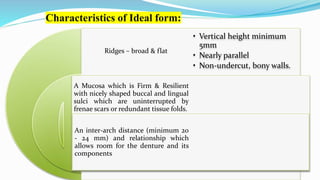
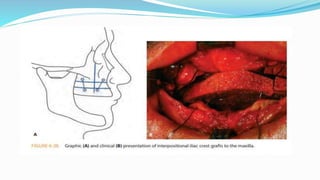
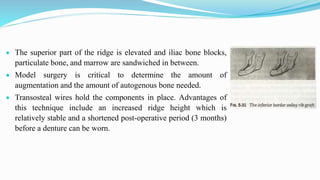
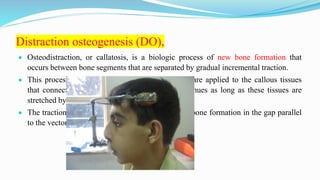
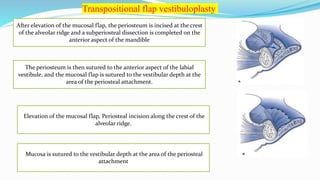
This document discusses secondary pre-prosthetic surgical procedures. It describes ideal ridge form for denture wearing and secondary procedures to modify ridges through augmentation or altering relationships. Ridge augmentation aims to recreate ridges compatible with dentures through autografts, homografts, or alloplastic materials. Ridge relationship procedures correct arch discrepancies through maxillary advancement or mandibular advancement surgeries. Secondary soft tissue procedures further modify ridges after hard tissue alterations.