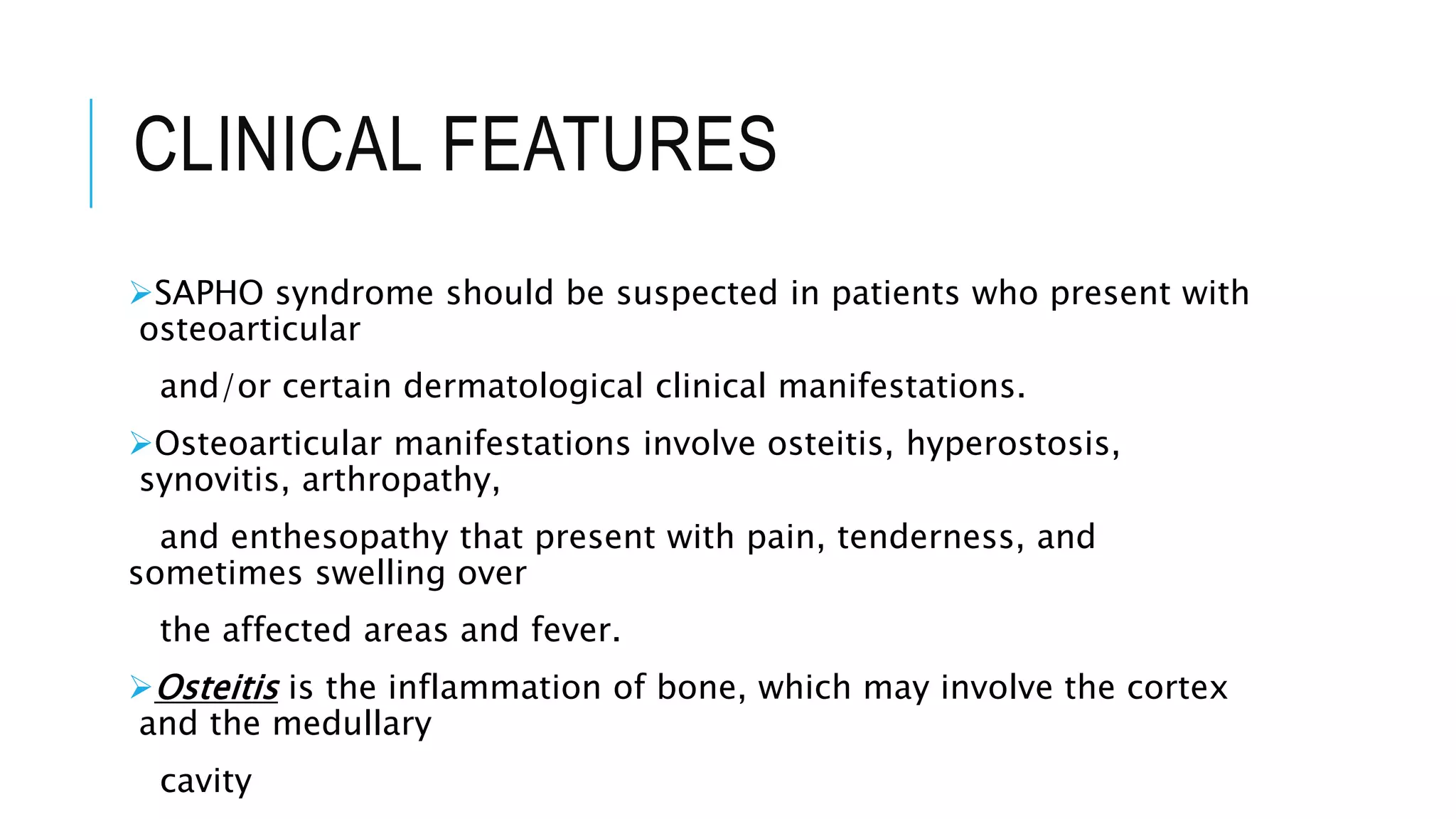
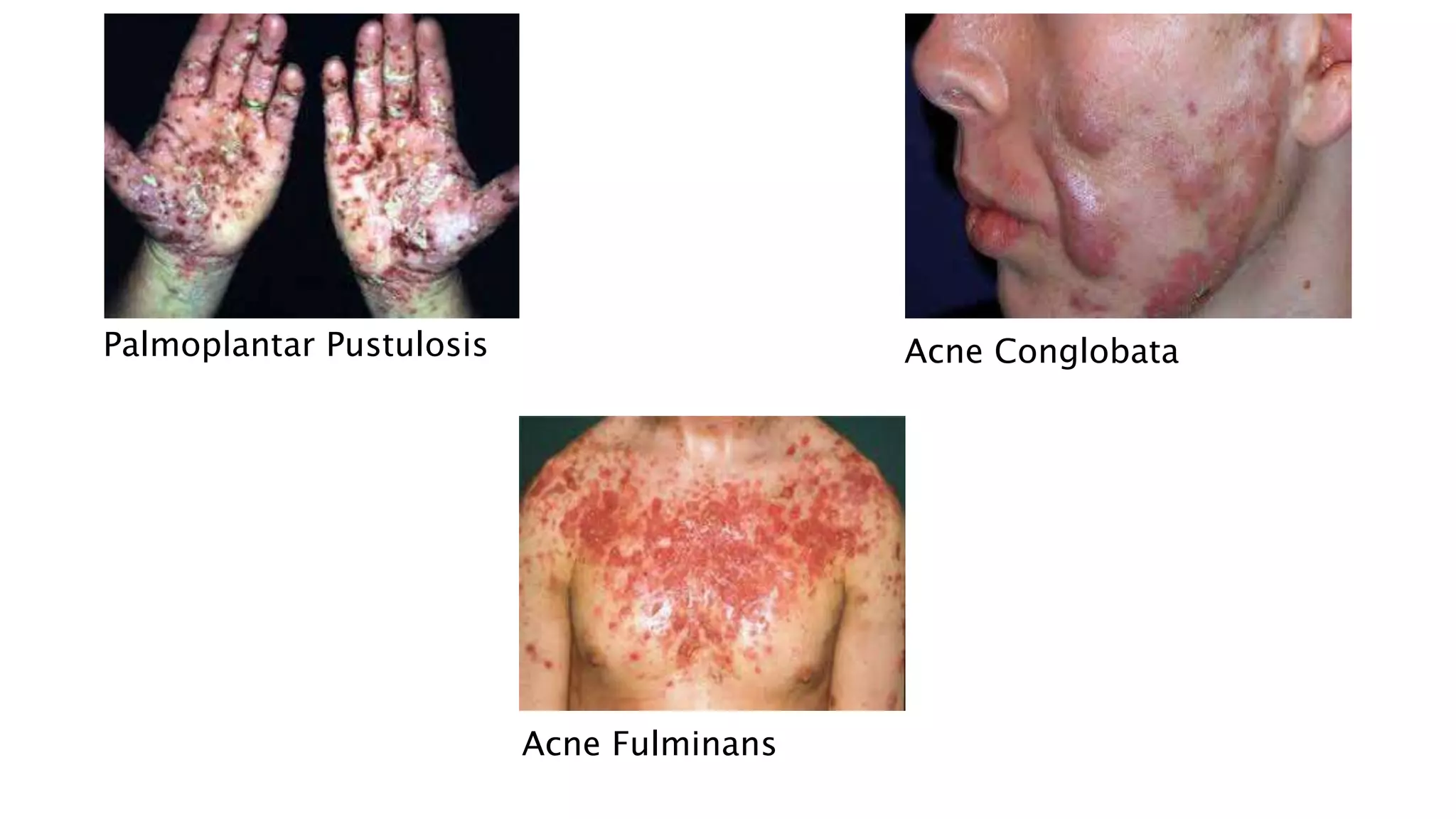
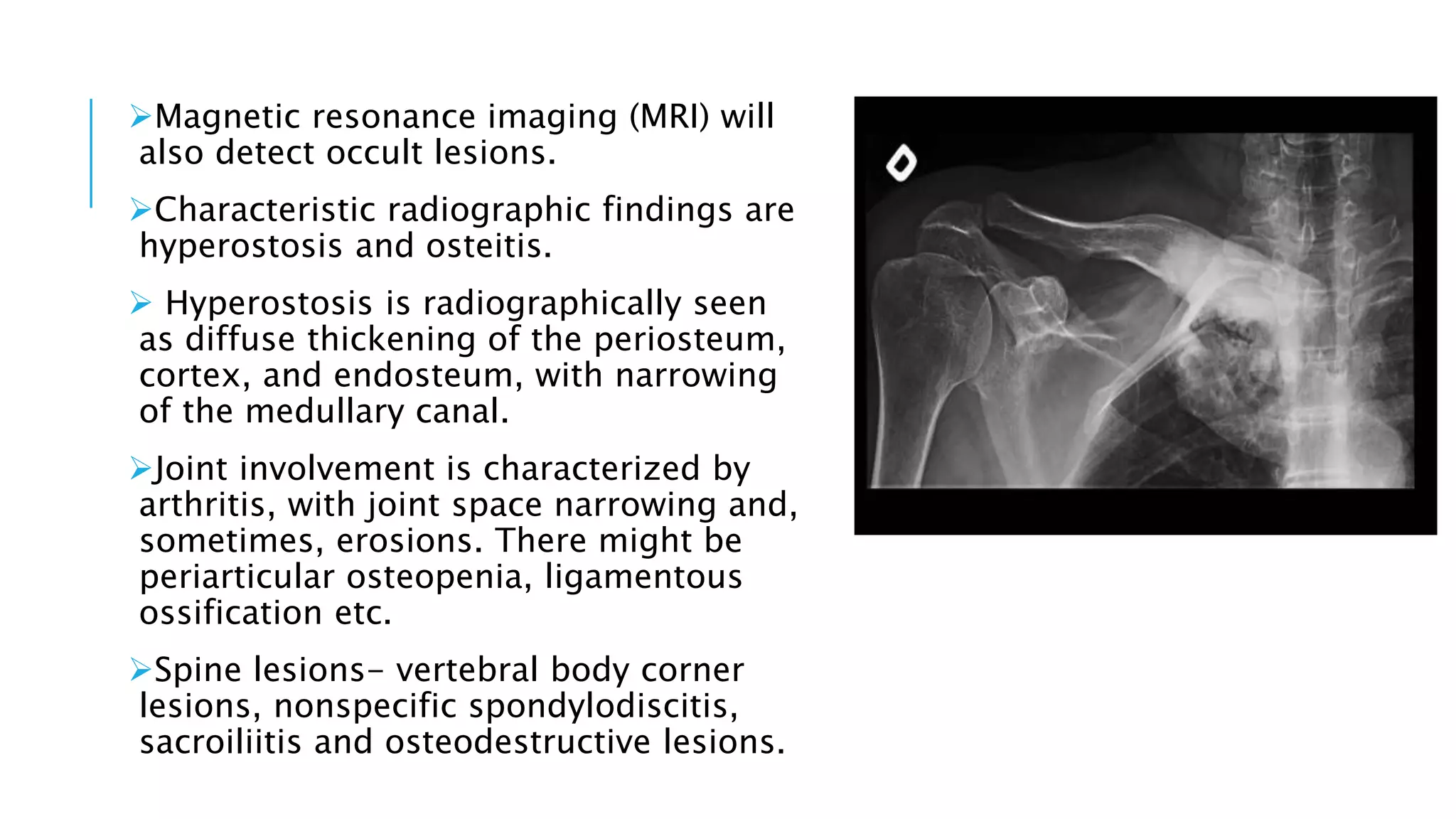
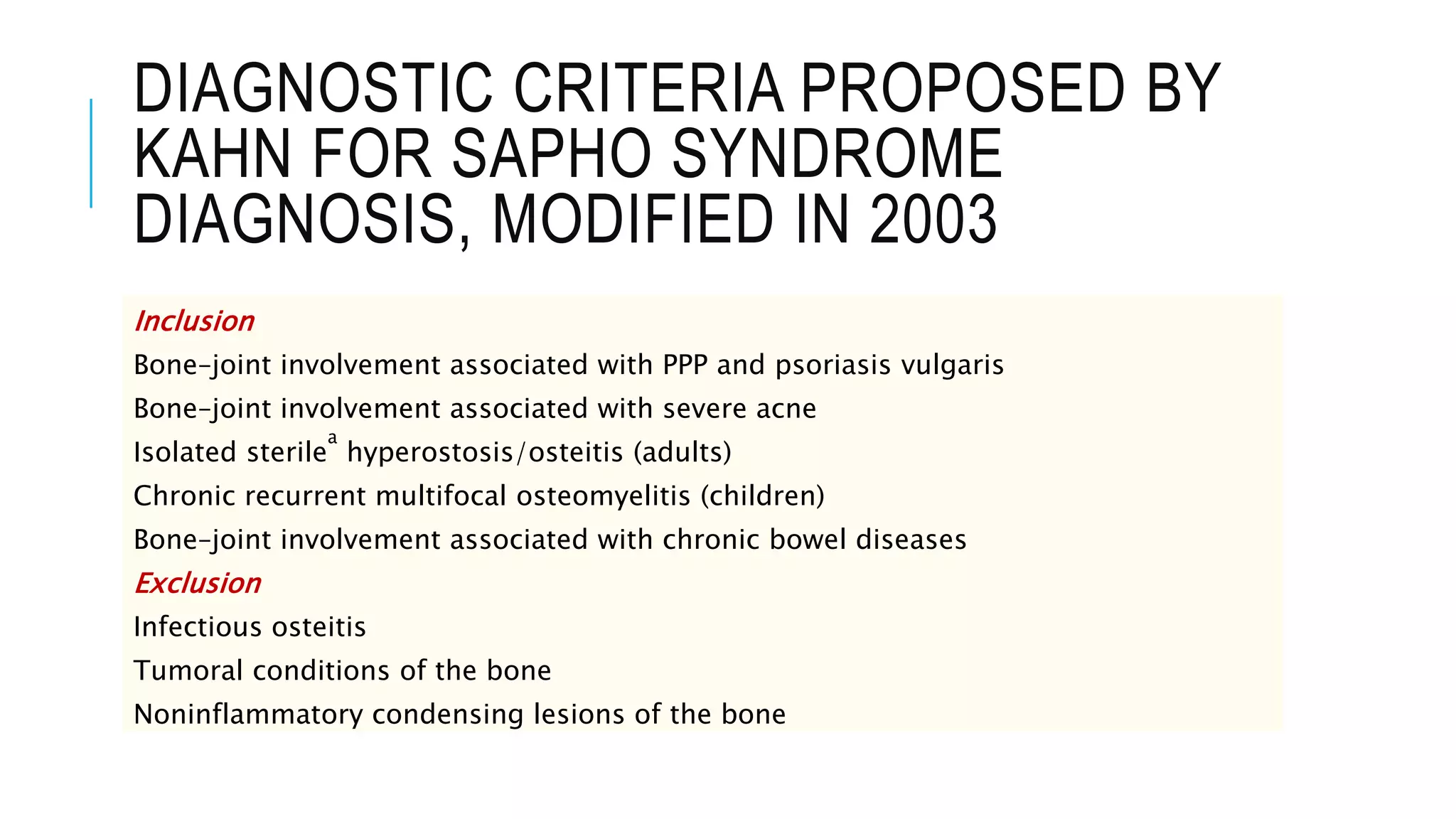
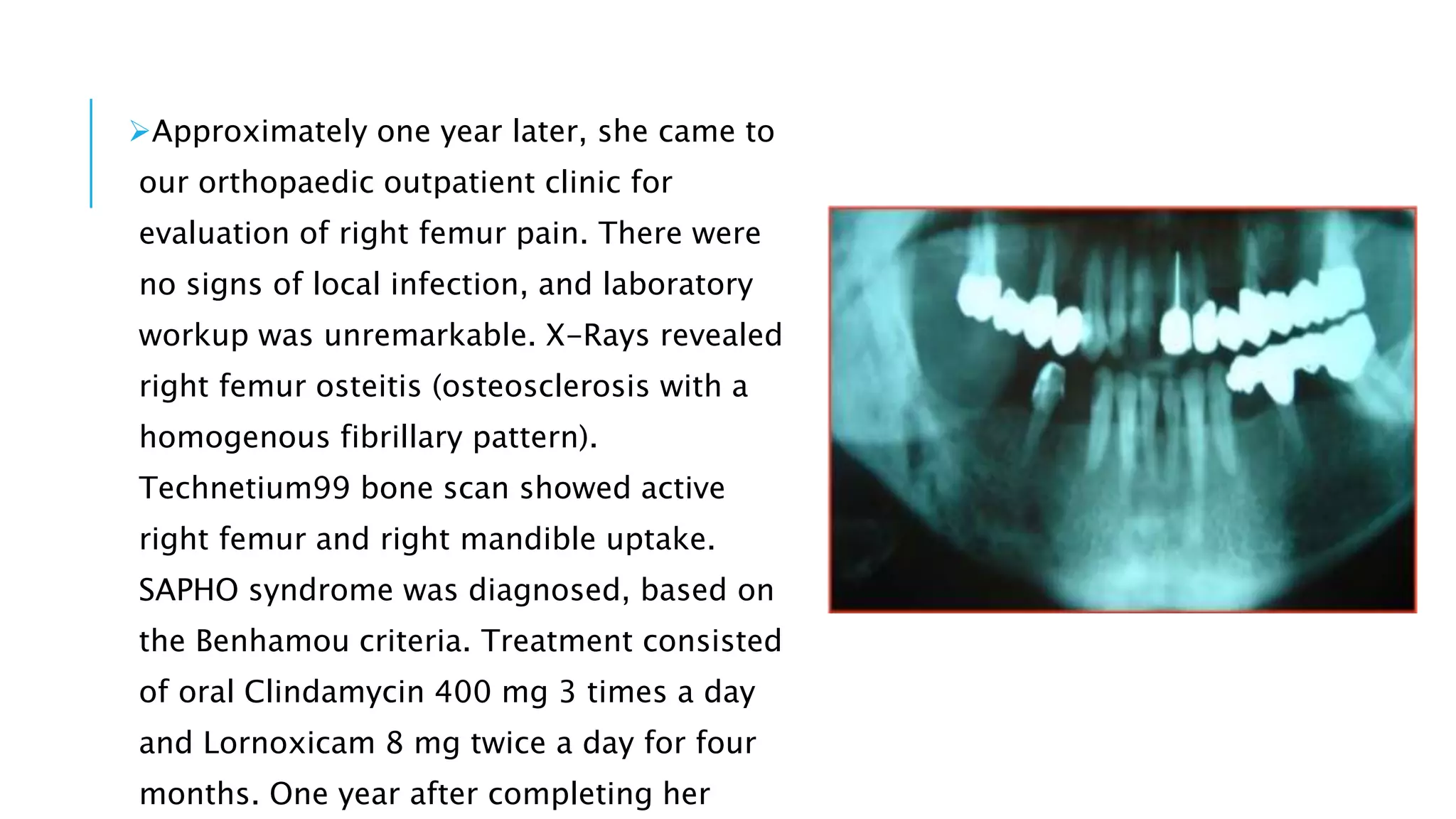
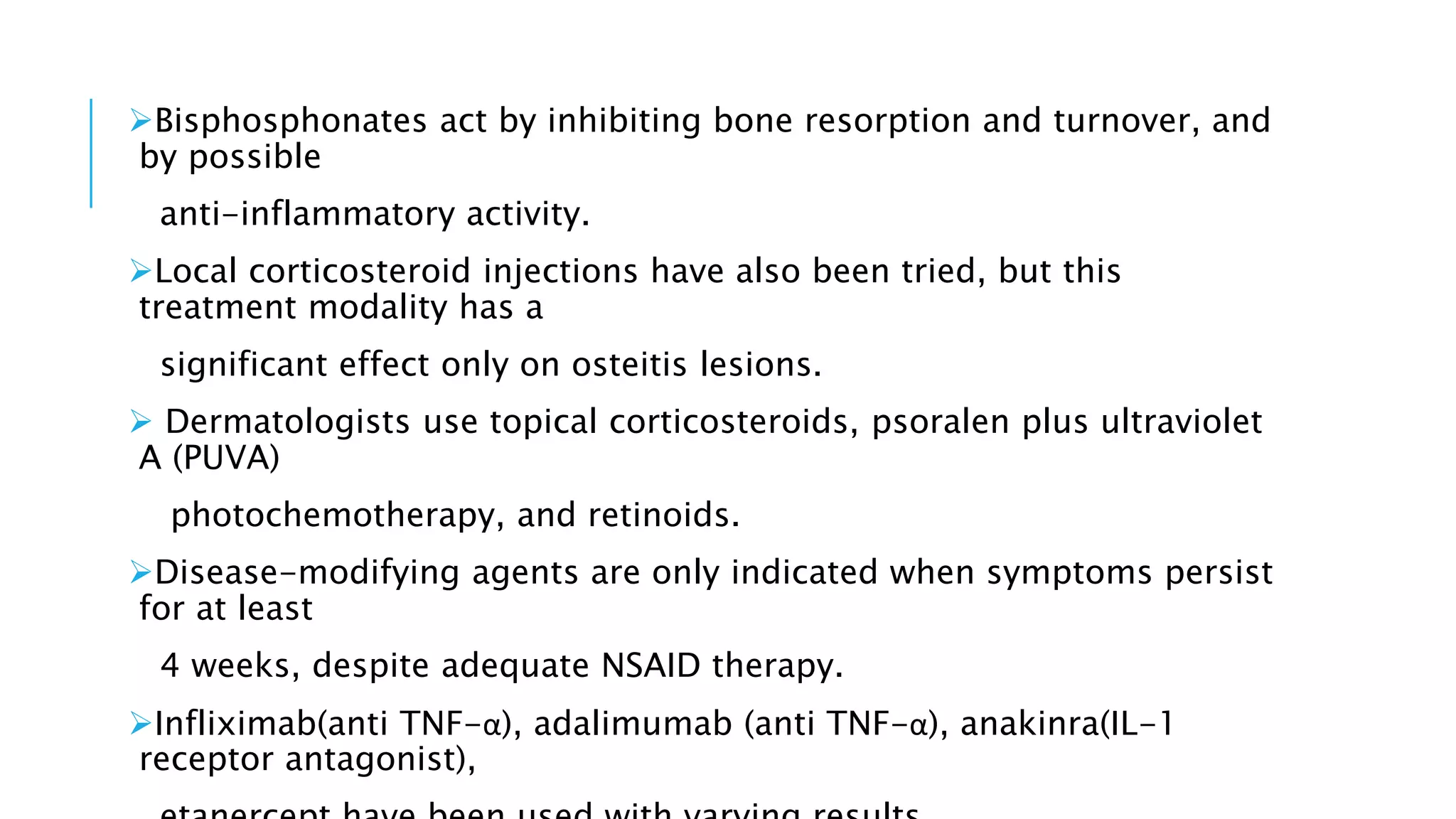
The document discusses SAPHO syndrome, characterized by synovitis, acne, pustulosis, hyperostosis, and osteitis, with a complex etiology likely involving genetic, infectious, and immunological factors. Key clinical features include osteoarticular manifestations, such as osteitis and arthritis, alongside skin conditions like palmoplantar pustulosis and severe acne, while diagnostic criteria and differential diagnoses are outlined. Treatment options vary, including NSAIDs, antibiotics, and immunomodulatory medications, with a generally relapsing-remitting or chronic indolent disease course.