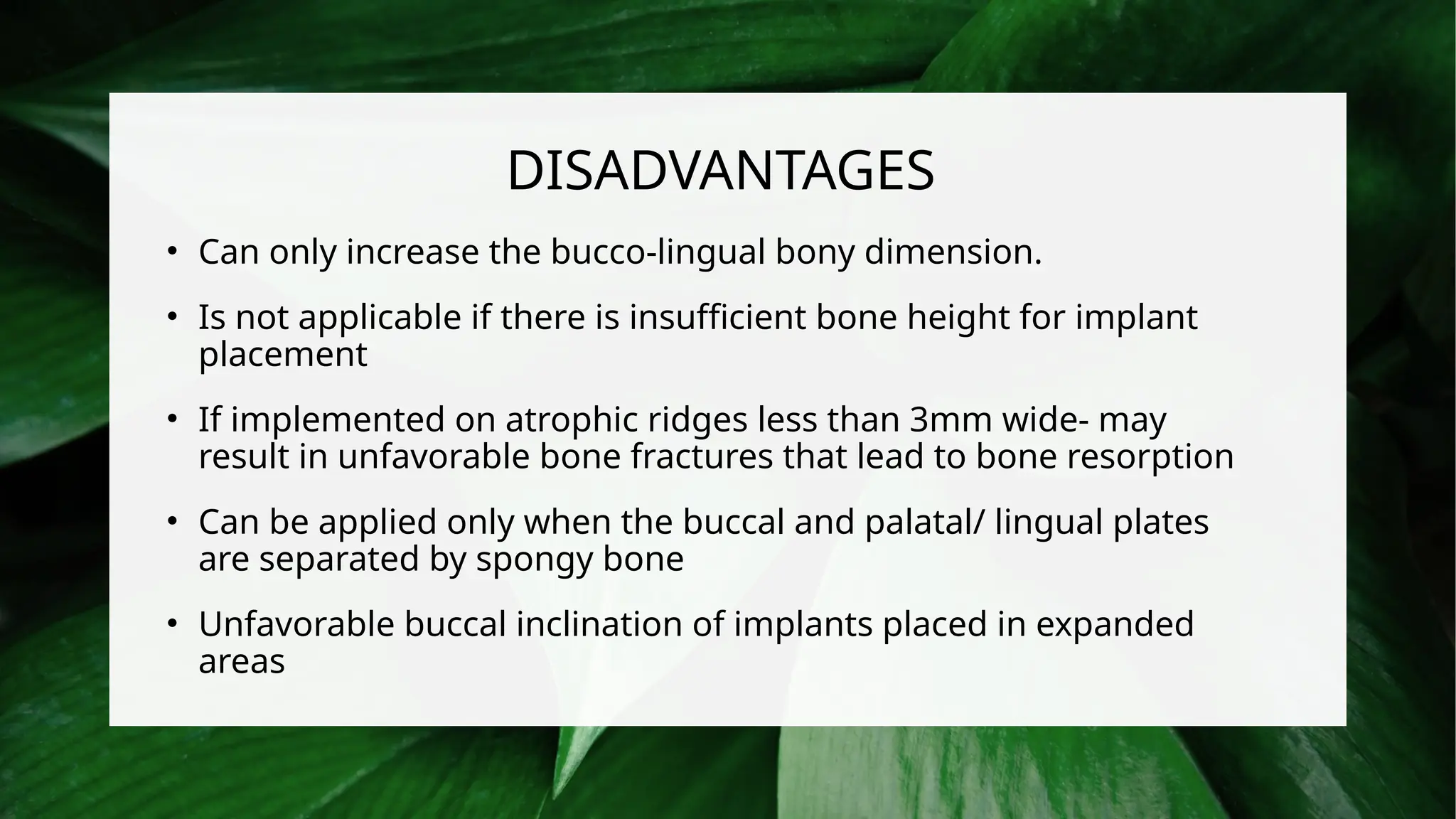
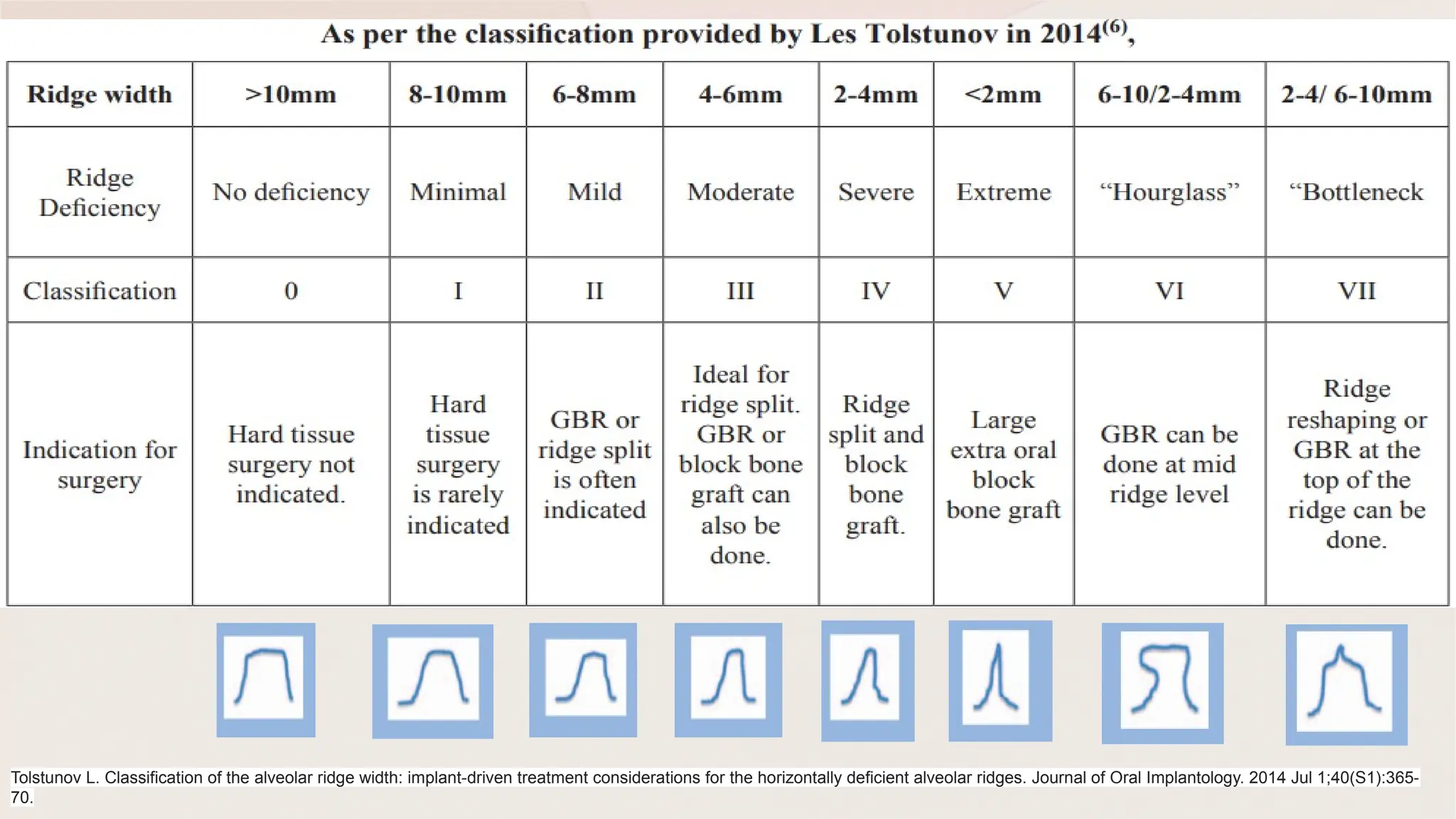
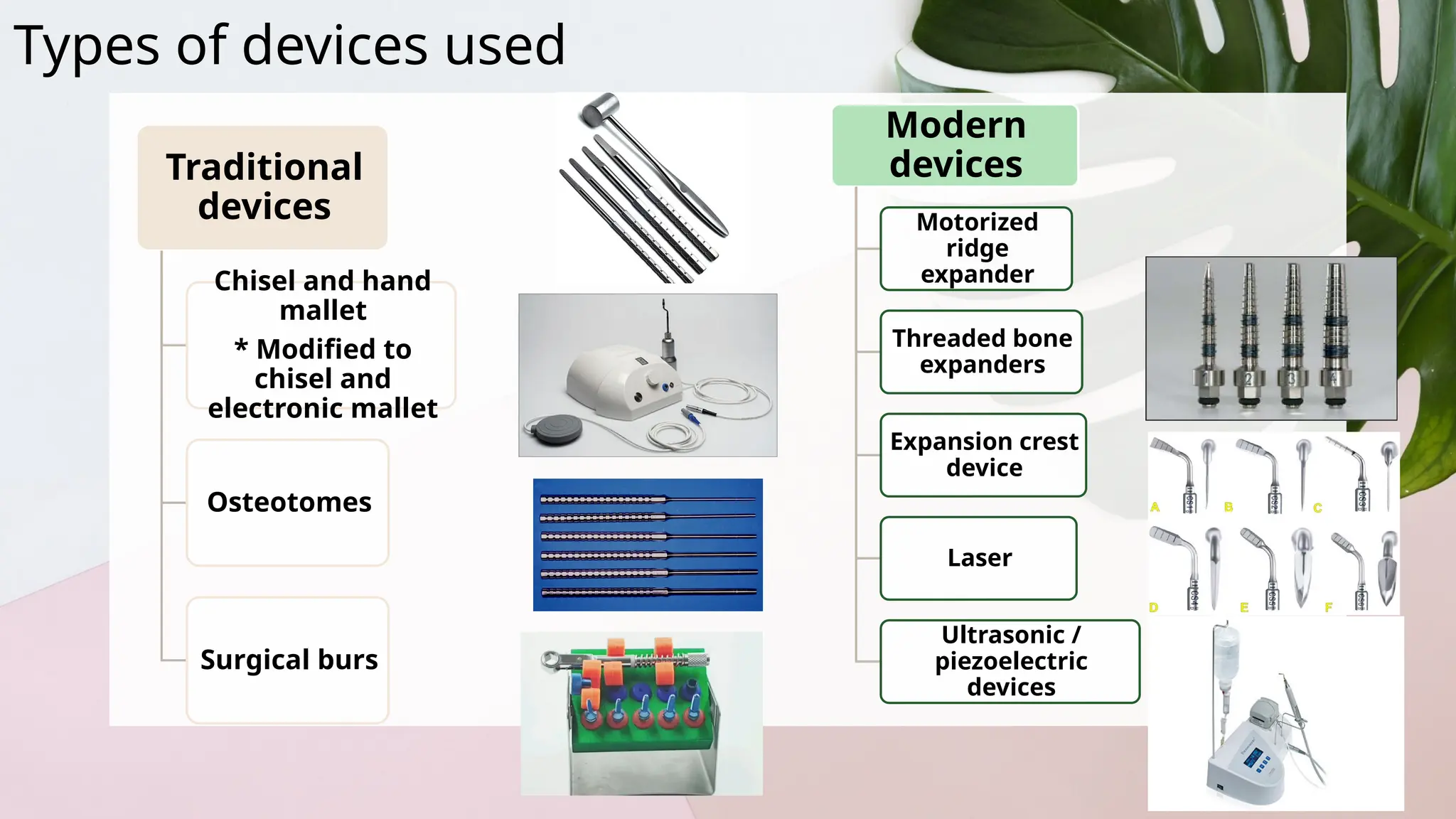
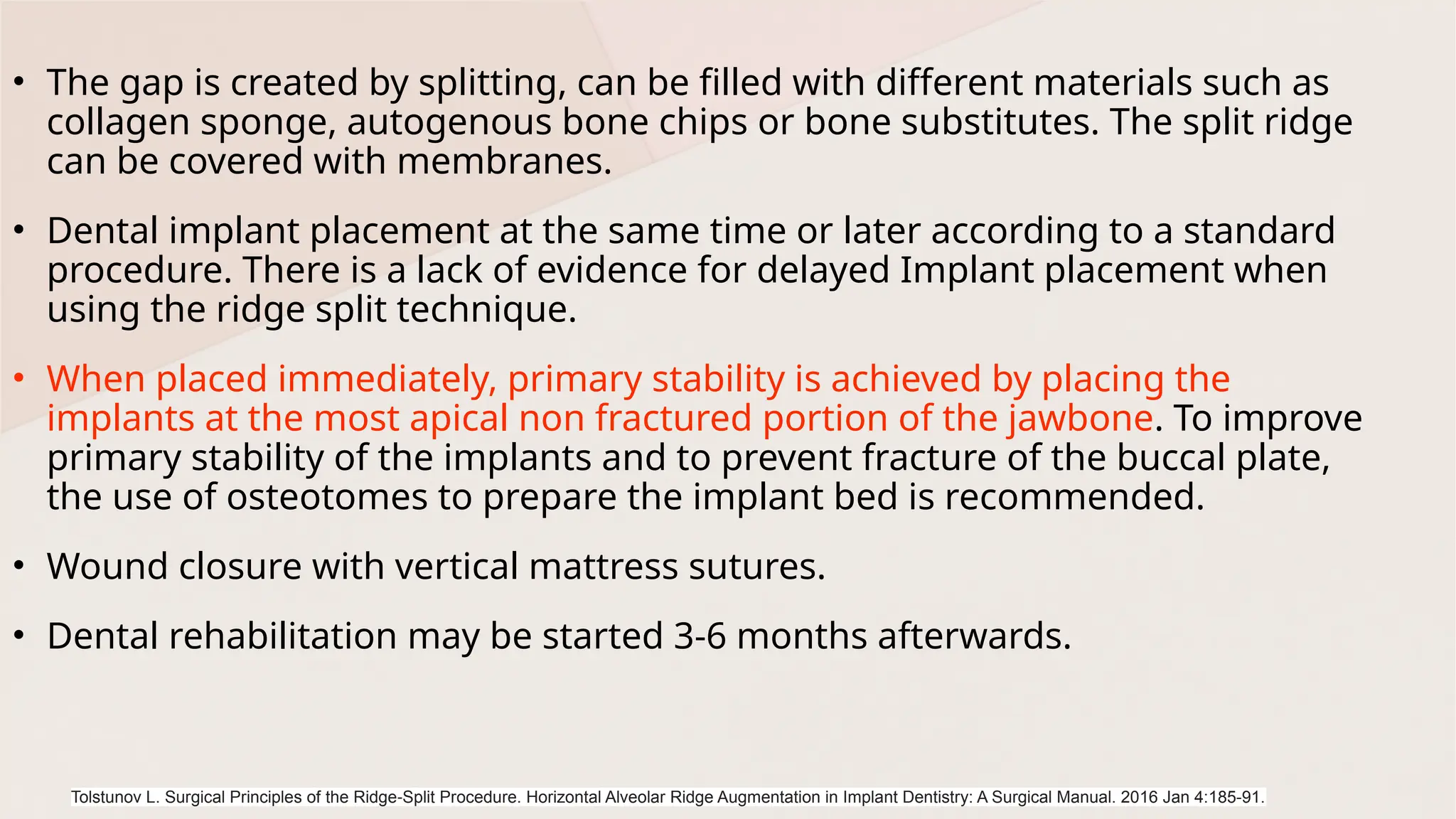
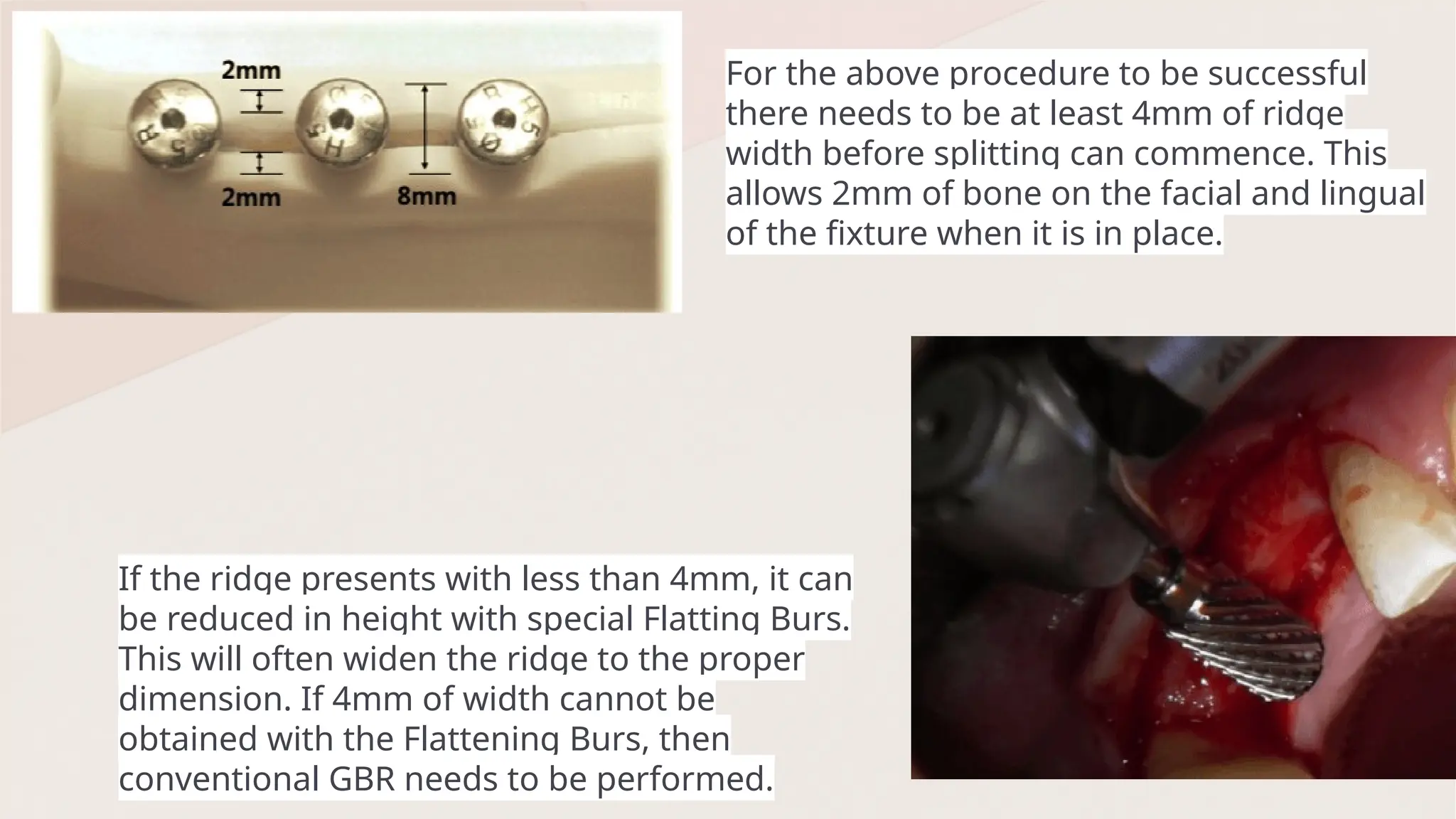
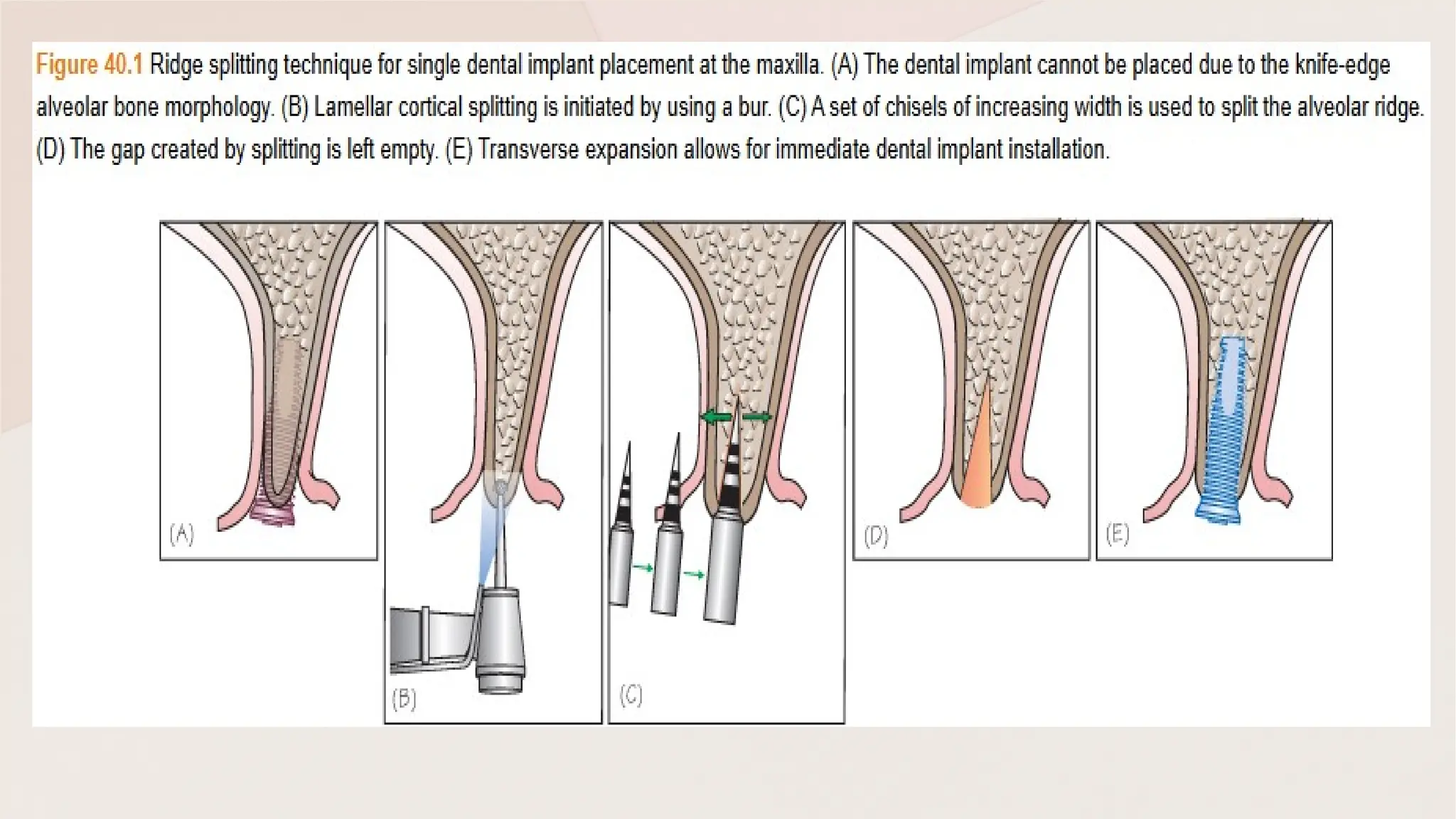
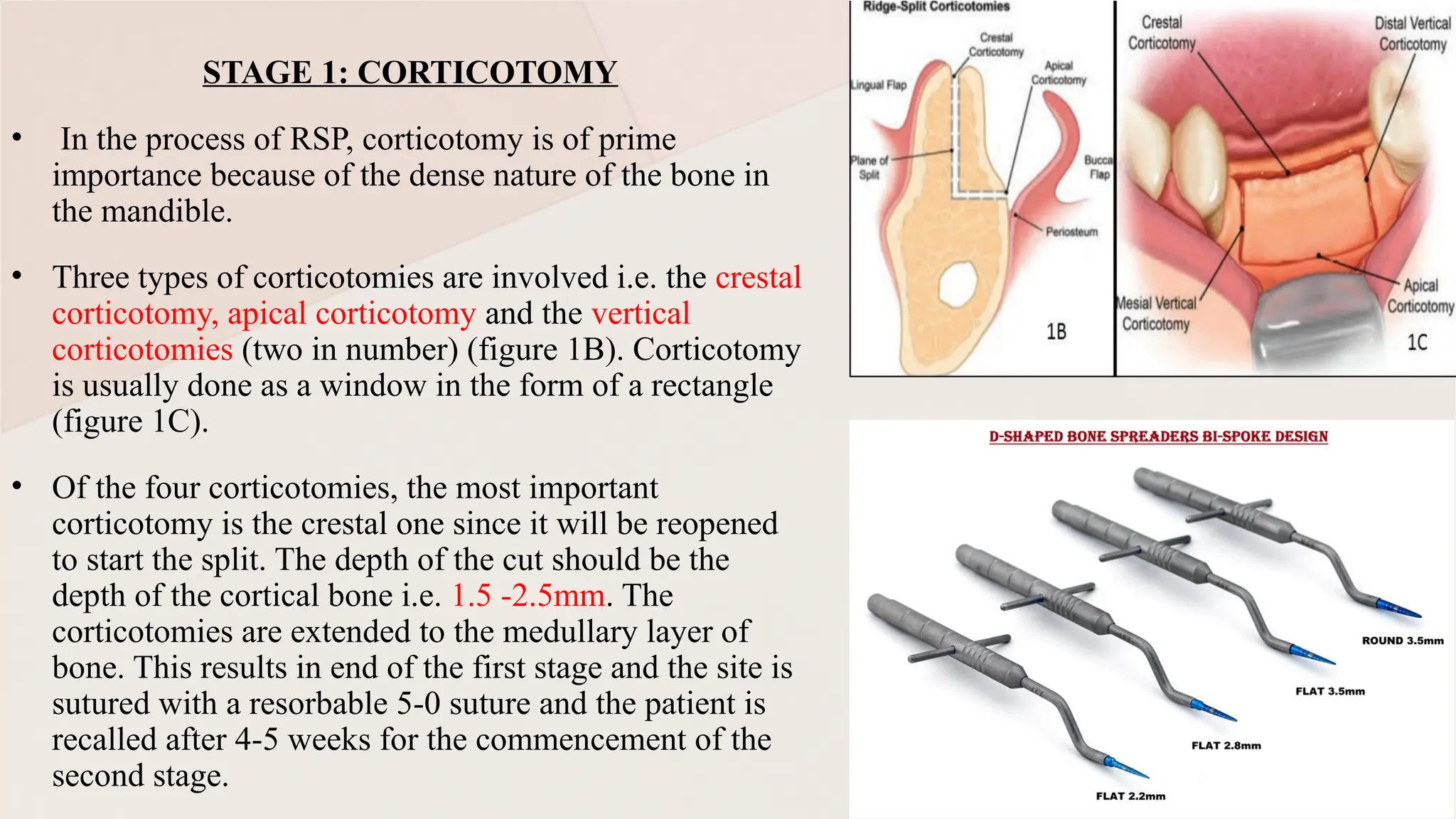
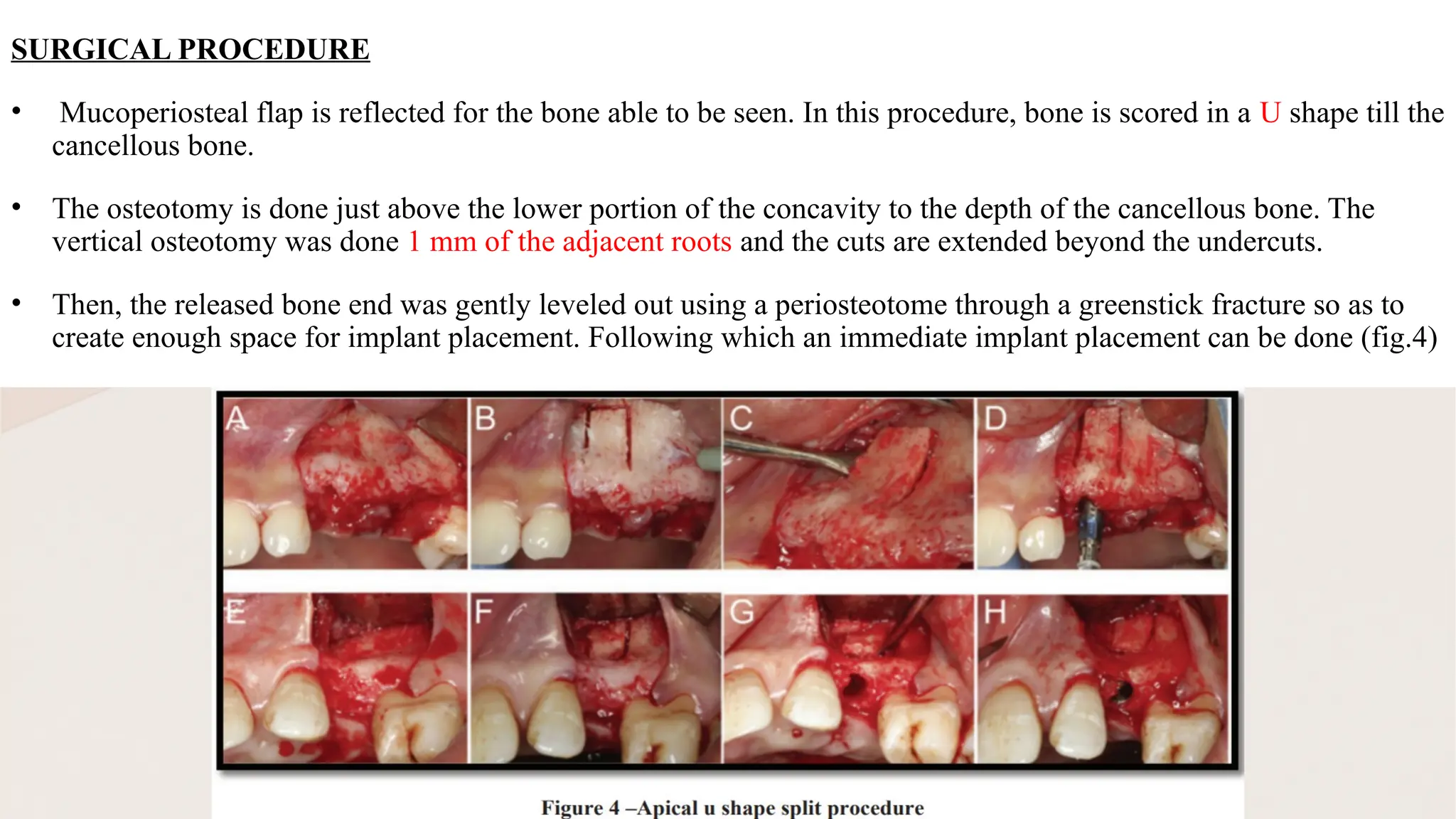
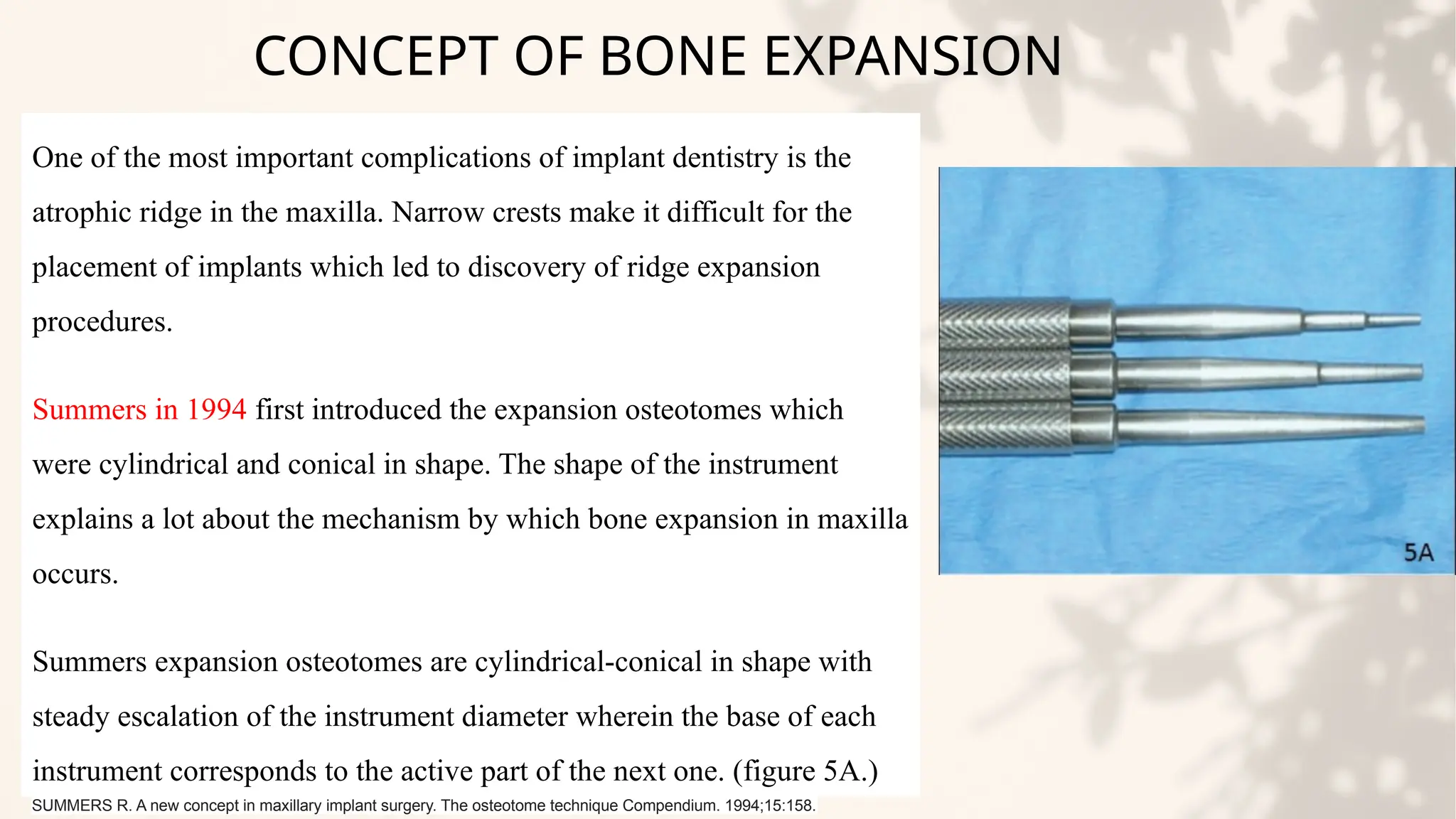
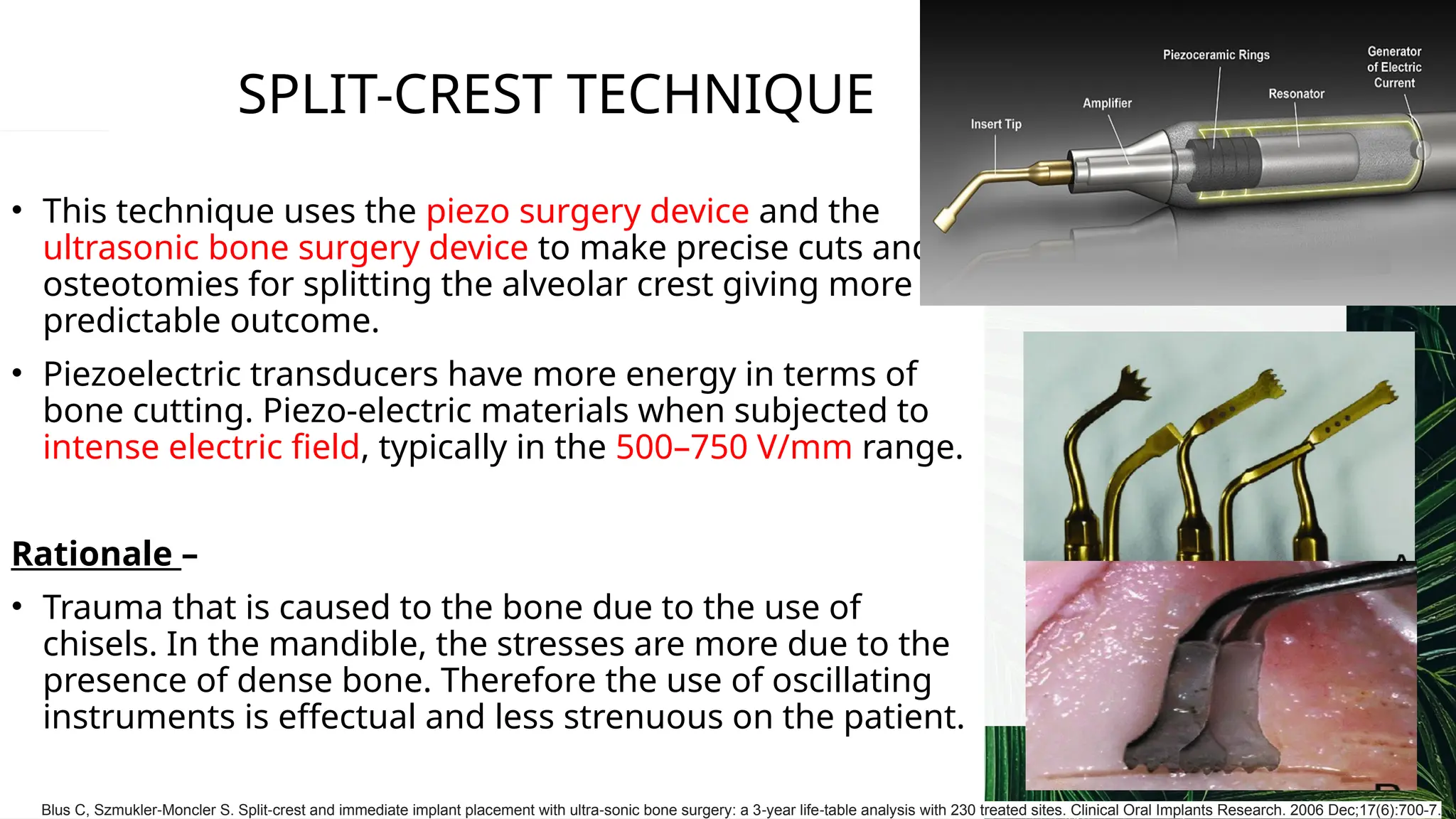
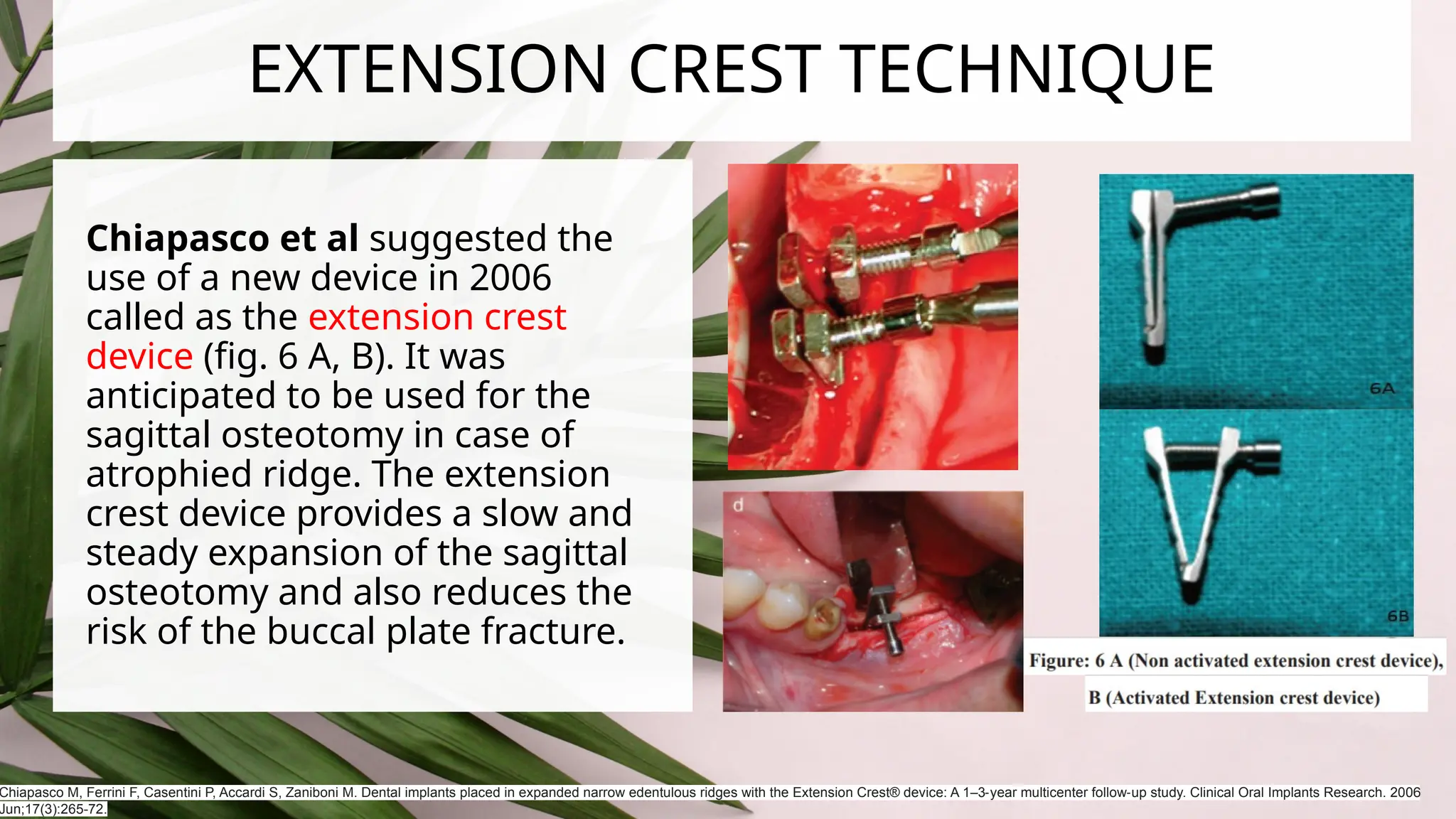
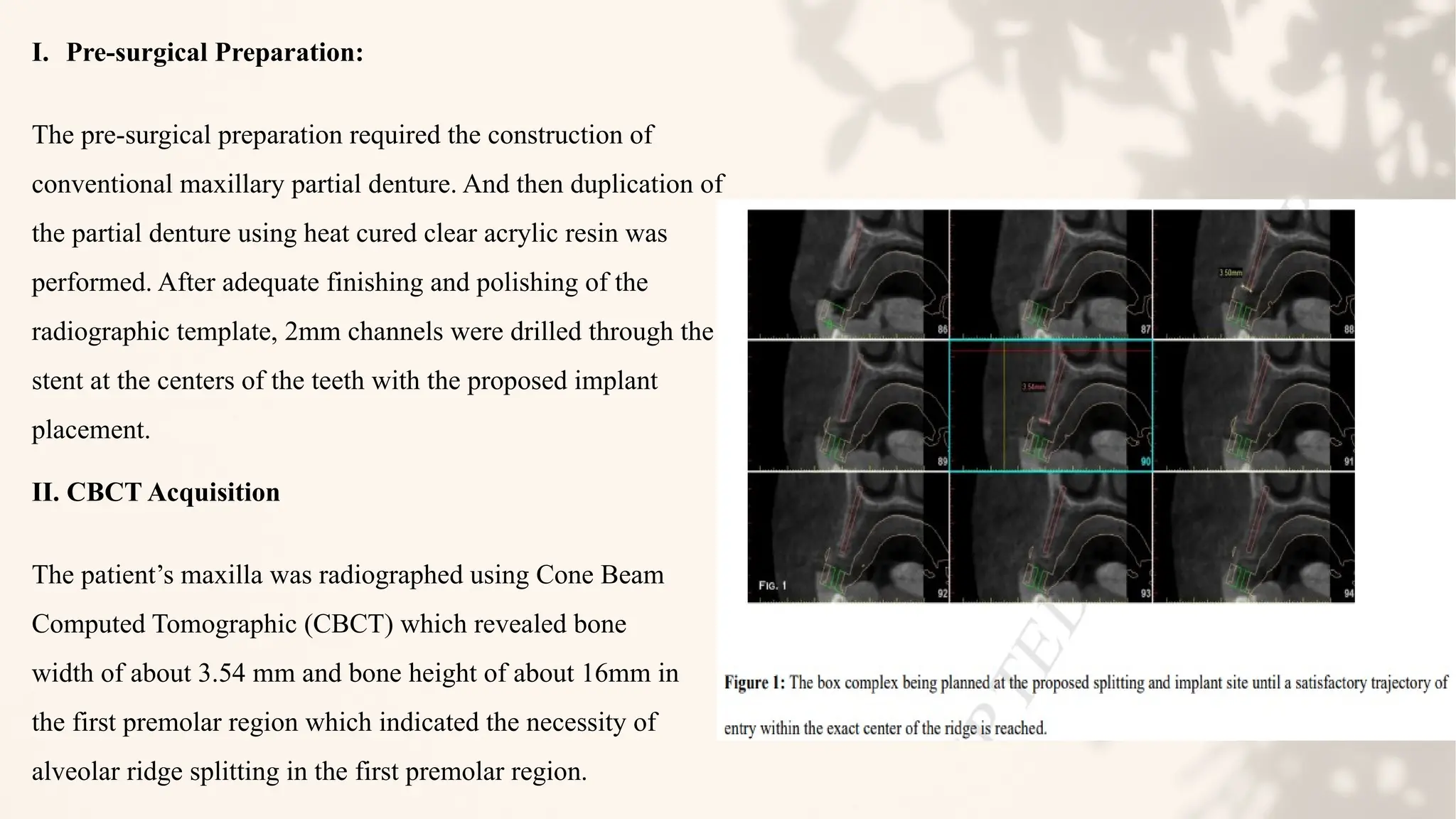
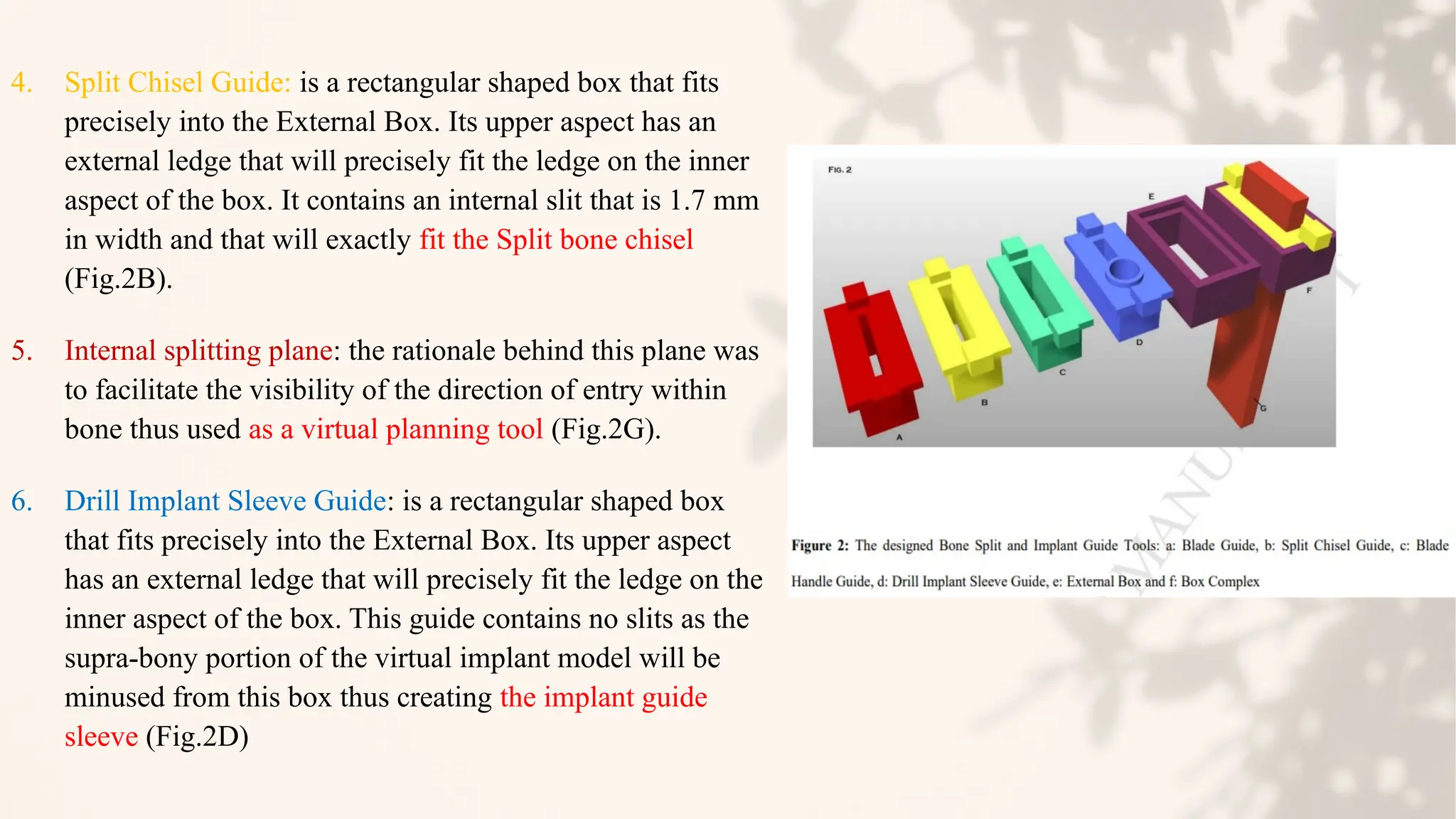
The document discusses ridge split techniques in prosthodontics, particularly their applications for augmenting narrow alveolar ridges for dental implant placement. It covers the history, indications, contraindications, advantages, and disadvantages of these techniques, along with their classifications and surgical principles. Recent advancements and specific procedures, including piezosurgery and the apical U-shape splitting technique, are also highlighted.