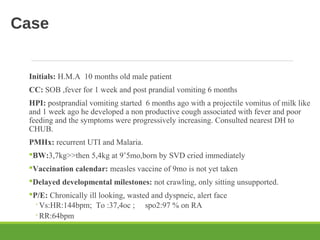
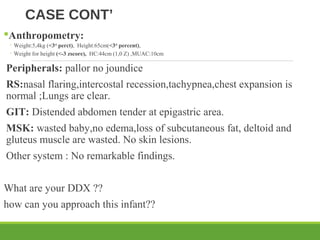
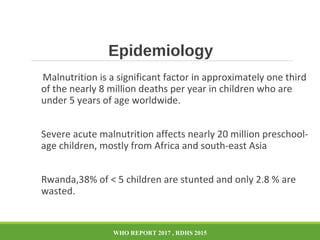
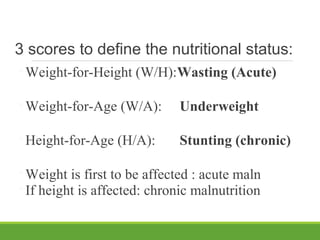
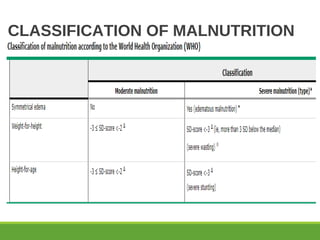
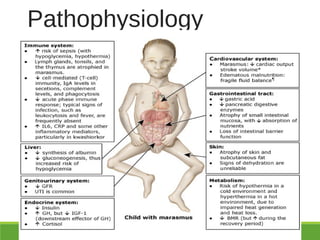
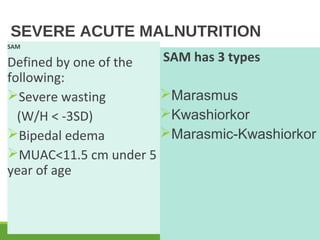
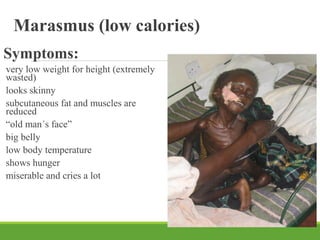
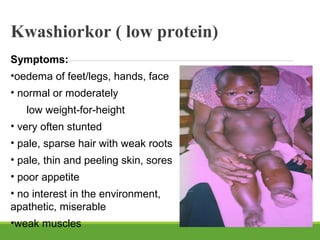
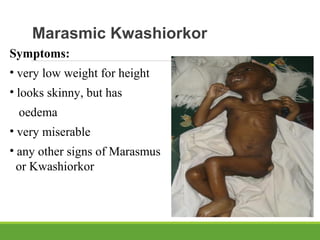
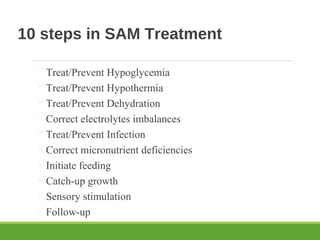
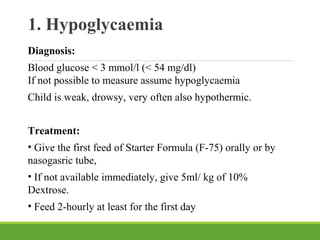
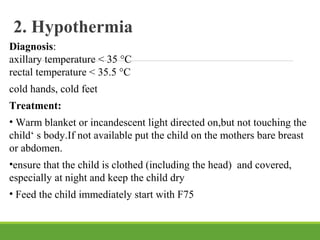
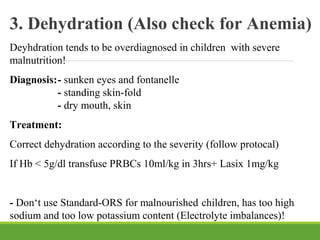
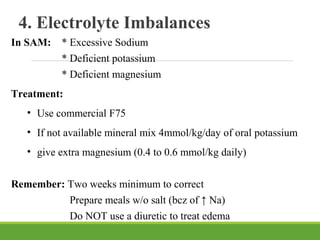
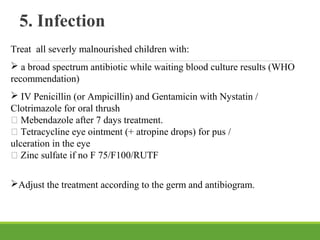
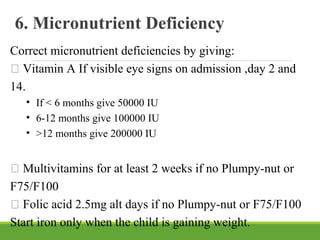
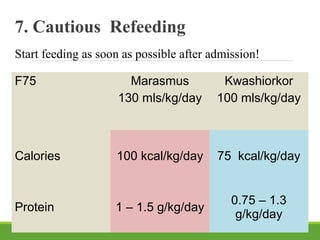
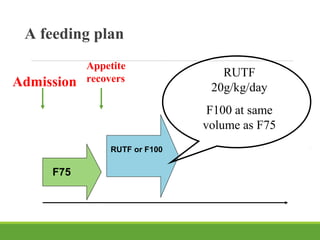
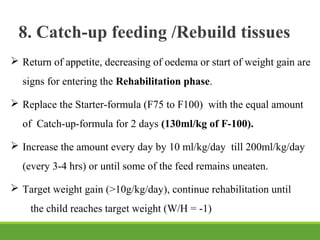
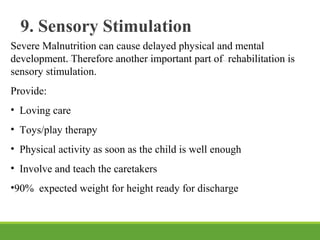
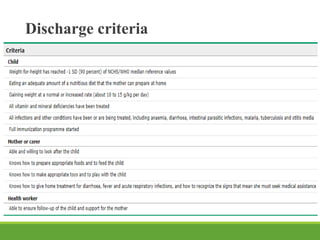
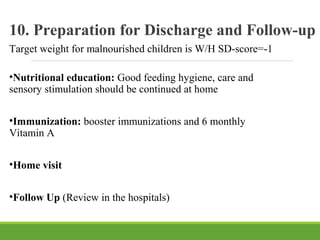
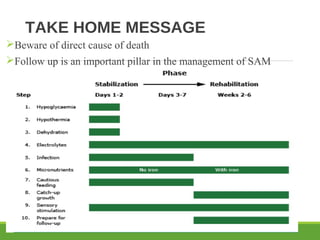
This document describes the case of a 10 month old male patient presenting with symptoms of shortness of breath, fever, and post-prandial vomiting for 6 months. On examination, the patient appeared chronically ill, wasted, and dyspneic. Anthropometric measurements revealed severe wasting. Differential diagnoses for this case of severe acute malnutrition include marasmus, kwashiorkor, and marasmic-kwashiorkor. The standard 10 step approach is recommended, involving treating hypoglycemia, hypothermia, dehydration, infections, and providing cautious refeeding with F75 or F100 formulas.