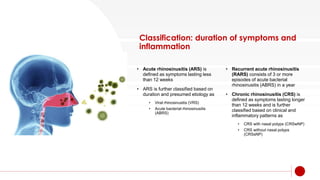
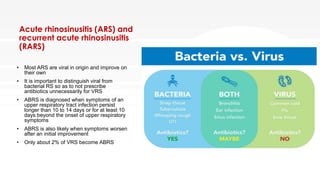
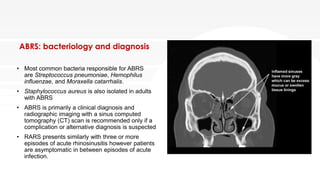
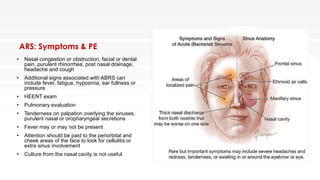
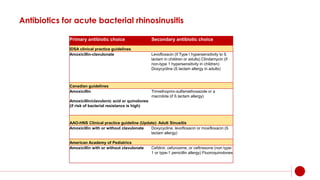
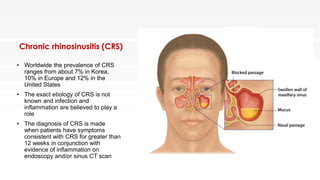
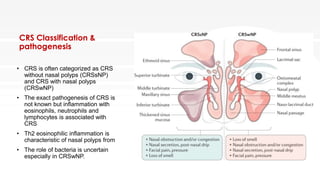
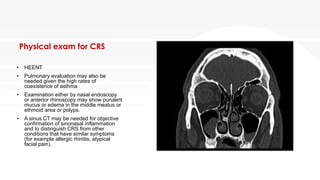
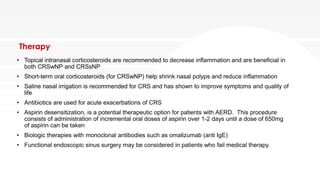
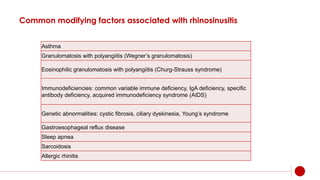
Rhinosinusitis (RS) is inflammation of the sinuses and nasal cavity, significantly impacting quality of life and healthcare costs, affecting over 12% of the U.S. population. It can be classified as acute, recurrent acute, or chronic, with varying symptoms and treatment options, including antibiotics for bacterial cases and intranasal steroids for chronic cases. The prevalence and treatment of chronic rhinosinusitis (CRS) highlight its complexity, with various potential modifying factors and a lack of definitive etiology.