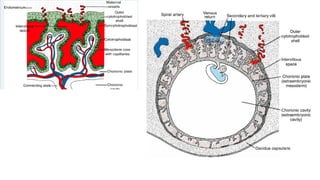
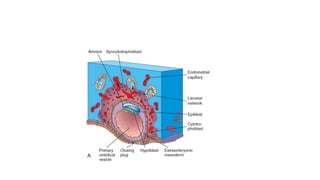
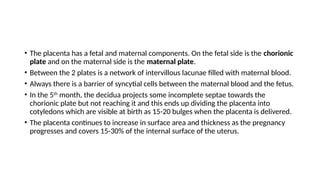
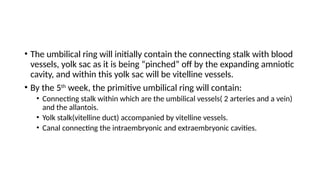
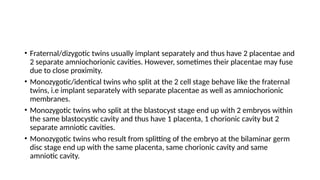
The document discusses the development and functions of the placenta and membranes during early pregnancy, highlighting the formation of the extraembryonic circulation, the roles of chorionic structures, and the processes involved in uterine attachment and growth. It details how the placenta evolves in size and function, including roles in nutrient exchange and hormone production, while also addressing twin pregnancies and potential complications like preeclampsia and placenta previa. The amniotic fluid's functions, along with the structure and changes of the umbilical cord, are also explained.