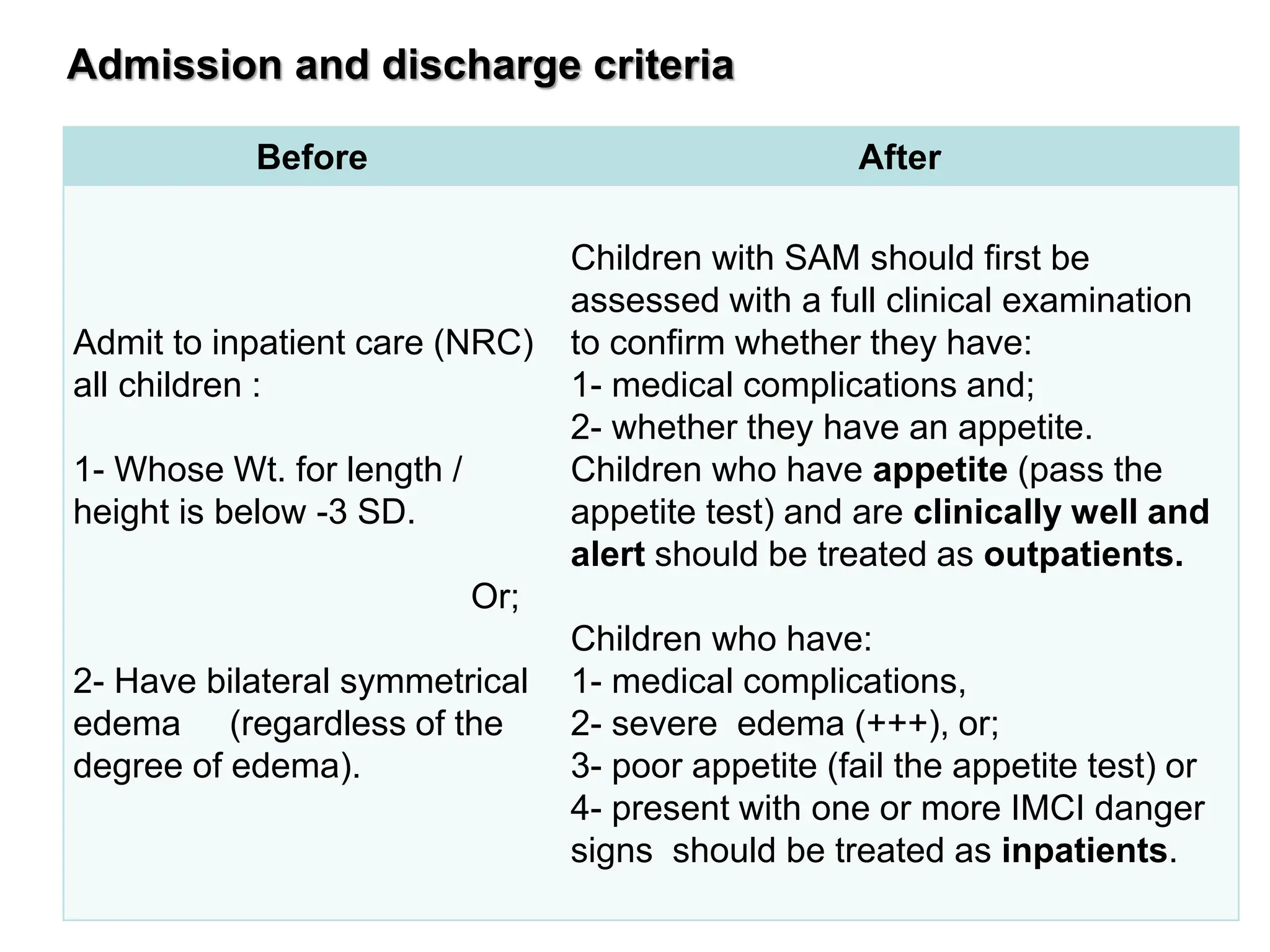
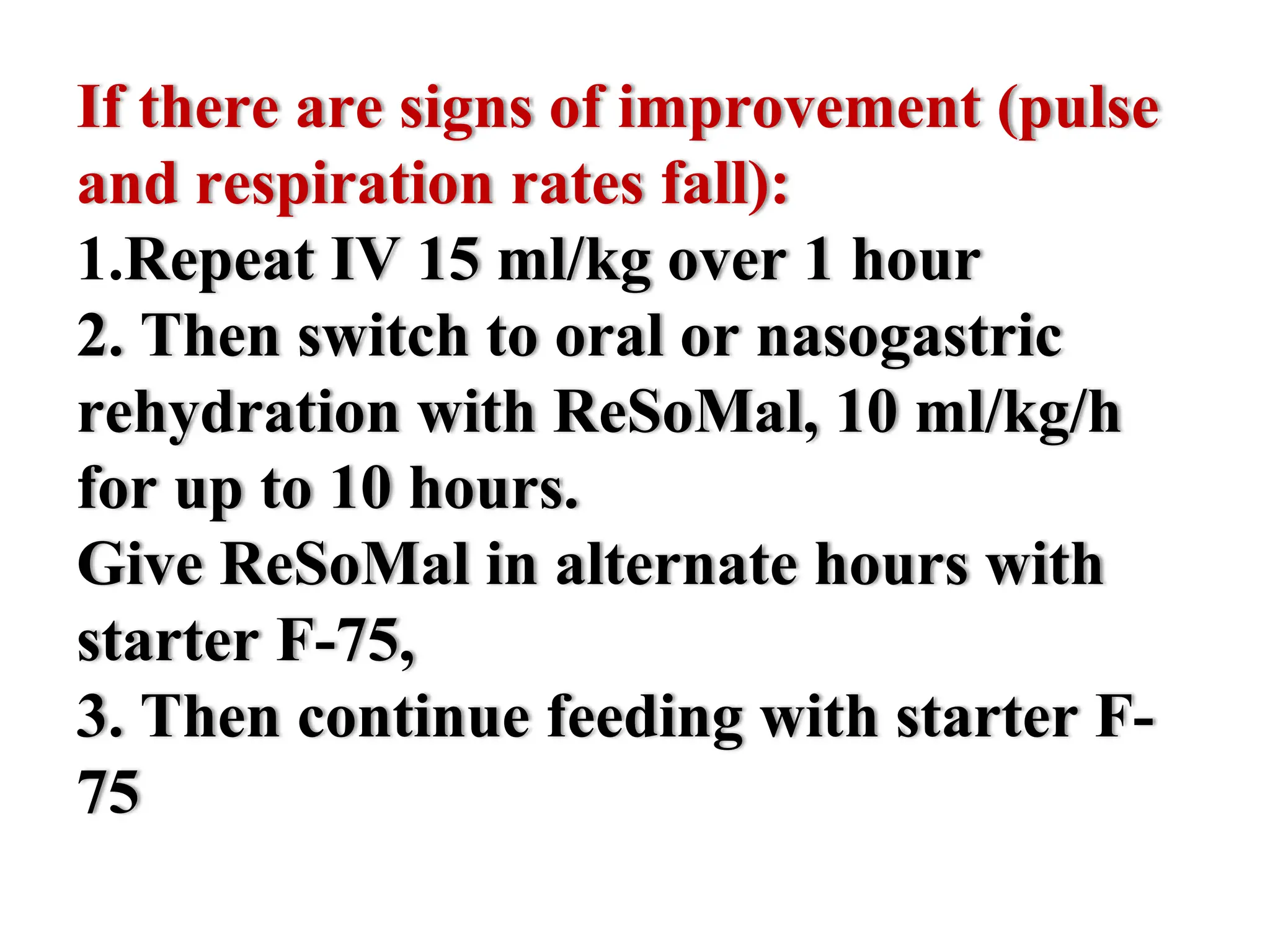
The document discusses the classification, diagnosis, and treatment of severe acute malnutrition. It provides criteria for classifying and admitting patients based on clinical signs and anthropometric measurements. It outlines the initial treatment phase including managing complications like hypoglycemia, hypothermia, dehydration, and infections. The treatment principles aim to progressively refeed patients while avoiding electrolyte imbalances or other dangers during the reductive adaptation period. A case study is presented and guidelines are provided for assessing and managing its complications.