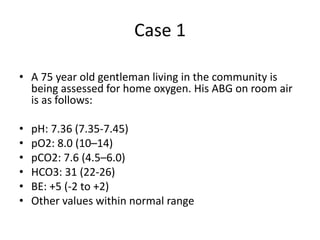
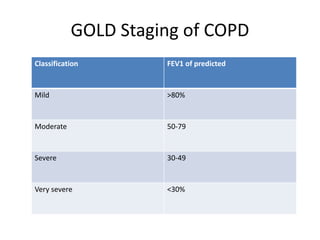
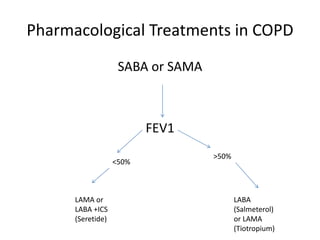
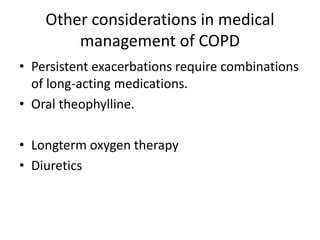
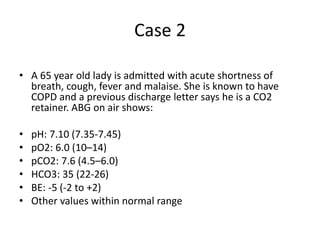
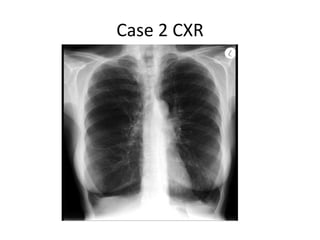
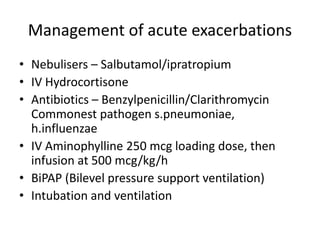
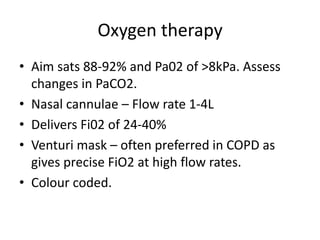
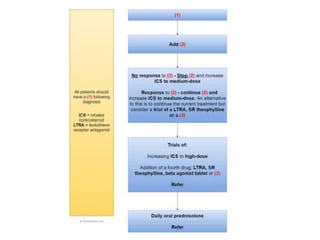
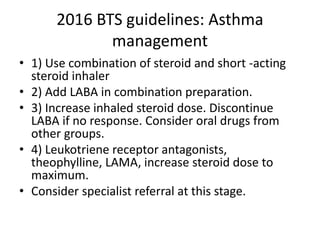
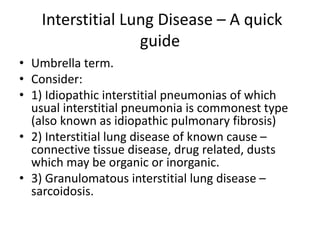
The document presents case studies of patients with respiratory conditions, focusing on COPD and asthma management. It details diagnostic features, pharmacological treatments, and management approaches for acute exacerbations, including oxygen therapy and invasive interventions. Additionally, it highlights classifications such as GOLD staging for COPD and emphasizes the importance of monitoring blood gas values in patients.