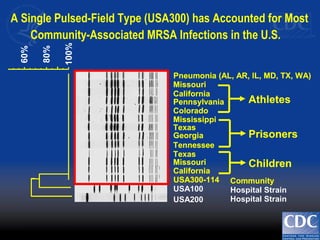
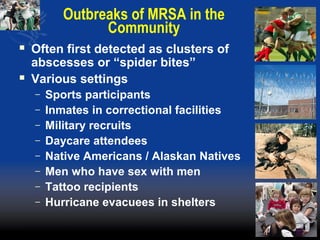
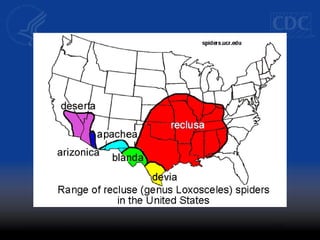
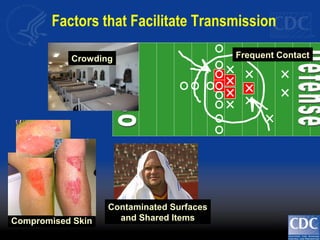
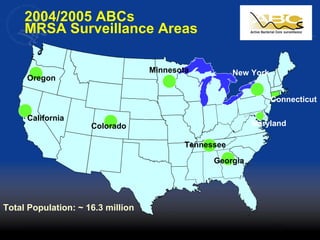
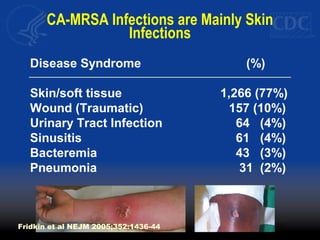
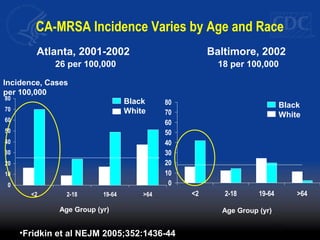
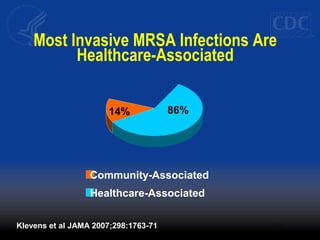
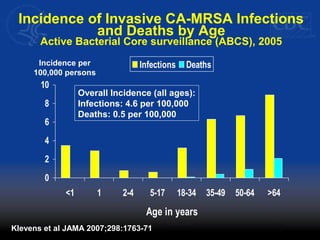
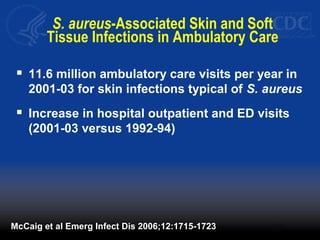
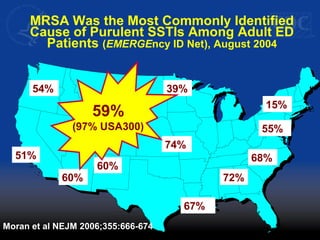
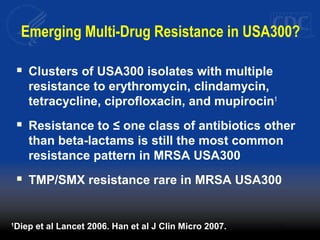
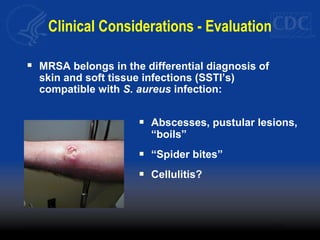
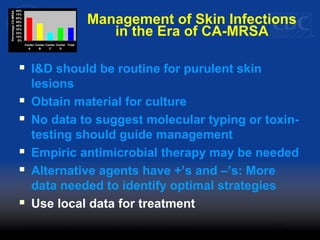
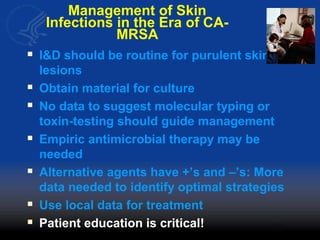
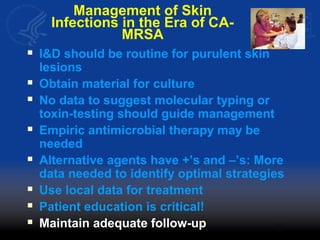
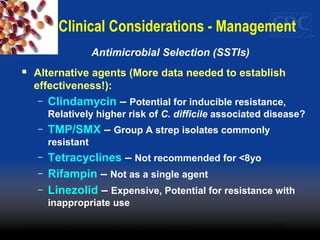
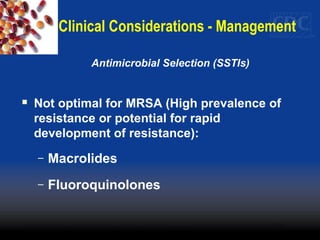
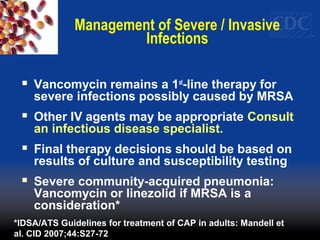
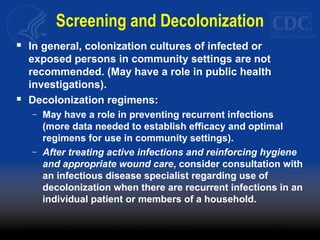
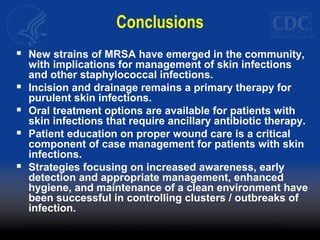
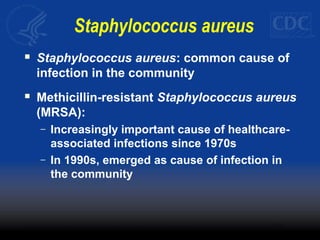
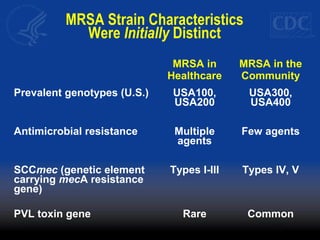
This document discusses methicillin-resistant Staphylococcus aureus (MRSA) infections in the community. It notes that MRSA emerged as a cause of infection in the community in the 1990s. Initially, MRSA strains in healthcare settings differed from community-associated MRSA strains, but the predominant community-associated strain (USA300) is now also found in some healthcare settings. Community-associated MRSA often presents as skin and soft tissue infections. Treatment recommendations include drainage of purulent lesions, obtaining cultures, and consideration of empiric antimicrobial therapy based on local resistance patterns.
![Dice (Opt:0.50%) (Tol 1.3%-1.3%) (H>0.0% S>0.0%) [0.0%-100.0%]
Pfsma
100
90
80
70
60
50
Pfsma
2001005114
2001005078
2000018626
2001035045
99045065
95009938
94042318
96023760
99034758
96028758
AA0097
2004711282
.
.
.
.
.
.
.
.
.
.
.
.
IVa
IVa
I I
I V
IVa
I V
IV
I I
I I
IVa
USA300
USA700
USA100
USA800
USA400
USA500
USA1000
USA900
USA600 .
USA200
USA1100
USA1200
8
72
5
5
1
8
59
15 / 13 1.
36
30
.
.
.
.
.
.
.
POS
NEG
NEG
NEG
NEG
NE
NE
NE
NE
NE
NE
PO
NE
PFT SCCmecMLST pvl
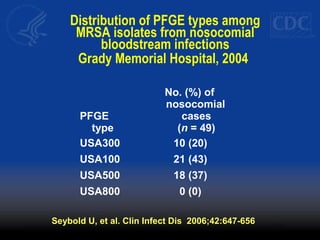
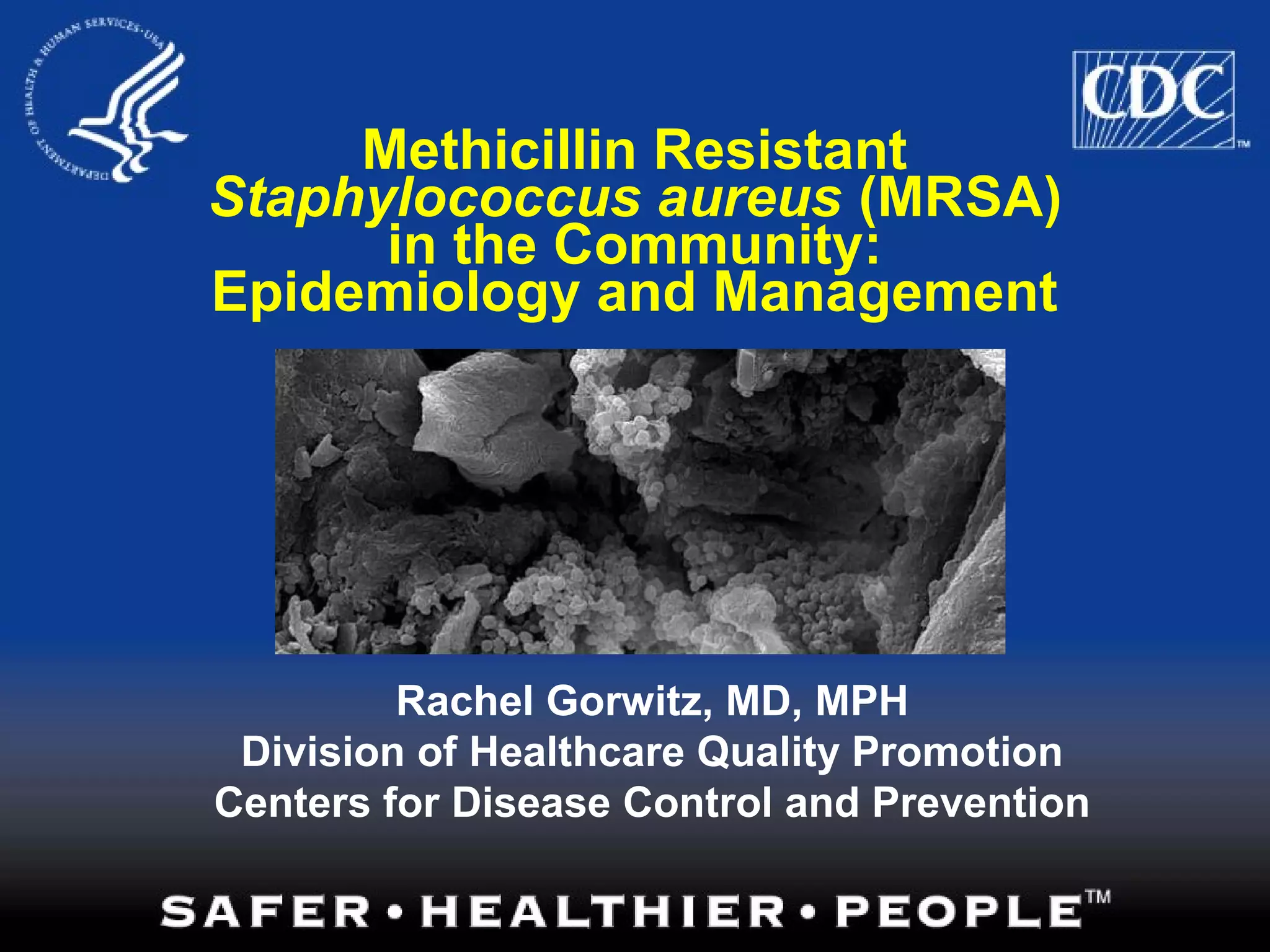
USA300 8 IV POS
USA700 72 IV NEG
USA100 5 I I NEG
USA800 5 IV NEG
USA400 1 IV POS
USA500 8 IV, I I NEG
USA1000 59 IV NEG/POS
USA900 15 MSSA NEG
USA600 45 I I NEG
USA200 36 I I NEG
USA1100 30 IV POS
USA1200 MSSA POS
McDougal et al J Clin Micro 2003;41:5113-5120
National Database of MRSA Pulsed-Field Types
(Highlighted PFTs: historically community-associated)](https://image.slidesharecdn.com/gorwitzcocawebcast2007-130904125548-/85/MRSA-4-320.jpg)