for lesions, discharge, or inflammation of affected areas. Providers must understand the various presentations of STIs to properly diagnose, treat, and counsel patients.
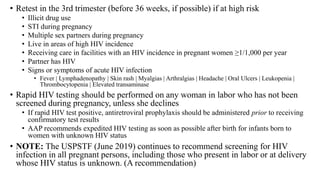
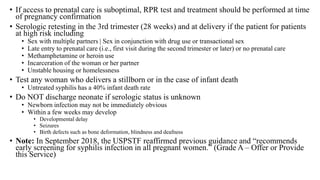
![SYPHILIS
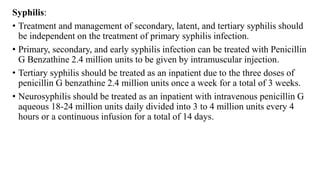
• Serologic tests should be performed at first prenatal visit
• Screening for syphilis infection is a 2-step process | Antepartum screening can be
performed by manual nontreponemal antibody testing (e.g., RPR) by using the
traditional syphilis screening algorithm or by treponemal antibody testing (e.g.,
immunoassays)
• Traditional screening: Initial “nontreponemal” antibody test (ie, Venereal Disease Research
Laboratory test or rapid plasma reagin [RPR] test) to detect biomarkers released from damage
caused by syphilis infection, followed by a confirmatory “treponemal” antibody detection test (ie,
fluorescent treponemal antibody absorption [FTA-ABS] or T pallidum particle agglutination test
[TP-PA])
• Reverse sequence screening algorithm: Automated treponemal test (such as an enzyme-linked
[EIA], chemiluminescence [CIA], or multiplex flow immunoassay [immunoblot]) performed
first, followed by a nontreponemal test
• If the test results of the reverse sequence algorithm are discordant, a second treponemal test (preferably
using a different treponemal antibody) is performed
• Pregnant women with positive treponemal screening tests (e.g., EIA, CIA, or immunoblot)
should have additional quantitative nontreponemal testing because titers are essential for
monitoring treatment response](https://image.slidesharecdn.com/sexuallytransmittedinfections-240320164532-1fdcf228/85/Sexually-Transmitted-Infections-in-gyn-pptx-36-320.jpg)