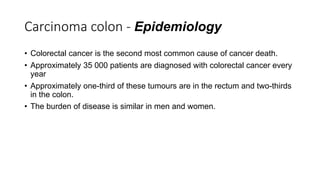
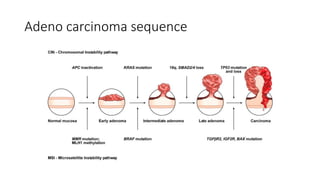
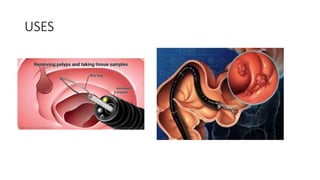
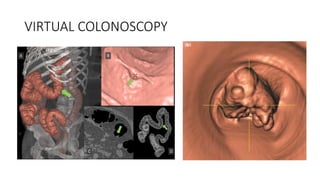
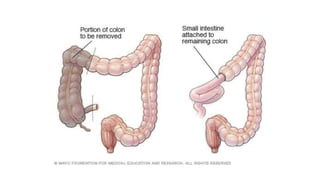
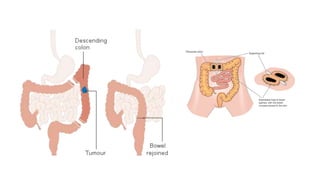
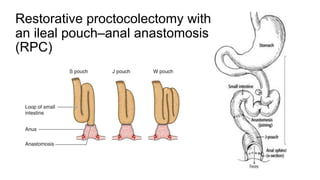
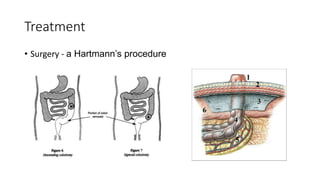
The document provides an overview of colorectal cancer, detailing its types, risks, and treatment options, including familial adenomatous polyposis (FAP) and hereditary non-polyposis colorectal cancer (Lynch syndrome). It emphasizes the importance of surgical interventions to prevent cancer development, diagnosis through genetic criteria, and the necessity of regular surveillance in high-risk patients. Additionally, it discusses the epidemiology of colorectal cancer, the various diagnostic methods, and considerations for managing metastatic disease.