Malnutrition Types, Causes, and Management
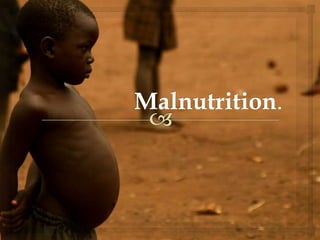
- 3. MALNUTRITION WHO defines Malnutrition as "the cellular imbalance between the supply of nutrients and energy and the body's demand for them to ensure growth, maintenance, and specific functions.“ Malnutrition is the condition that develops when the body does not get the right amount of the vitamins, minerals, and other nutrients it needs to maintain healthy tissues and organ function. Definitions
- 4. PROTEIN ENERGY MALNUTRITION It is a group of body depletion disorders which include kwashiorkor, marasmus and the intermediate stages MARASMUS Represents simple starvation . The body adapts to a chronic state of insufficient caloric intake KWASHIORKOR It is the body’s response to insufficient protein intake but usually sufficient calories for energy
- 5. Protein-Energy Malnutrition PEM is also referred to as protein-calorie malnutrition. It is considered as the primary nutritional problem. Also called the 1st National Nutritional Disorder. The term protein-energy malnutrition (PEM) applies to a group of related disorders that include marasmus, kwashiorkor, and intermediate states of marasmus-kwashiorkor. PEM is due to “food gap” between the intake and requirement.
- 6. Malnutrition is a special health problem, especially in developing countries. 95 % of all malnourished peoples living in the sub- tropics and tropics. More than 70% of children with PEM live in Asia and 26% in Africa, and 4% in Latin America and the Caribbean (WHO).
- 7. Malnutrition is by far the biggest contributor to child mortality: 49% of the 10.4 million deaths occurring in children younger than 5 years in developing countries are associated with PEM. 6 million children die of hunger every year.
- 8. AETIOLOGY: Different aetiological factors can lead to PEM in children. They are: Social and Economic Factors Biological factors Environmental factors Role of Free Radicals Age of the Host
- 9. Amongst the Social, Economic, Biological and Environmental Factors the common causes are: Lack of breast feeding and giving diluted formula Improper complementary feeding Over crowding in family Ignorance Illiteracy Lack of health education Poverty Infection Familial disharmony
- 10. Role of Free Radicals : Two new theories have been postulated recently to explain the pathogenesis of kwashiorkor. These include Free Radical Damage to liver cells giving rise to kwashiorkor. Age Of Host : Frequent in Infants & young children whose rapid growth increases nutritional requirement. PEM in pregnant and lactating women can affect the growth, nutritional status & survival rates of their fetuses, new born and infants. Elderly can also suffer from PEM due to alteration of GI System
- 11. Leading cause of death (less than 5 years of age) Primary PEM: Protein + energy intakes below requirement for normal growth. Secondary PEM: the need for growth is greater than can be supplied. decreased nutrient absorption increase nutrient losses Linear growth ceases Static weight Weight loss Wasting Malnutrition and its signs AETIOLOGY of PEM:
- 12. CLASSIFICATIONS
- 13. Height for Age: It is a measure of linear growth, and deficit represents the cumulative impact of adverse events, that ultimately results in stunting or chronic malnutrition. H/A: (Ht of child/Ht of normal child of same age) × 100. INDICATORS OF PEM.
- 14. Weight for Height: Low weight for height indicates Acute Malnutrition. W/H: (Wt of child/Wt of normal child of same height) × 100 Weight for Age: W/A: (Wt of child/Wt of normal child of same age) × 100 Mid Upper Arm Circumference: Used for screening wasted childrens.
- 15. Body mass Index: It is a screening tool for thinness,overweight and obesity. BMI= Weight in Kg/square of height in meters. Z score: It is the child’s height minus the median height for the age and sex of the child divided by relevant standard deviation.
- 16. GOMEZ CLASSIFICATION In this weight is assessed at various ages by standard weight chart. 1st degree 75-90%of expected wt 2nd degree 60-75%of expected wt 3rd degree <60% of expected wt.
- 18. HARVARD CLASSIFICATION. Childs wt=50th percentile is healthy and is taken as 100%. Between 80-100%of 50th percentile is healthy child <80%malnourished Grade 1 71-80%of 50th percentile Grade 2 61-70%of 50th percentile Grade 3 51-60%of 50th percentile Grade 4 <50%of 50th percentile
- 19. WELCOME CLASSIFICATION. Weight for Age Edema present. Edema absent. 80-60% of standard. Kwashiorkor Ponderal retardation < 60 % of standard. Marasmic Kwashiorkor Marasmus
- 20. WATERLOW CLASSIFICATION. A system for classifying protein‐energy malnutrition in children based on wasting (the percentage of expected weight for height) and the degree of stunting (the percentage of expected height for age.
- 21. MID UPPER ARM CIRCUMFERENCE. Community based screening programs for severe malnutrition usually use MUAC less than 12cm to identify severe wasting.
- 22. SKIN FOLD THICKNESS. Special calipers (Herpenden) in the region of triceps or back of shoulder Normal 9-11 mm Malnourished <9mm It is for index of body wt.
- 23. UDANI CLASSIFICATION. GRADES LOSS OF FAT I BUTTOCK II AXILLA/GROIN III ABDOMEN,CHEST,BACK IV BUCCAL PAD OF FAT
- 24. KANAWATI INDEX.
- 25. COLE CLASSIFICATION. Z-scores of BMI for age. GRADE BMI FOR AGE Z SCORE Grade I Z score < -1 Grade II Z score < -2 Grade III Z score < -3
- 27. WHO CLASSIFICATION. PARAMETERS MODERATE SEVERE EDEMA ABSENT PRESENT WEIGHT/HEIGHT Z SCORE -2 to -3 Z SCORE < -3 HEIGHT/AGE Z SCORE -2 to -3 Z SCORE < -3
- 31. Definition. It is defined as severe wasting and/or bilateral edema. Severe wasting is extreme thinness diagnosed by weight for height below -3 SD Severe malnutrition is one of the most common causes of morbidity and mortality among children under the age of 5 years worldwide.
- 32. Clinical Signs.
- 33. Reductive Adaptation System The systems of the body begin to “shut down” with severe malnutrition. The systems slow down and do less in order to allow survival on limited calories. This slowing down is known as reductive adaptation. As the child is treated, the body's systems must gradually "learn" to function fully again. Rapid changes (such as rapid feeding or fluids) would overwhelm the systems, so feeding must be slowly and cautiously increased.
- 34. Reductive adaptation affects treatment of the child in 3 ways. 1- Presume and treat infection Nearly all children with severe malnutrition have bacterial infections. However, as a result of reductive adaptation, the usual signs of infection may not be apparent, because the body does not use its limited energy to respond in the usual ways, such as inflammation or fever.
- 35. 2.Iron Due to reductive adaptation, the severely malnourished child makes less haemoglobin than usual. Iron that is not used for making haemoglobin is put into storage. Giving iron early in treatment can also lead to “free iron” in the body. Free iron can cause problems in three ways: Free iron is highly reactive and promotes the formation of free radicals with damaging effects. Free iron promotes bacterial growth and can make some infections worse. The body tries to protect itself from free iron by converting it to ferritin. This conversion requires energy and amino acids and diverts these from other critical activities
- 36. 3. Provide potassium and restrict sodium In reductive adaptation, the “pump” that usually controls the balance of potassium and sodium runs slower. As a result, the level of sodium in the cells rises and potassium leaks out of the cells and is lost. ReSoMal has less sodium and more potassium than regular ORS.
- 37. MANAGEMENT. WHO recommends that children be kept in the severe malnutrition ward or area until they reach −1 SD (90%) weight-for-height.
- 38. MANAGEMENT.
- 40. HYPOGLYCEMIA. In severely malnourished children, the level considered low is less than (<) 3 mmol/litre (or <54 mg/dl). If the child can drink, give the 50 ml bolus of 10% glucose orally. If the child is alert but not drinking, give the 50 ml by NG tube.
- 41. HYPOGLYCEMIA. If the child is lethargic, unconscious, or convulsing, give 5 ml/kg body weight of sterile 10% glucose by IV, followed by 50 ml of 10% glucose by NG tube. If the IV dose cannot be given immediately, give the NG dose first. Start feeding F-75 half an hour after giving glucose , during the first 2 hours. If the child’s blood glucose is not low, begin feeding the child with F-75 right away. Feed the child every 2 hours, even during the night.
- 42. HYPOTHERMIA. Actively re-warm the hypothermic child: keeping the child covered keeping the room warm, Have the mother hold the child with his skin next to her skin when possible (kangaroo technique), and cover both of them. Keep the child’s head covered. Monitor temperature hourly. Stop rewarming when rectal temperature is 36.5 C
- 43. SHOCK MANAGEMENT. The severely malnourished child is considered to have shock if he/she: is lethargic or unconscious and has cold hands plus either: slow capillary refill (longer than 3 seconds),or weak fast pulse.
- 44. SHOCK MANAGEMENT. Give oxygen. Give sterile 10% glucose 5 ml/kg by IV. Infuse IV fluid at 15ml/kg over 1 hour. Use 0.45% (half-normal) saline with 5% glucose). Observe the child and check respiratory and pulse rates every 10 minutes.
- 45. SHOCK MANAGEMENT. If respiratory rate and pulse rate are slower after 1 hour, the child is improving. stop the IV. If the respiratory rate and pulse rate increase Repeat the same amount of IV fluids for another hour. Continue to check respiratory and pulse rates every 10 minutes. After 2 hours of IV fluids, switch to oral or nasogastric rehydration with ReSoMal (special rehydration solution for children with severe malnutrition).
- 46. SHOCK MANAGEMENT. Give 5 − 10 ml/kg ReSoMal in alternate hours with F- 75 for up to 10 hours. Leave the IV line in place in case it is needed again. If the child fails to improve after the Second hour of IV fluids, then assume that the child has septic shock. Give maintenance IV fluids (4 ml/kg/hour) while waiting for blood. When blood is available, stop all oral intake and IV fluids, give a diuretic to make room for the blood, and then transfuse whole fresh blood at 10 ml/kg slowly over 3 hours.
- 47. ANEMIA MANAGEMENT. Mild or moderate anaemia is very common in severely malnourished children and should be treated later with iron, after the child has stabilized. Very severe anaemia If haemoglobin is less than 40 g/l, give a blood transfusion. If there are no signs of congestive heart failure, transfuse whole fresh blood at 10 ml/kg slowly over 3 hours. If there are signs of heart failure, give 5 – 7 ml/kg packed cells over 3 hours instead of whole blood. Give a diuretic; Furosemide (1 mg/kg, given by IV)
- 48. CORNEAL ULCERATION. All severely malnourished children need vitamin A on Day 1. Additional doses are given if: the child has signs of eye infection, measles , clinical signs of vitamin A deficiency. The additional doses are given on Day 2 and at least 2 weeks later, preferably on Day 15.
- 49. Manage watery diarrhea and/or vomiting with ReSoMal. ReSoMal is Rehydration Solution for Malnutrition. It is a modification of the standard Oral Rehydration Solution (ORS) recommended by WHO. ReSoMal contains less sodium, more sugar, and more potassium than standard ORS For children < 2 years, give 50 − 100 ml after each loose stool. For children 2 years and older, give 100 − 200 ml after each loose stool. It should be given by mouth or by nasogastric tube. If the child develops a hard distended abdomen with very little bowel sound, give 2 ml of a 50% solution of magnesium sulphate IM
- 50. RESOMAL. 1 packet ORS 2 L water 50 g sucrose 40 ml mineral solution COMPOSITION RESOMAL Na 45 Cl 70 K 40 GLUCOSE 125 OSMOLALITY 300
- 51. INFECTION MANAGEMENT. Give all severely malnourished children antibiotics for presumed infection.
- 52. ELECTROLYTE IMBALANCE. Give extra potassium (4mmol/kg/day). Give extra magnesium (0.6 mmol/kg/day). These should be given for atleast 2 weeks.
- 53. MICRONUTRIENT DEFICIENCIES. Give vitamin A. Folic acid 1 mg. Zinc and copper(0.3mg/kg/day). Multivitamin syrup.
- 54. FEEDING F75 & F 100.
- 55. Determine frequency & Amount of feeds. Feed orally . Use an NG tube if the child : does not take 80% of the feed (i.e., leaves more than 20%) for 2 or 3 consecutive feeds. Remove the NG tube when the child takes: 80% of the day’s amount orally; or two consecutive feeds fully by mouth.
- 56. . On the first day, feed the child a small amount of F-75 every 2 hours (12 feeds in 24 hours, including through the night). If the child is hypoglycaemic, give ¼ of the 2-hourly amount every half-hour for the first 2 hours or until the child’s blood glucose is at least 3 mmol/l. After the first day, increase the volume per feed gradually so that the child's system is not overwhelmed. The child will gradually be able to take larger, less frequent feeds (every 3 hours or every 4 hours).
- 57. Determine amount of F-75 needed per feed.
- 58. . Criteria for increasing volume/decreasing frequency of feeds: If little or no vomiting, modest diarrhea (for example, less than 5 watery stools per day), and finishing most feeds, change to 3-hourly feeds. After a day on 3-hourly feeds: If no vomiting, less diarrhea, and finishing most feeds, change to 4- hourly feeds.
- 59. Adjusting to F-100 during transition, or feeding freely on F-100. Look for the following signs of readiness usually after 2 − 7 days: Return of appetite (easily finishes 4-hourly feeds of F 75) Reduced oedema or minimal oedema The child may also smile at this stage
- 60. . Begin giving F-100 slowly and gradually: Transition takes 3 days. First 48 hours (2 days): Give F-100 every 4 hours in the same amount as you last gave F-75. Do not increase this amount for 2 days. Then, on the 3rd day: Increase each feed by 10 ml as long as the child is finishing feeds. Continue increasing the amount until some food is left after most feeds (usually when amount reaches about 30 ml/kg per feed). If the child is breastfeeding, encourage the mother to breastfeed between feeds of F-100.
- 61. Rehabilitation" phase . After transition, the child is in the "rehabilitation" phase and can feed freely on F-100 to an upper limit of 220 kcal/kg/day. (This is equal to 220 ml/kg/day.) , give iron daily, Calculate and administer the amount needed: Give 3 mg elemental Fe/kg/day in 2 divided doses. Always give iron orally, never by injection. Preferably give iron between meals using a liquid preparation.
- 62. Monitor individual patient progress and care:. Good weight gain: 10 g/kg/day or more Moderate weight gain: 5 up to10 g/kg/day Poor weight gain: Less than 5 g/kg/day
- 63. Criteria for failure to respond to treatment. Primary failure to respond: Failure to regain appetite Day 4 Failure to start to lose oedema Day 4 Oedema still present Day 10 Failure to gain at least 5 g/kg Day 10 of body weight per day Secondary failure to respond: Failure to gain at least 5 g/kg During rehabilitation of body weight per day for 3 successive days
- 64. Review patient records for common factors in adverse outcomes. Deaths that occur within the first 2 days are often due to: Hypoglycaemia. Overhydration. Unrecognized or mismanaged septic shock, or other serious infection. Deaths that occur after 2 days are often due to: Heart failure.
- 65. DISCHARGE. WHO recommends that children be kept in the severe malnutrition ward or area until they reach −1 SD weight- for-height. It usually requires about 2 – 6 weeks . If a child leaves before being achieving -1 SD, he is likely to get worse and have to return. WHO recommends that children be kept in the severe malnutrition ward or area until their condition is stabilized( regained appetite, reduced edema)
- 66. General instructions. In addition to feeding instructions, mothers will need to be taught: how to feed the child at home and give supplements. how to continue any needed medications, vitamins , folic acid (for 1 − 2 weeks), and iron (for 1 month) at home
- 67. General instructions. when and where to go for planned follow-up: at 1 week, 2 weeks, 1 month, 3 months, and 6 months; then twice yearly visits until the child is at least 3 years old.
