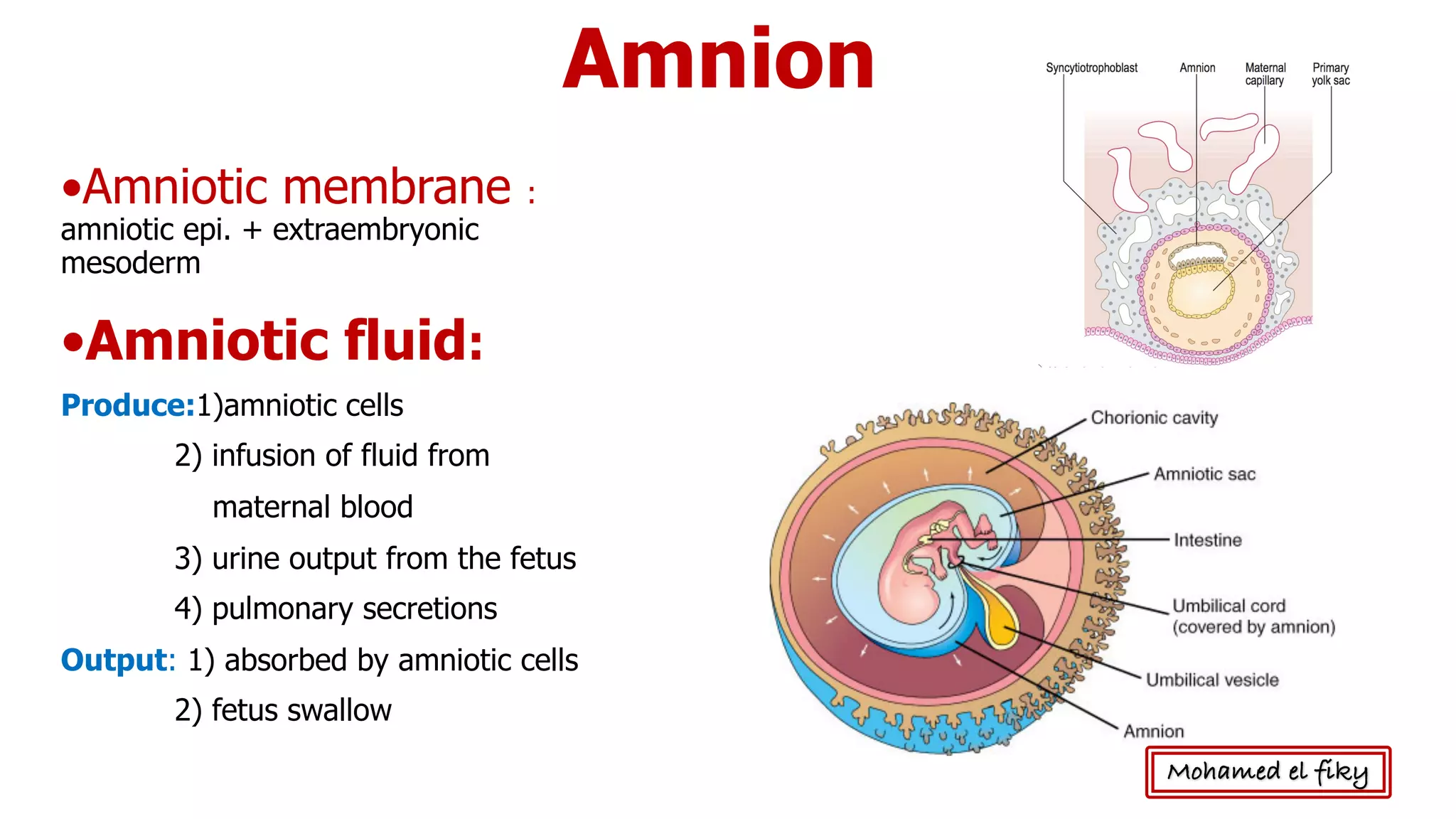
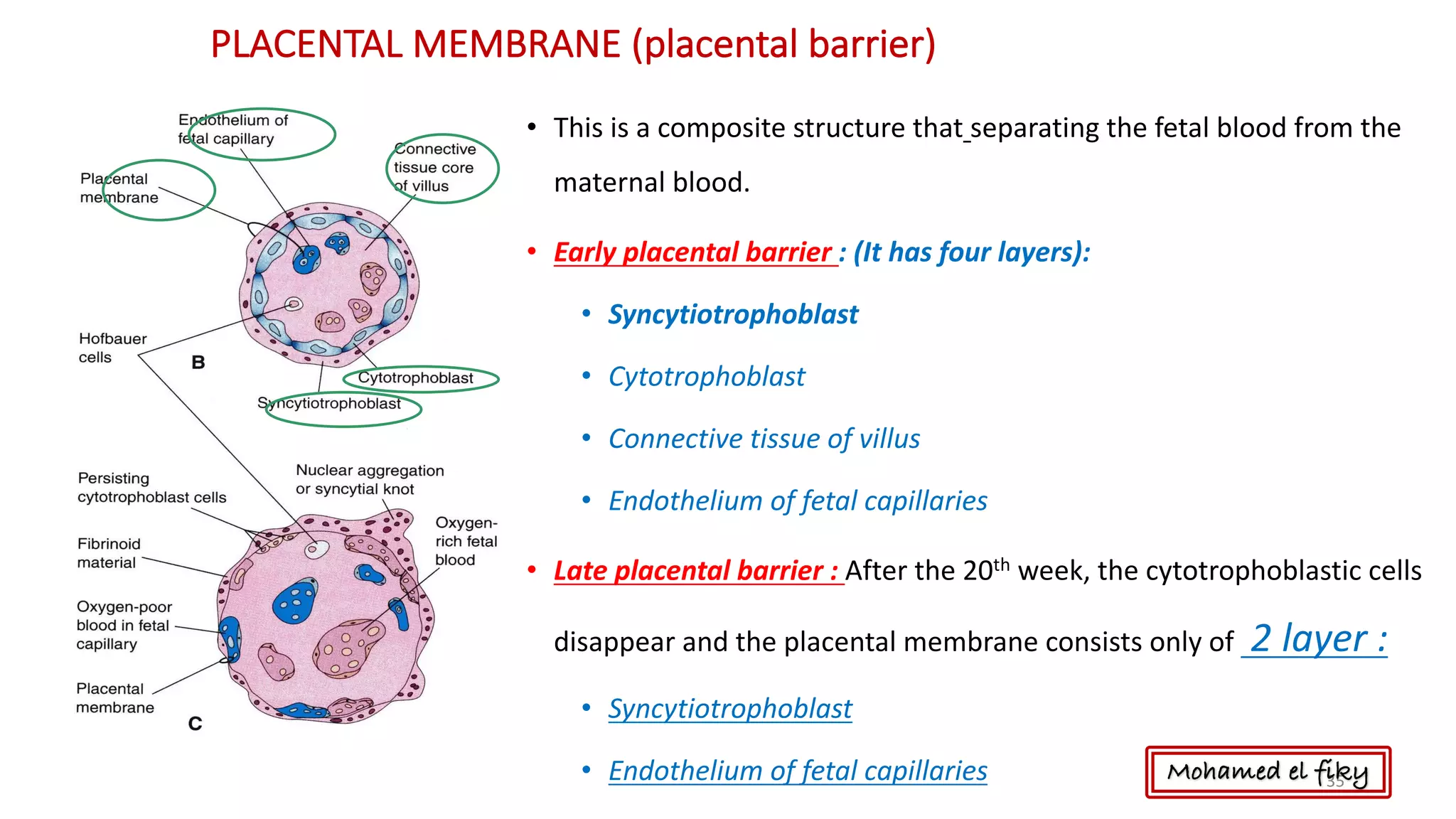
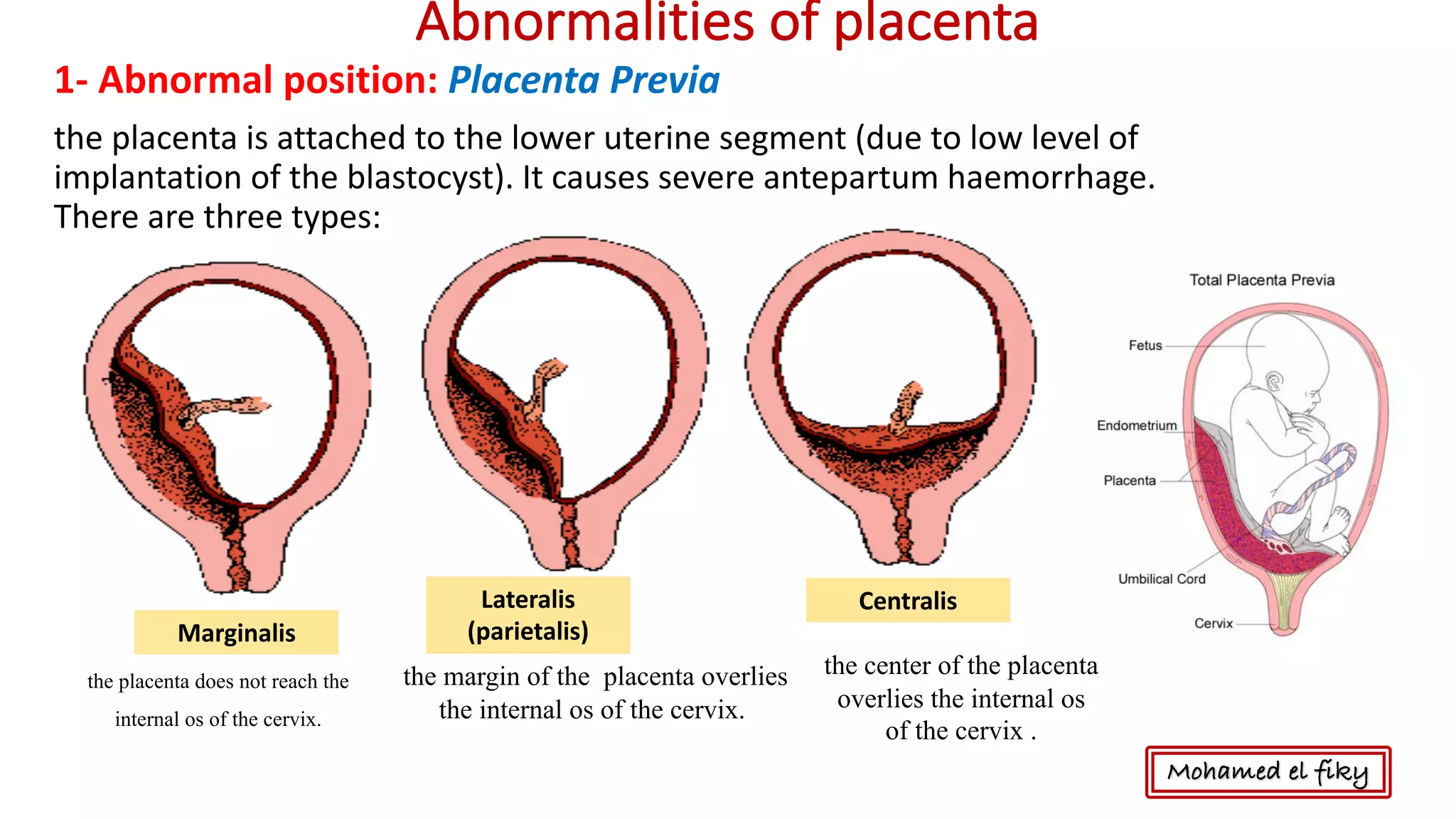
The document discusses fetal membranes including the amnion, chorion, yolk sac, allantois, and umbilical cord. It describes their development, structure, and functions. The amniotic fluid is mainly composed of water and plays various roles in fetal growth. The chorion develops from the trophoblast and contains villi that contribute to placental formation. The placenta forms from the chorionic villi and decidua basalis and functions to exchange gases, nutrients, and waste between the maternal and fetal blood without mixing.