The document provides information on examining the respiratory system, including:
- Key anatomical structures of the chest and how to locate findings
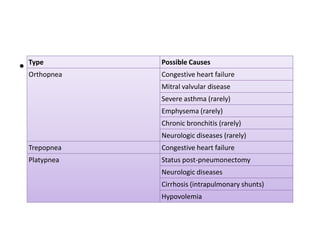
- Main symptoms to ask about including cough, dyspnea, hemoptysis, and wheezing
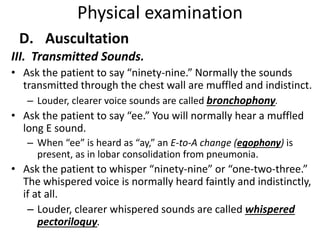
- How to perform a physical exam of the chest including inspection, palpation, percussion, and auscultation
- What different lung sounds and abnormalities indicate