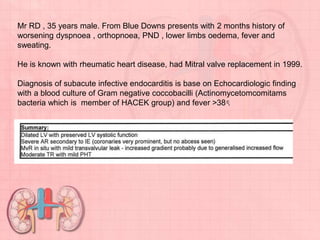
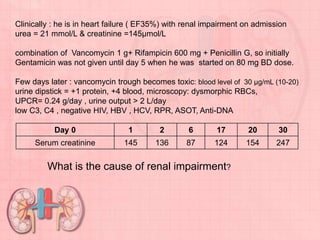
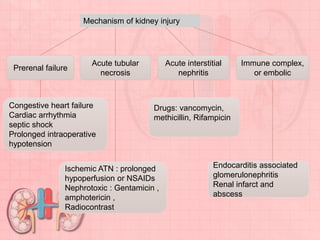
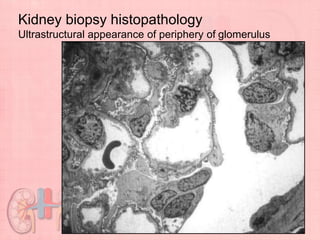
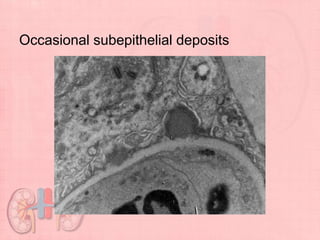
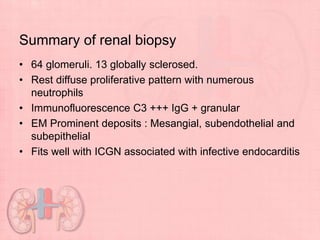
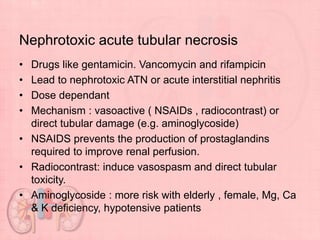
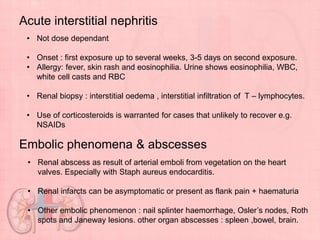
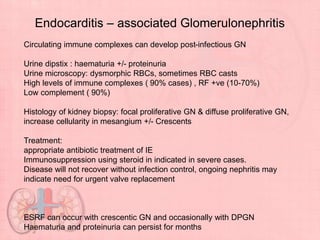
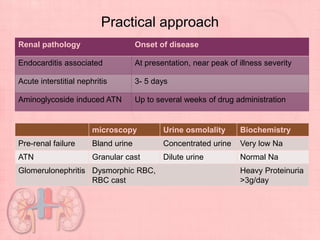
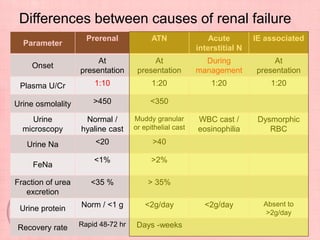
The document discusses a 35-year-old male with worsening respiratory symptoms and renal impairment, diagnosed with subacute infective endocarditis. It outlines kidney injury mechanisms, including nephrotoxic acute tubular necrosis and acute interstitial nephritis due to medication, particularly highlighting emergencies such as renal abscesses and glomerulonephritis associated with endocarditis. It emphasizes the need for appropriate antibiotic treatment and potential immunosuppression to manage the infection and its renal complications.