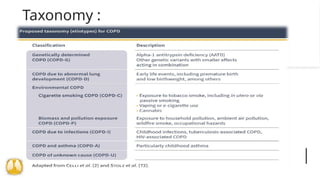
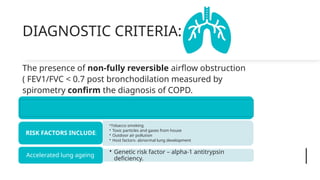
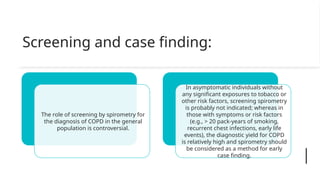
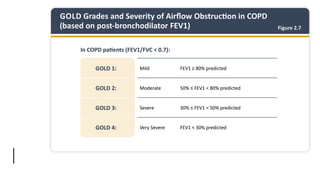
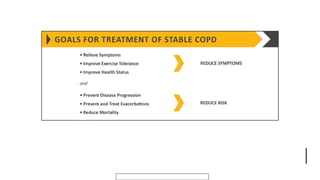
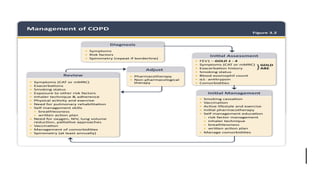
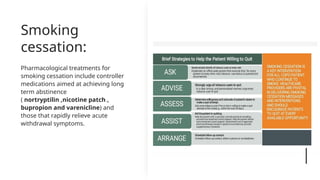
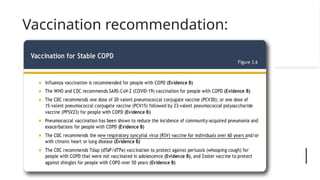
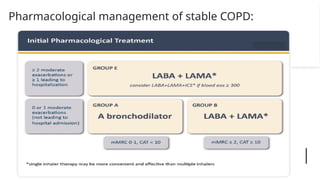
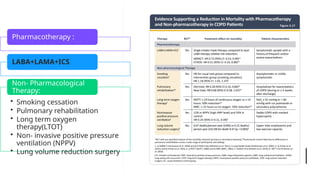
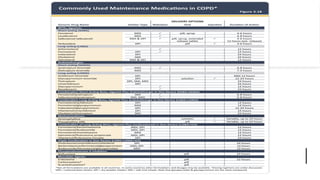
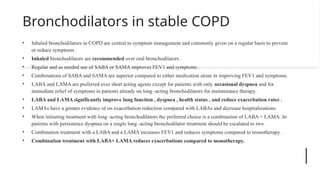
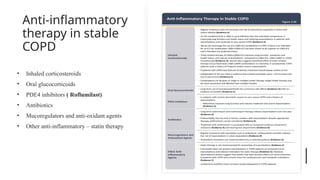
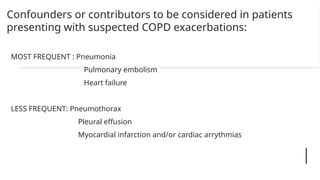
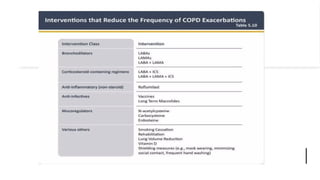
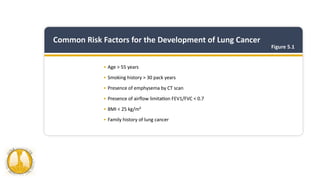
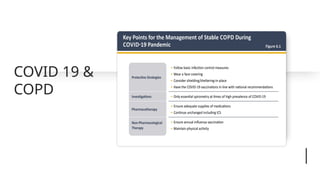
Chronic obstructive pulmonary disease (COPD) is a progressive lung condition characterized by airflow obstruction due to various factors, primarily tobacco smoking and environmental exposures. Diagnosis and management involve the use of spirometry for assessment and various treatments including smoking cessation, pharmacological therapies, and non-pharmacological interventions such as pulmonary rehabilitation. Early diagnosis and a comprehensive understanding of risk factors can significantly improve public health outcomes for individuals with COPD.