Embed presentation
Download to read offline
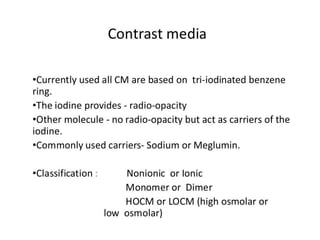
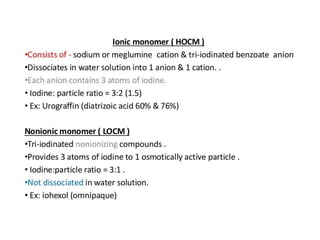
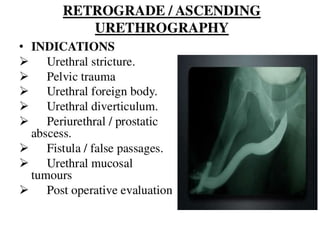
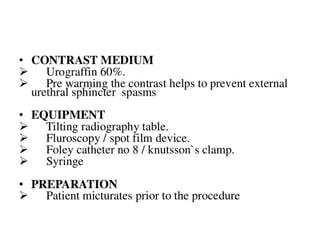

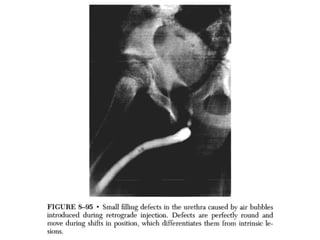
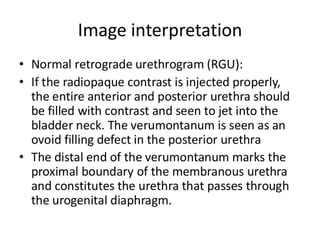
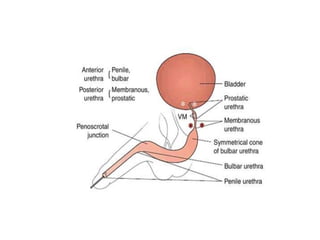
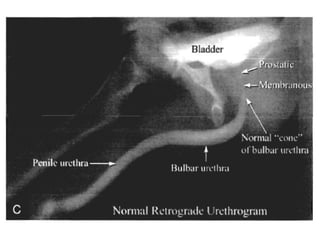
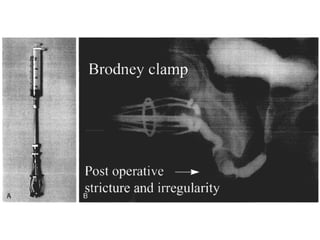
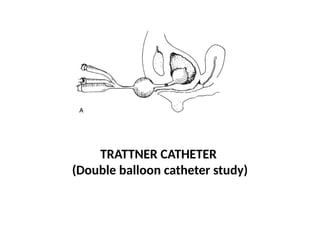
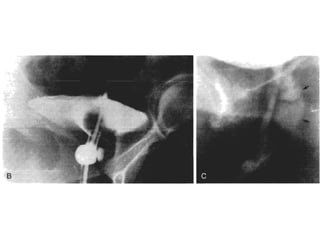
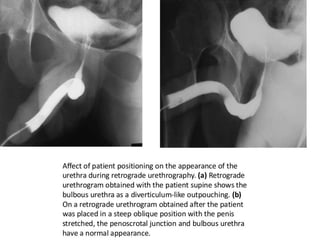
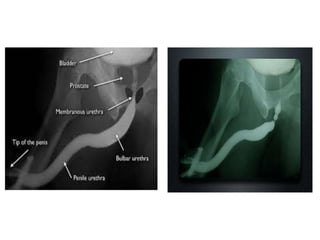
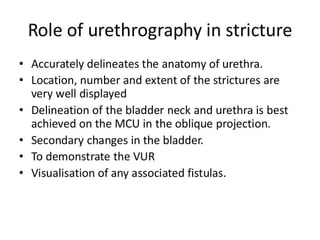

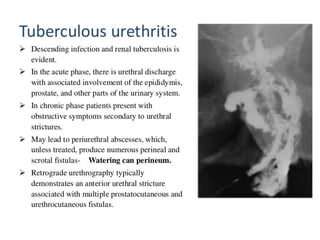
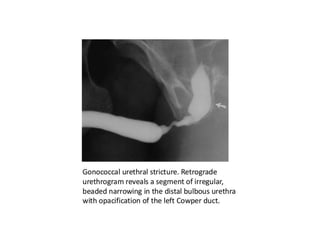
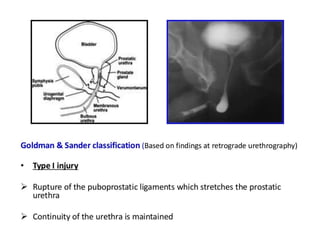
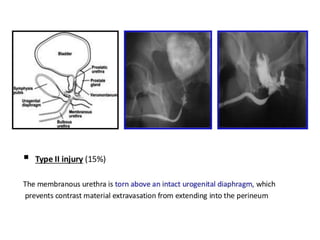
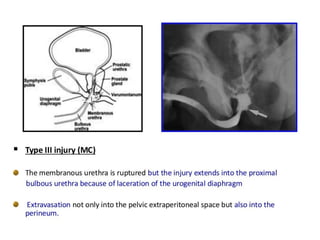
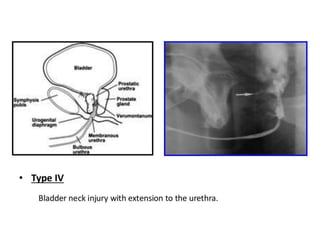
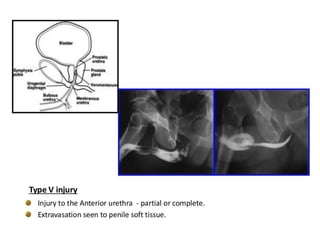
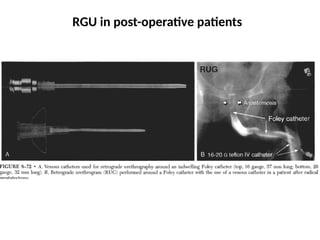
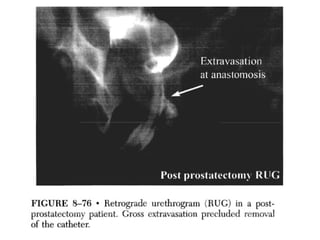
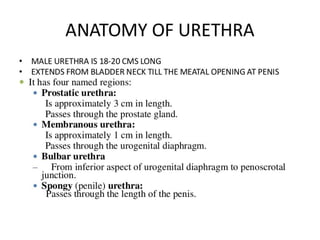
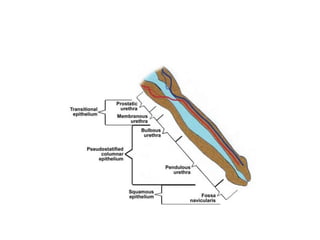
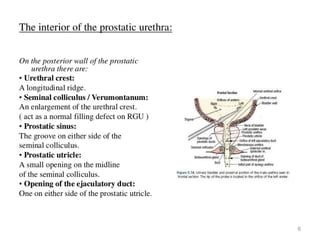
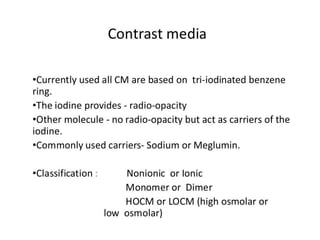
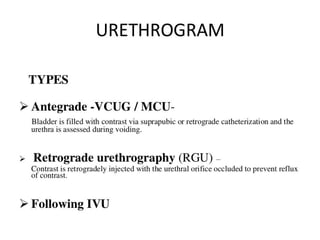
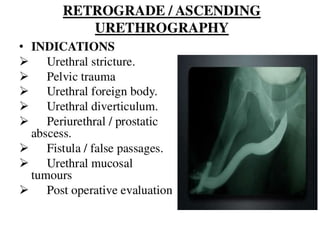
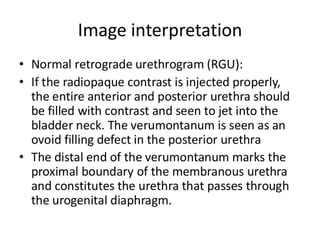
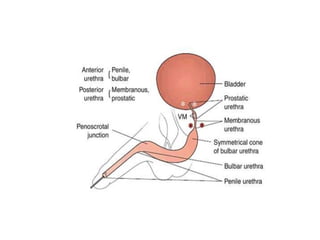
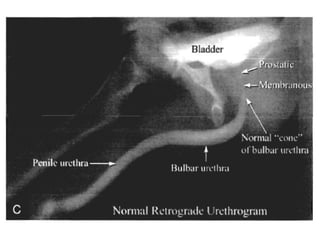
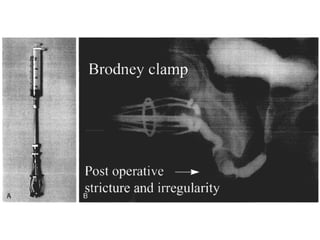
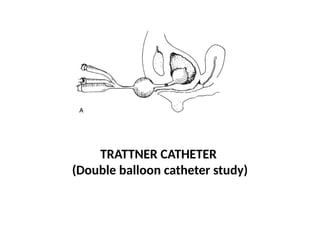
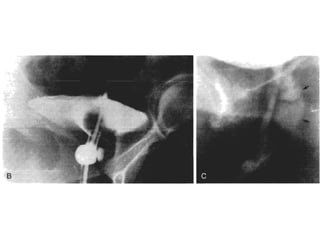
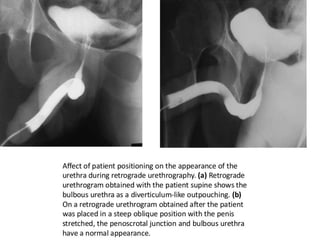
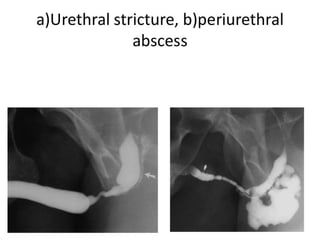
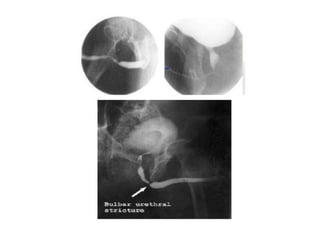
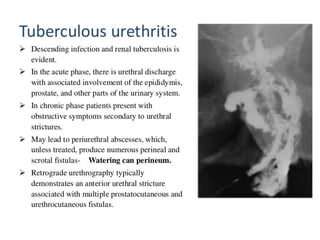
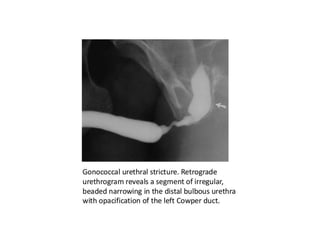
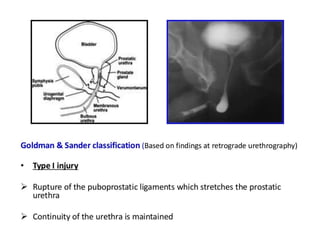
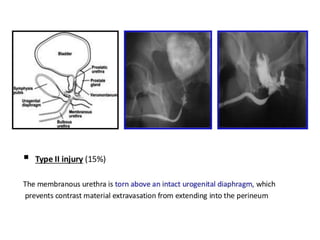
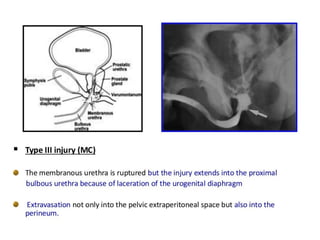
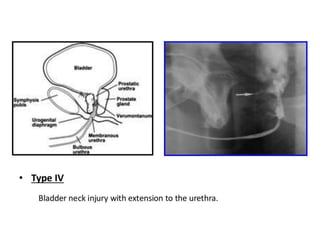
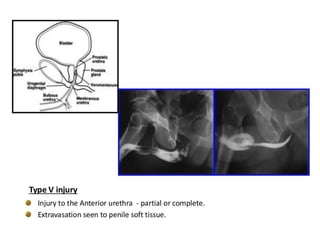
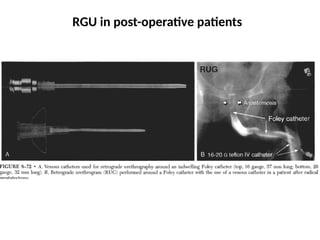
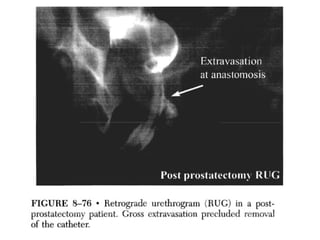
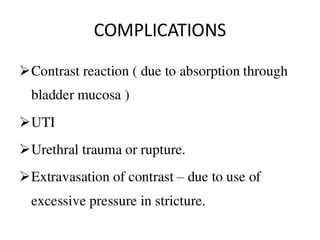
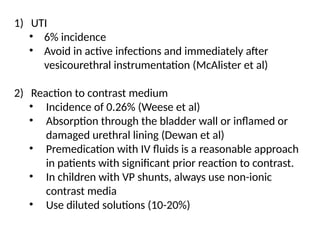
This document discusses the considerations and precautions for retrograde urethrography (RGU), noting that local anesthetic may cause issues such as mucosal edema. It highlights the need for antibiotic coverage due to potential complications like extravasation during contrast injection, and touches upon the role of cystography in pelvic fractures, indicating it can often be safely omitted. Additionally, it reports on complications related to urinary tract infections and reactions to contrast media, offering recommendations for patient management.