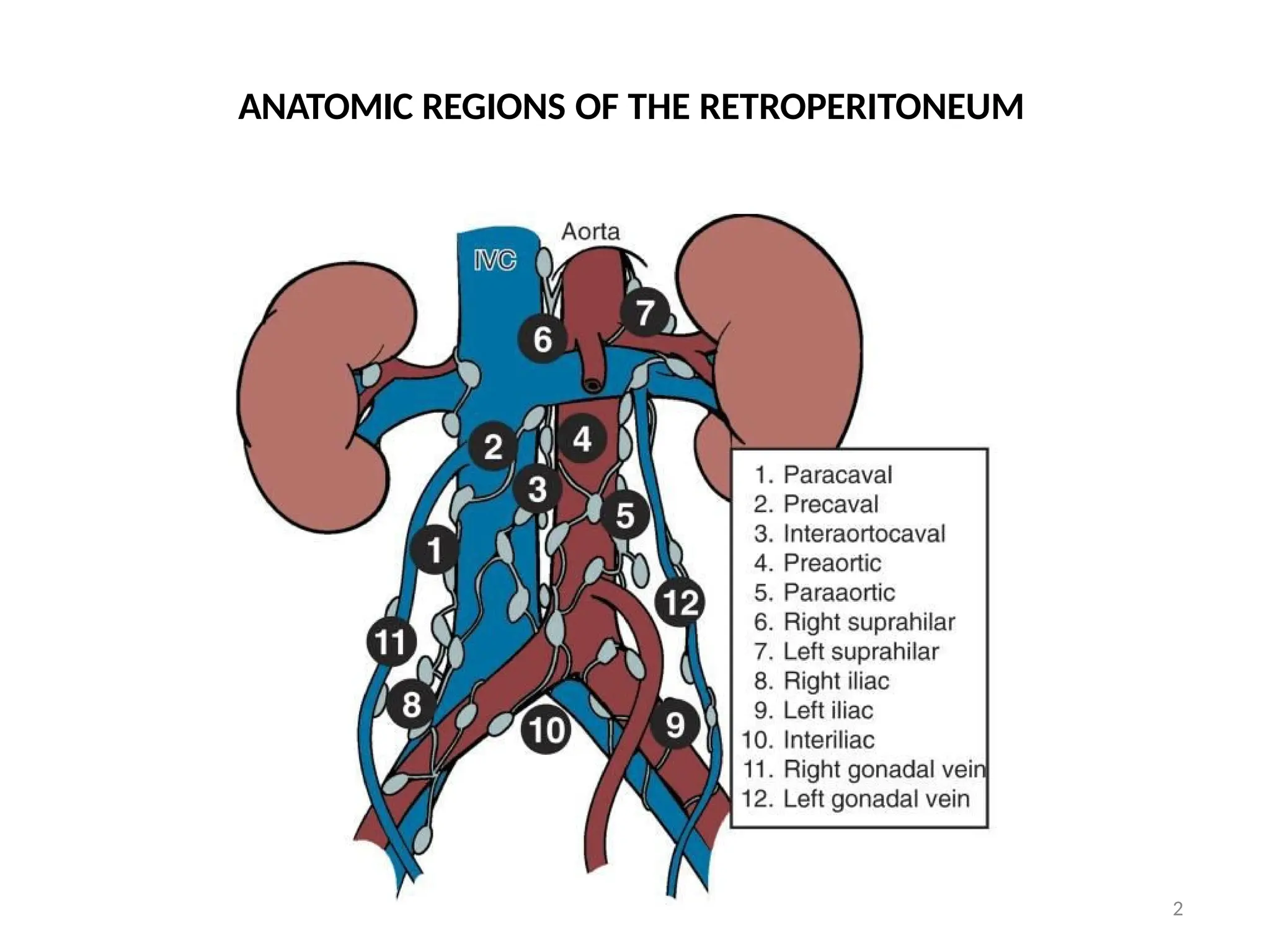
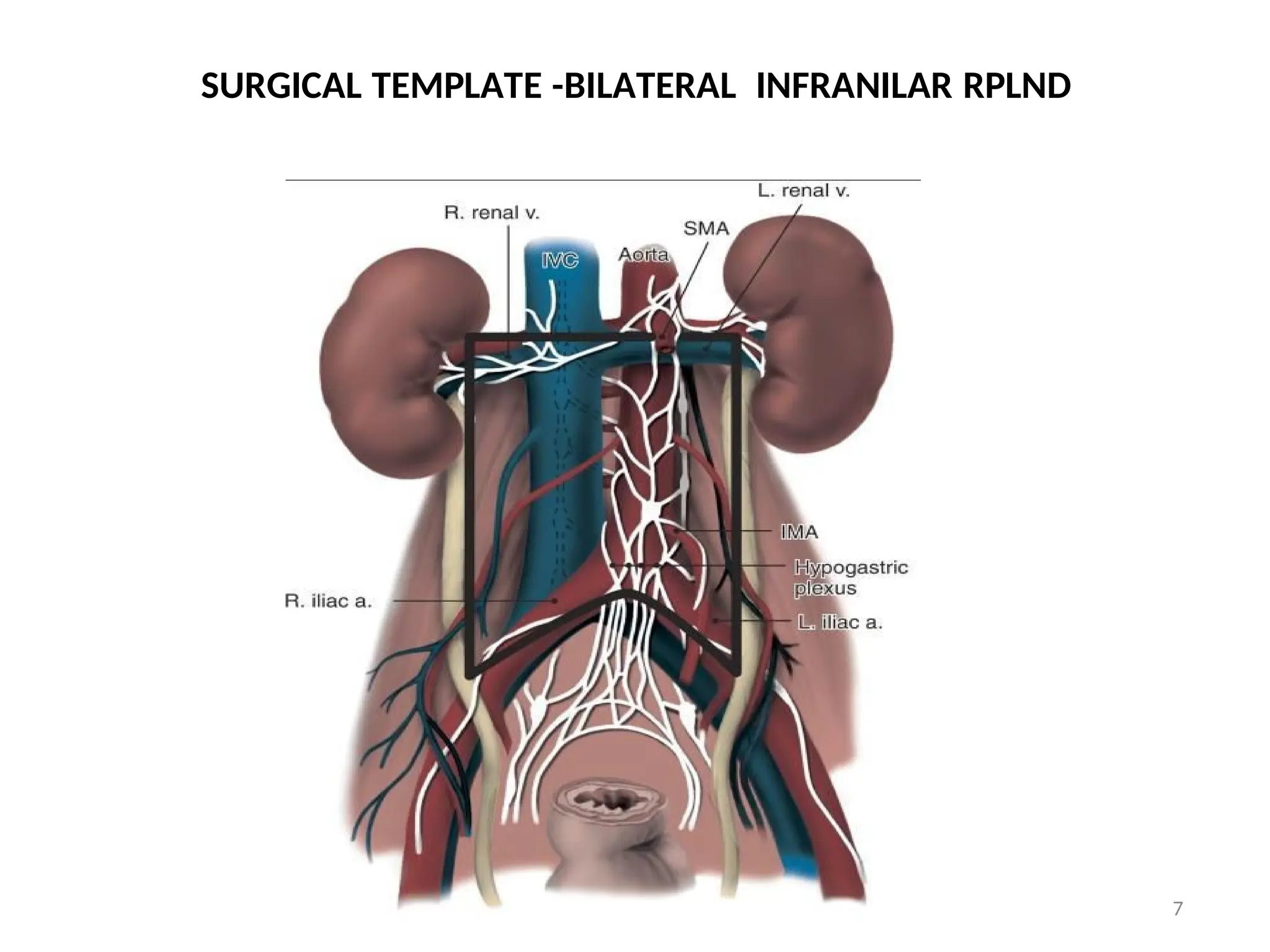
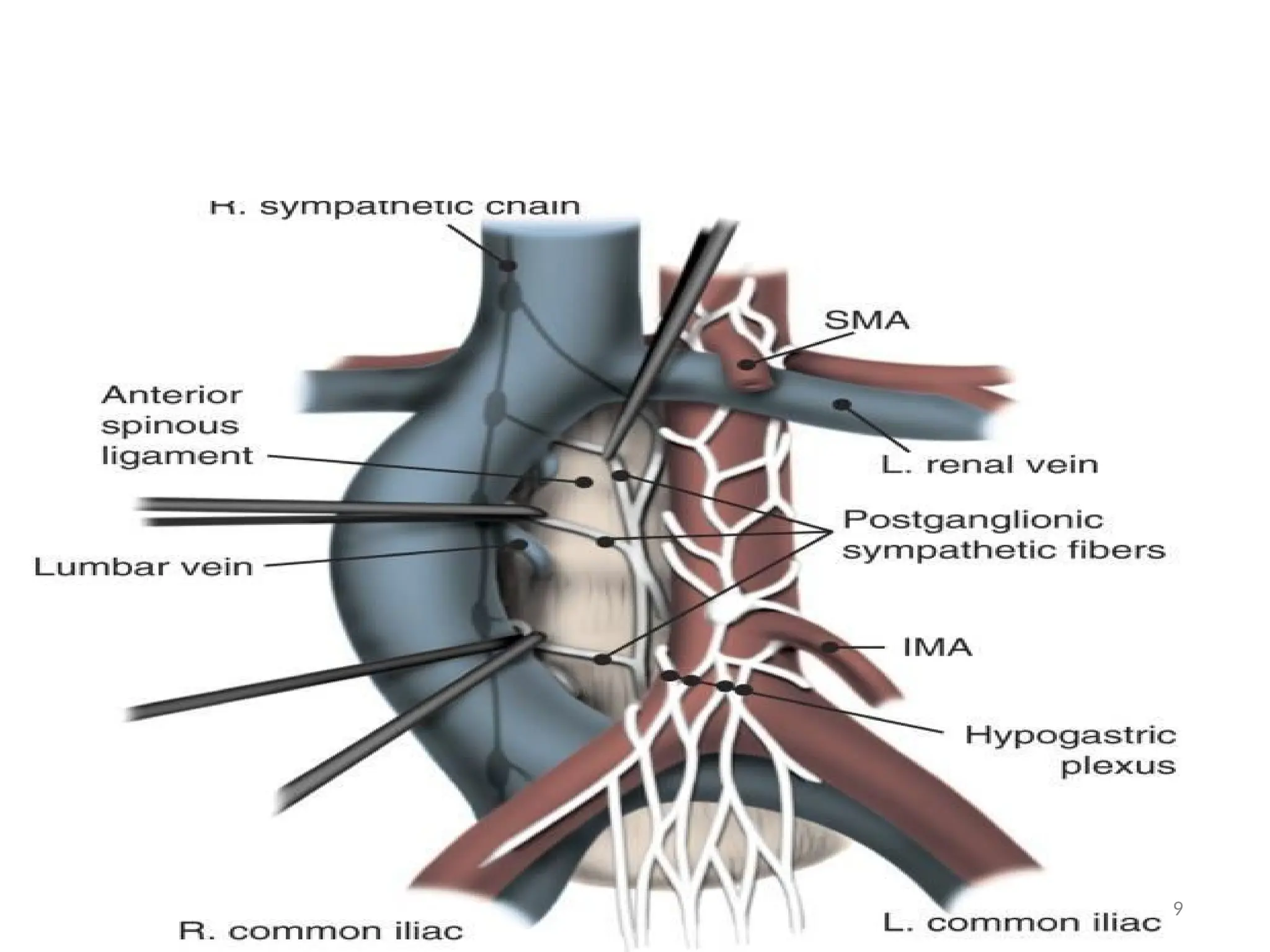
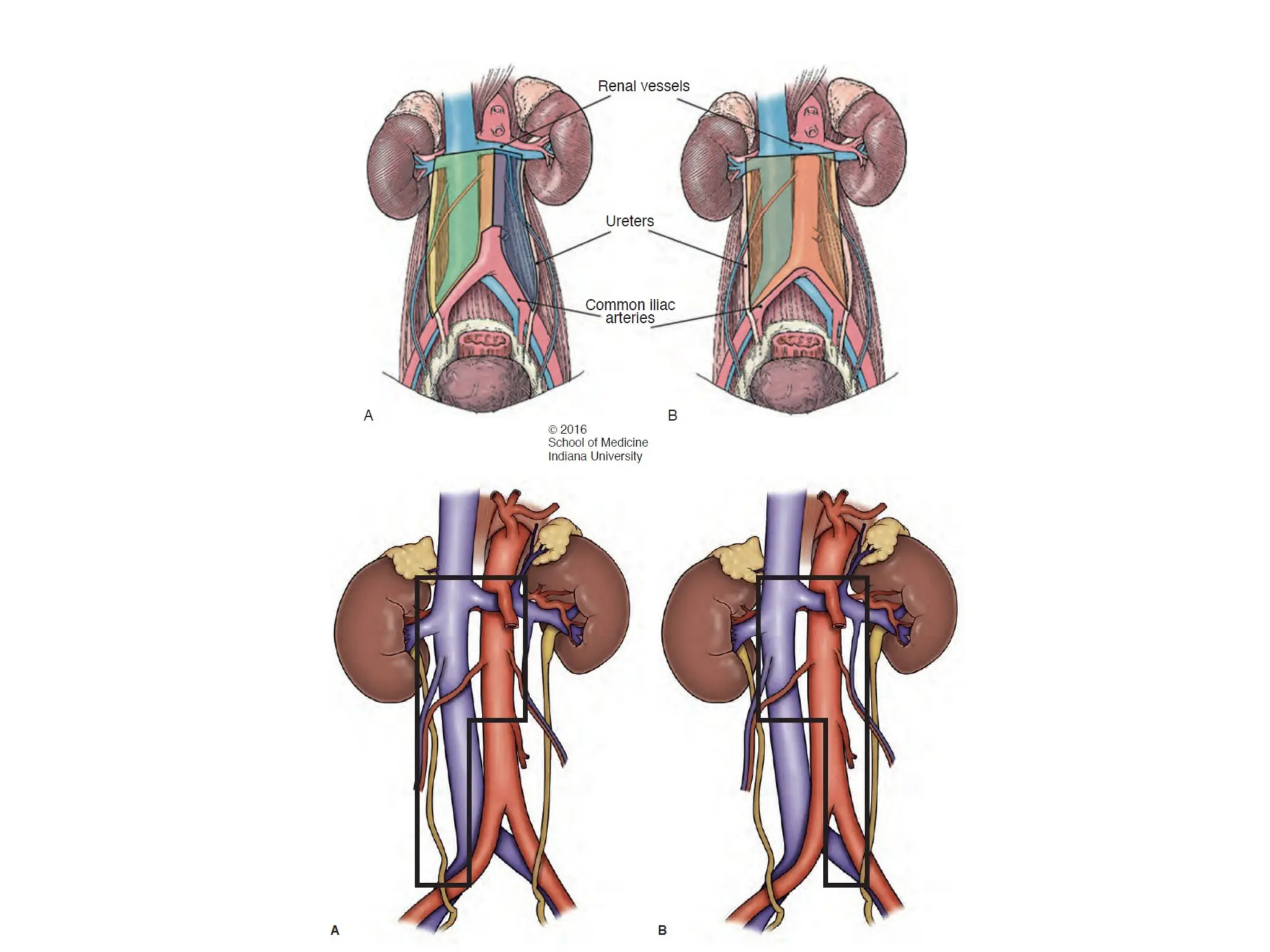
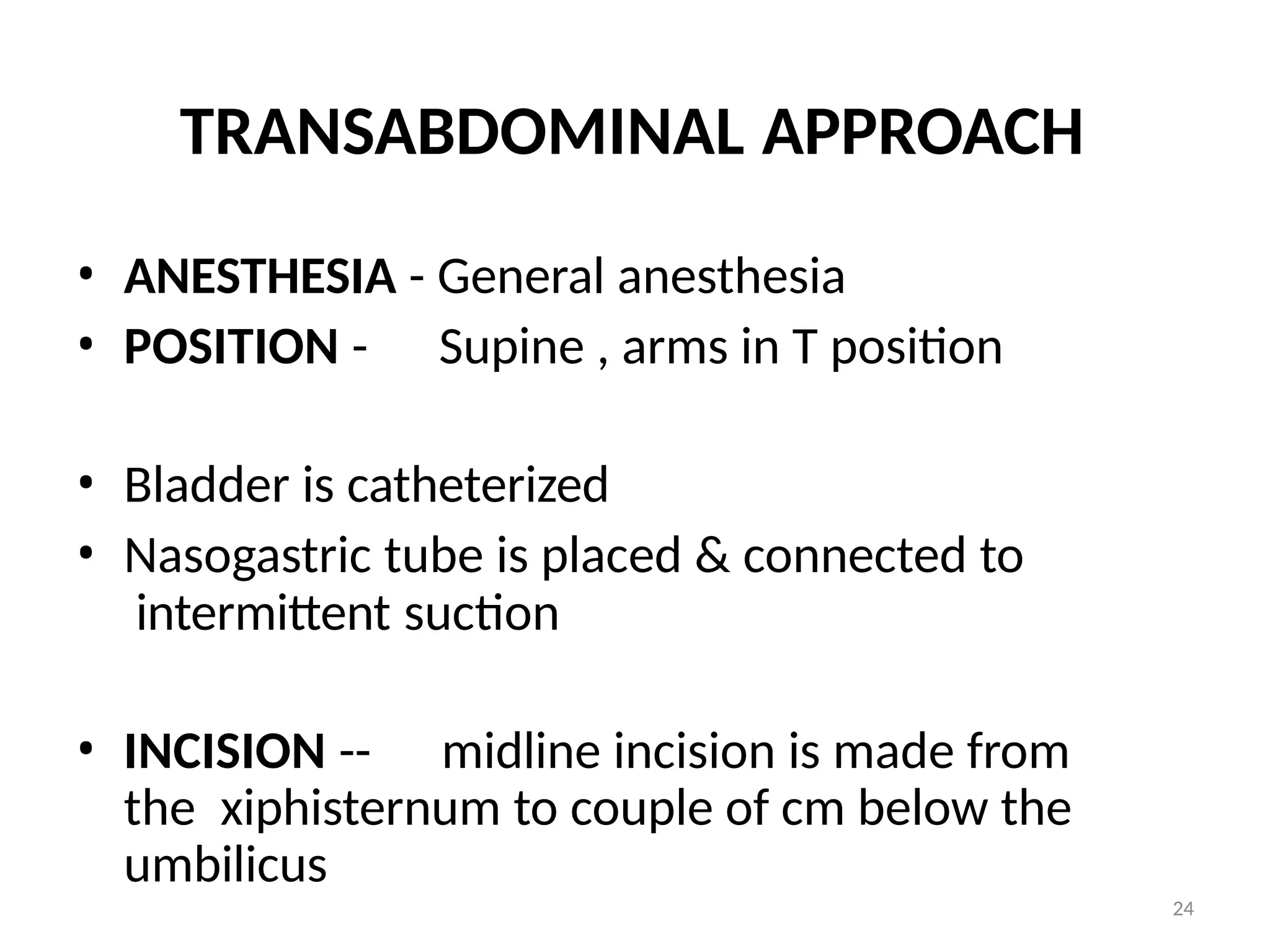
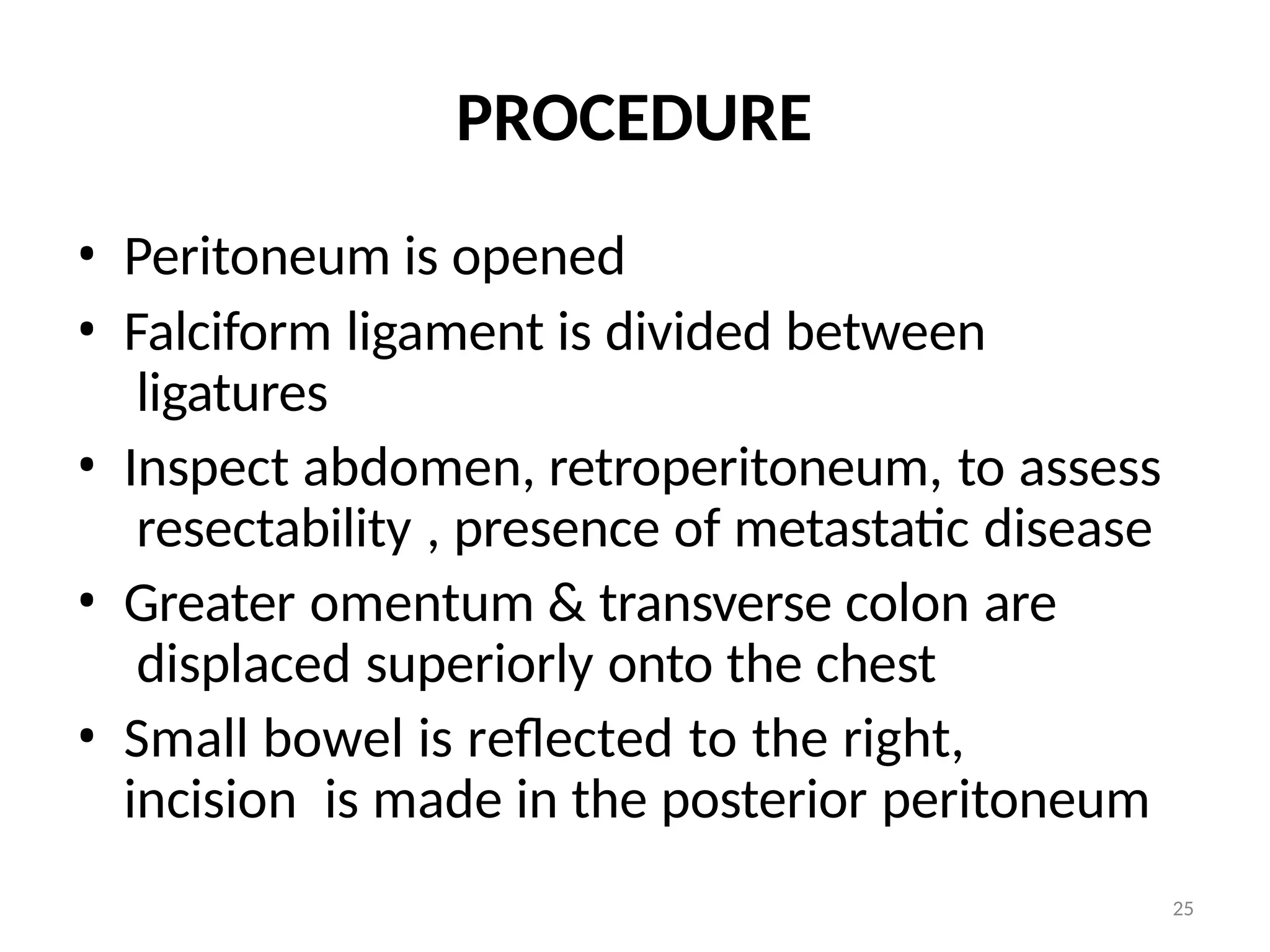
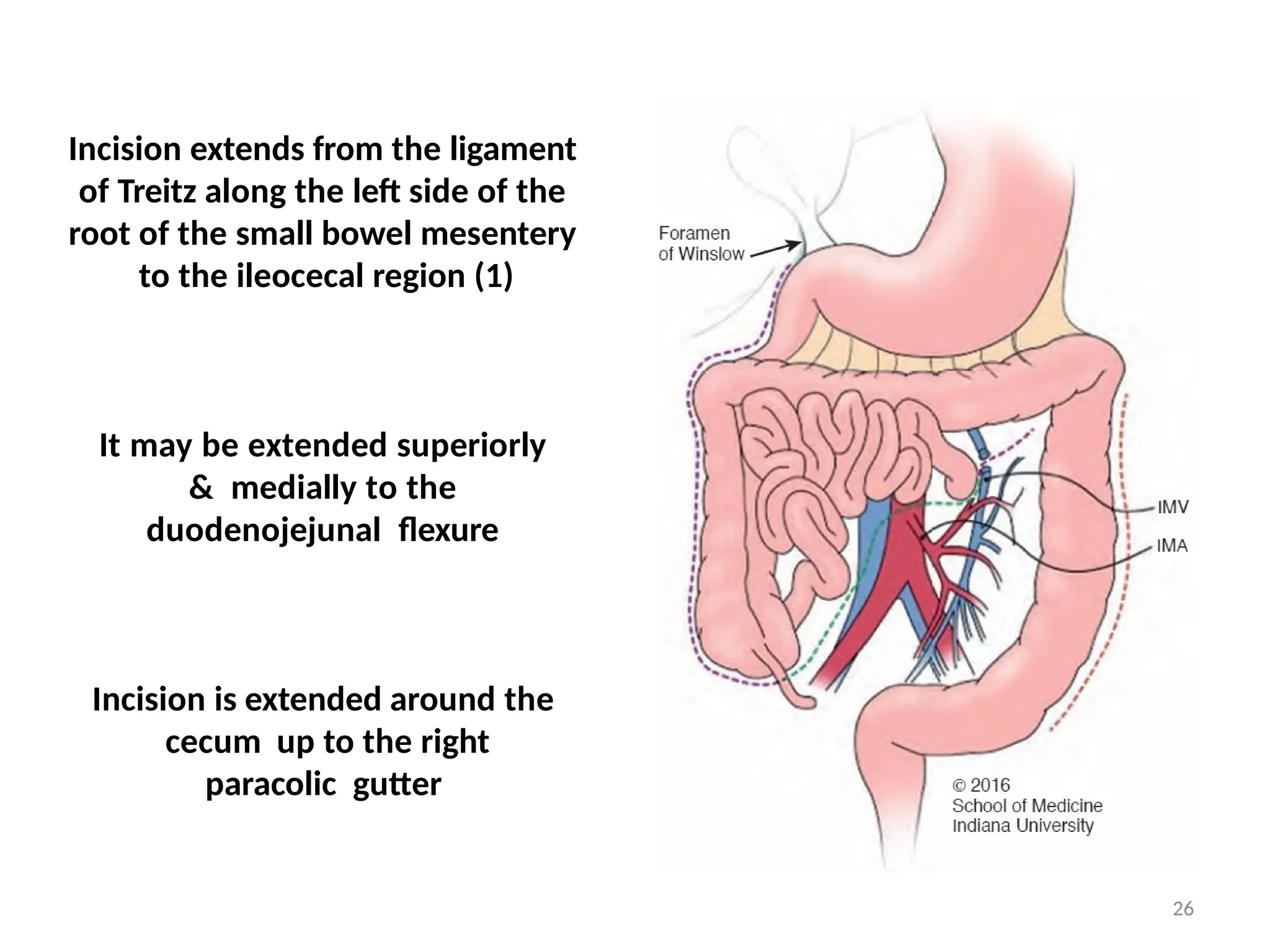
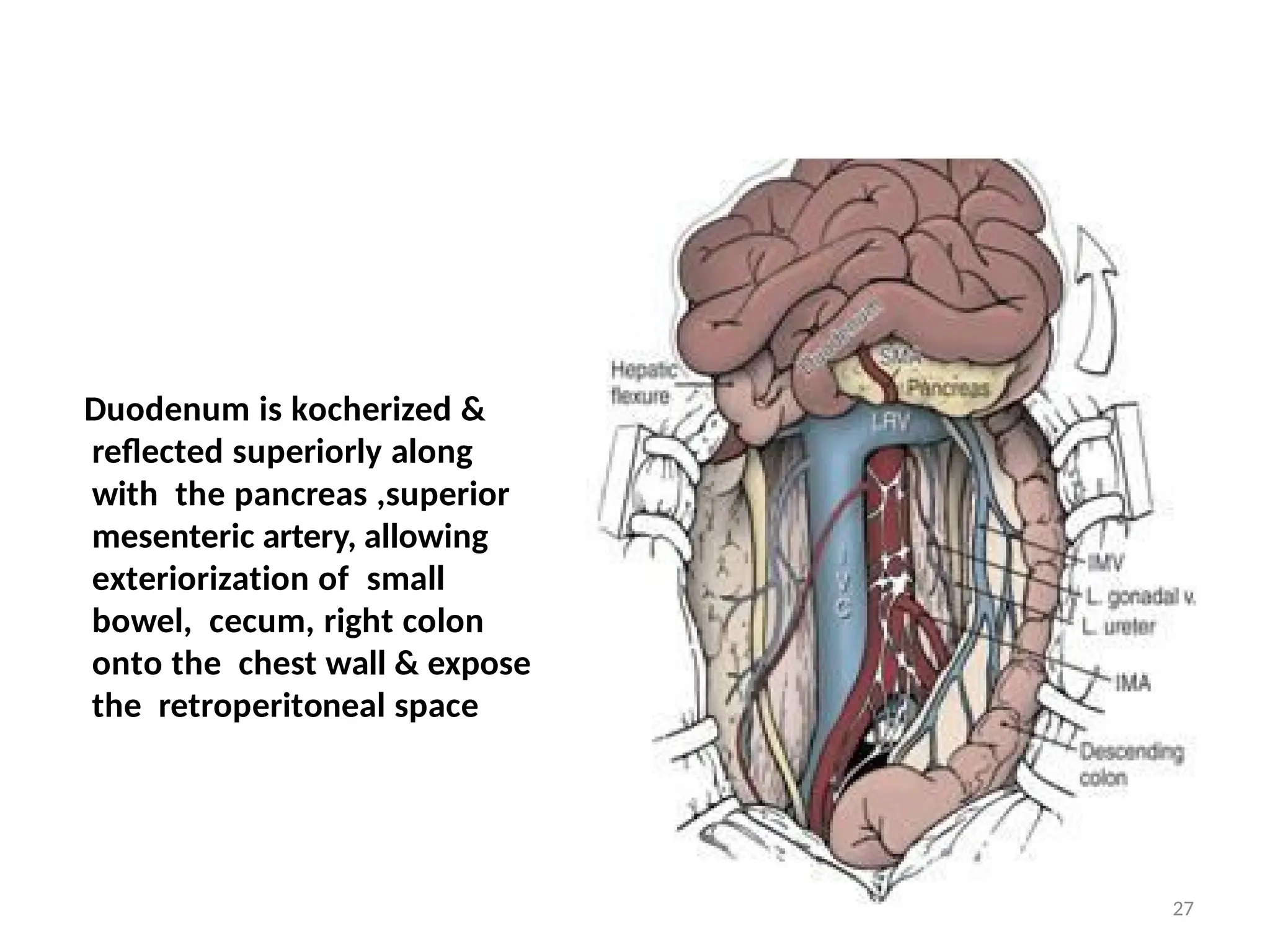
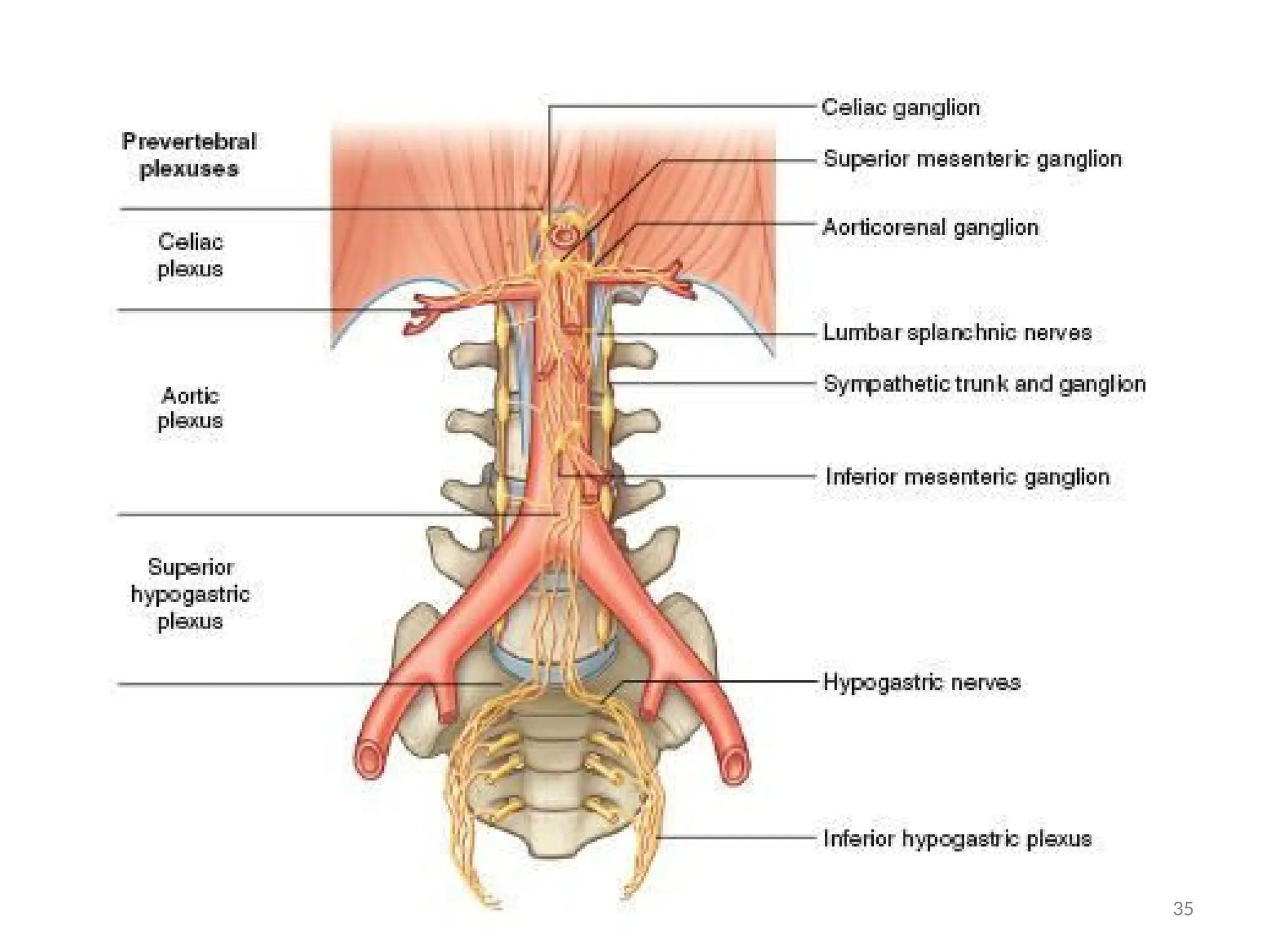
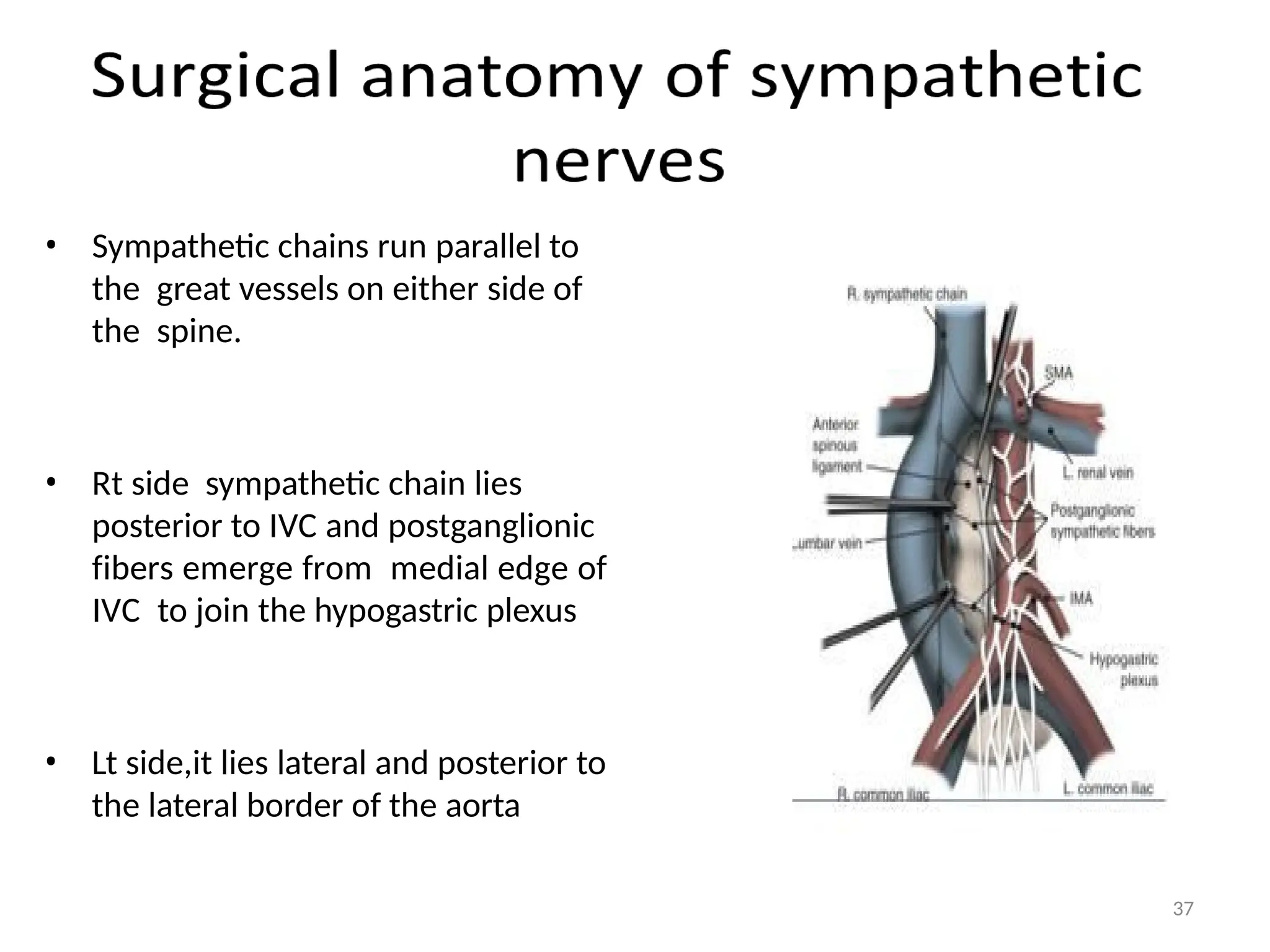
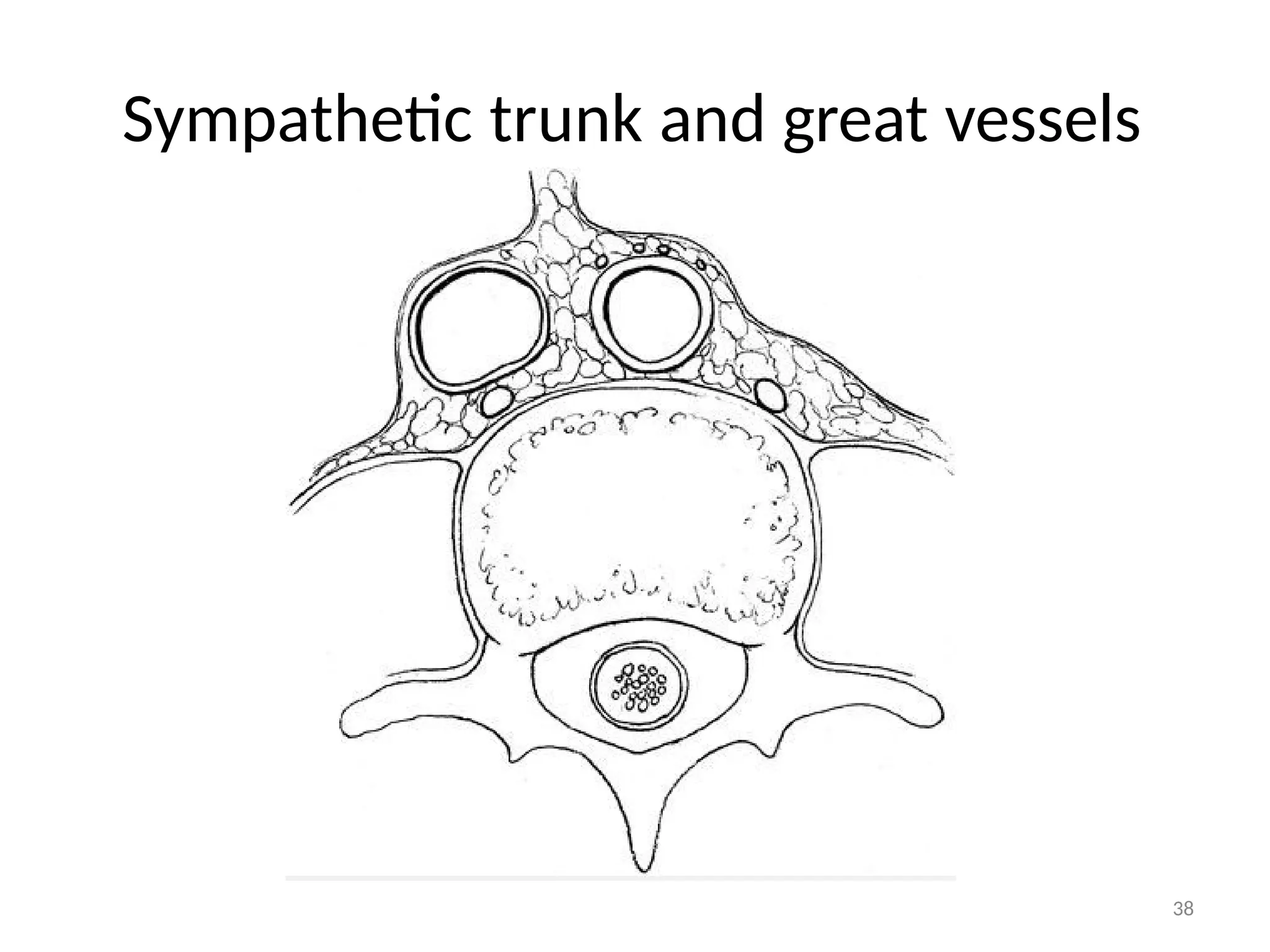
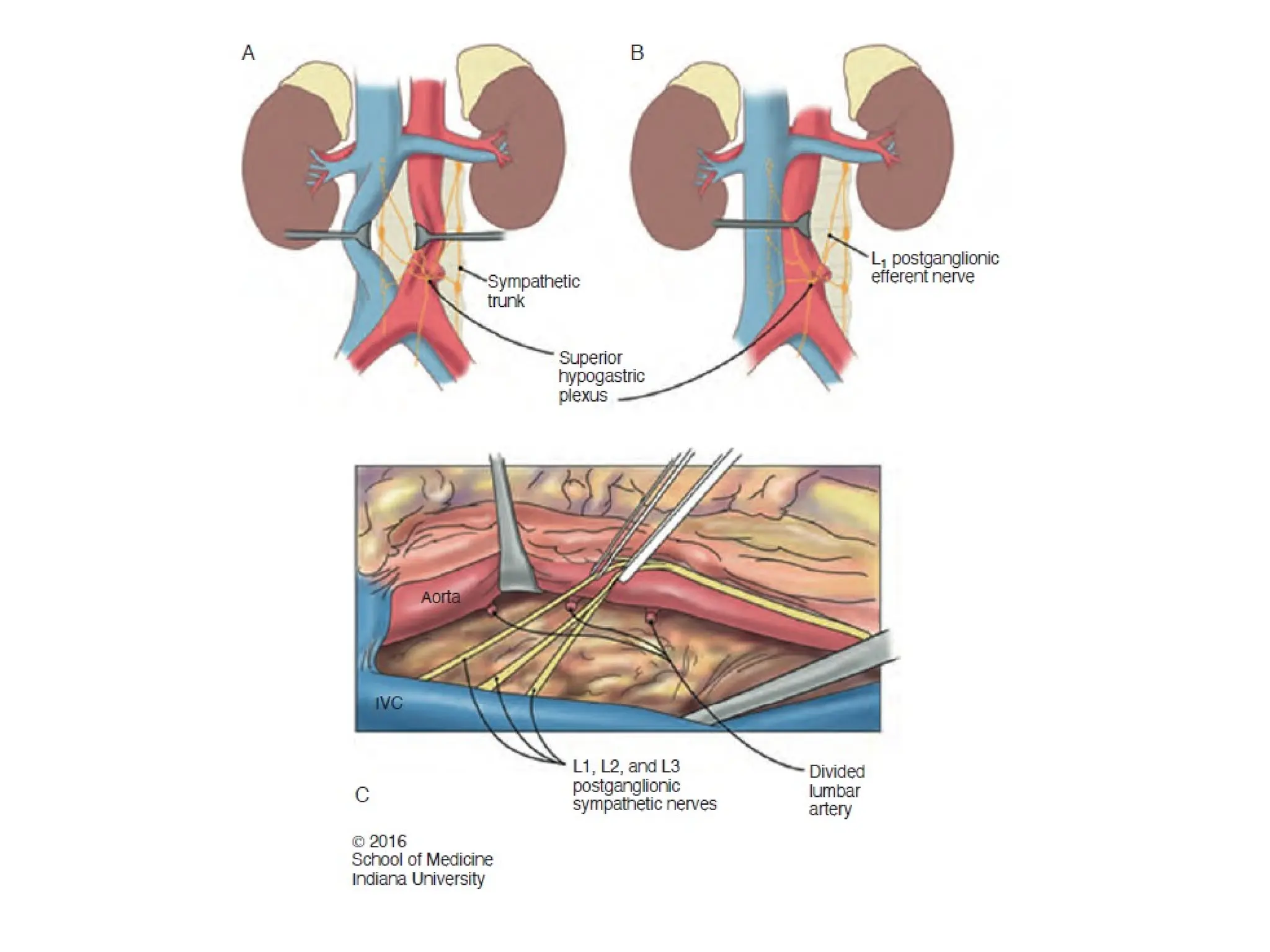
The document discusses retroperitoneal lymph node dissection (RPLND) techniques, focusing on surgical templates, rationale for treatment, and indications for different stages of non-seminomatous germ cell tumors (NSGCT). It emphasizes the importance of preserving sympathetic nerves to minimize ejaculatory dysfunction while ensuring complete lymph node removal for accurate staging and potential therapeutic benefits. Additionally, the document outlines complications associated with RPLND and the significance of modified techniques to improve patient outcomes.
![48
• Postoperative paternity can be expected in
approximately 75% of men undergoing
primary nerve-sparing RPLND.
• Fertility after PC-RPLND -not been established
[chemotherapy-induced disruption of
spermatogenesis can persist for several years
after completion of therapy].](https://image.slidesharecdn.com/rplndvenkateshenp-241006070214-1eabafee/75/RETRO-PERITONEAL-LYMPHNODE-DISSECTION-CA-48-2048.jpg)