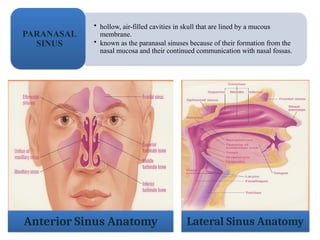
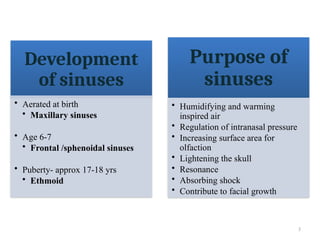
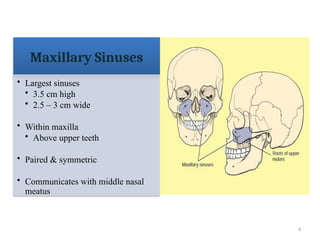
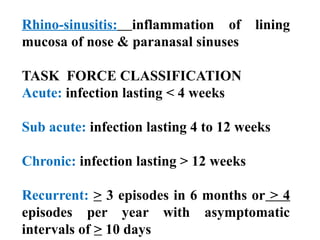
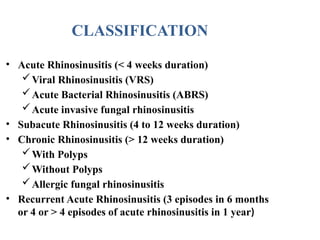
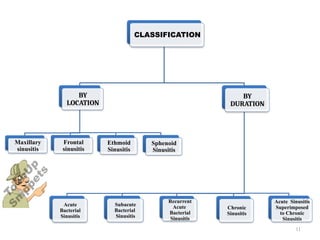
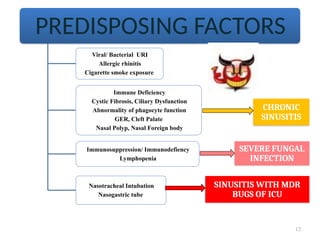
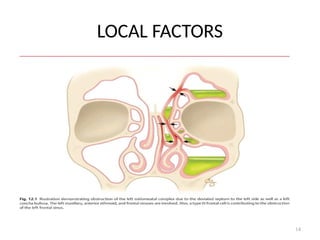
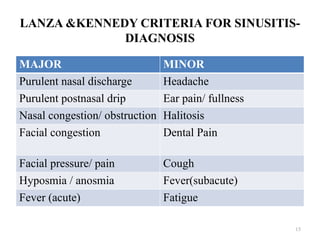
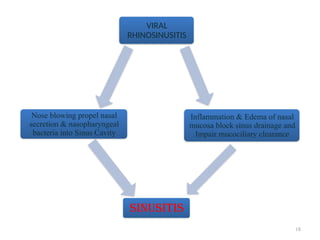
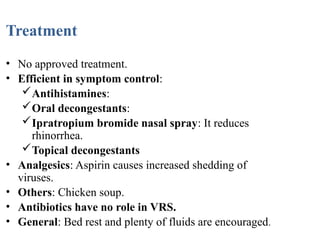
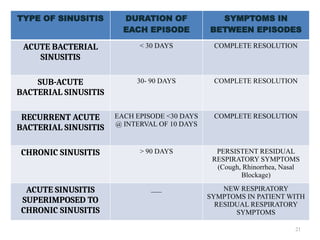
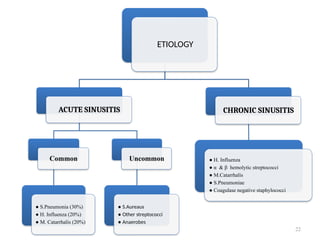
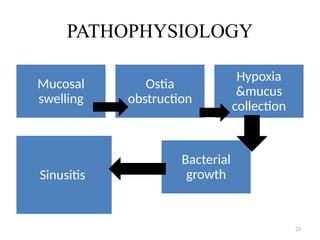
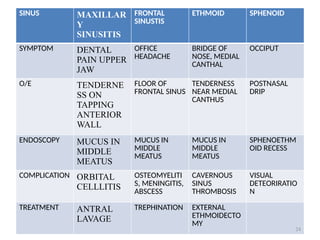
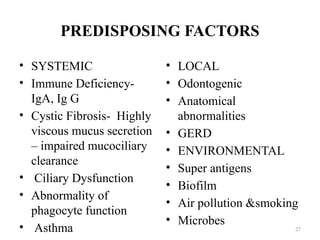
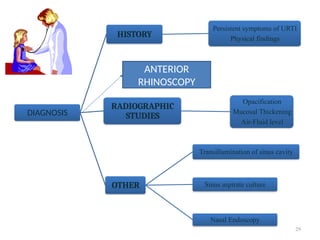
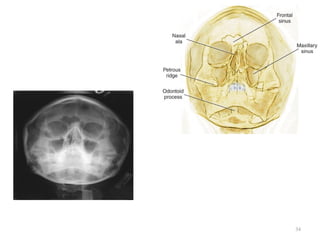
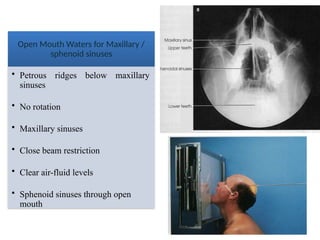
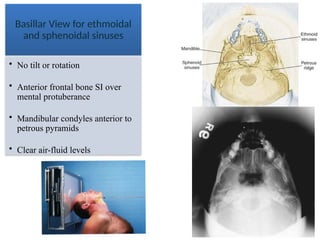
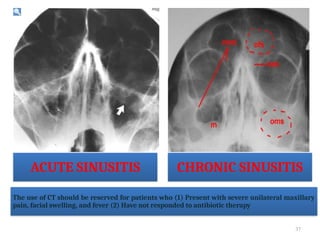
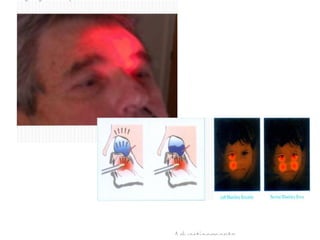
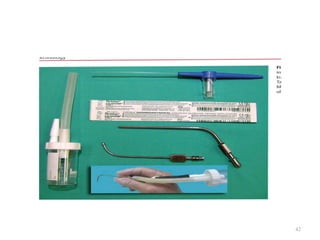
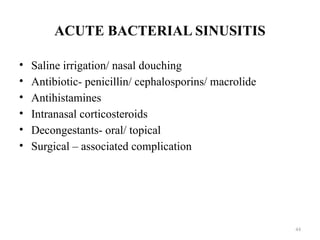
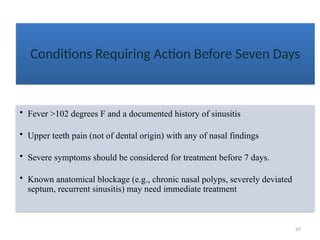
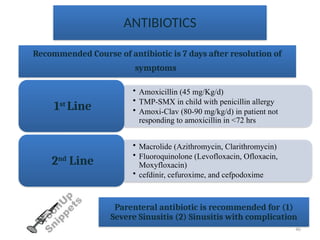
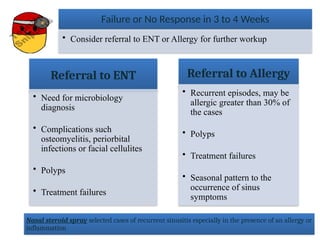
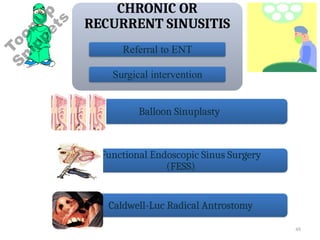
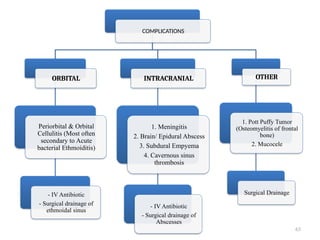
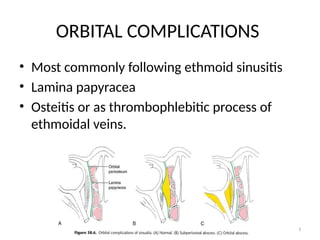
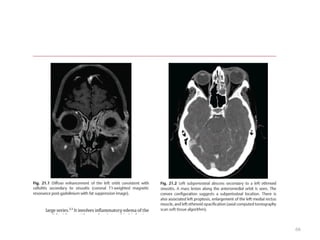
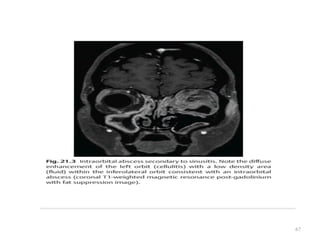
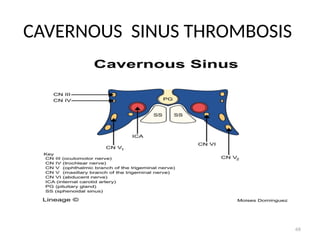
The document provides a comprehensive overview of sinusitis, including definitions, anatomy, types, classifications, causes, symptoms, diagnosis, and treatment options. It details the development of paranasal sinuses, various types of sinusitis (acute, chronic, recurrent), and underlying factors contributing to their conditions. Treatment recommendations include antibiotics for bacterial infections, nasal irrigation, and potential surgical interventions, while emphasizing the importance of proper diagnosis and management strategies.