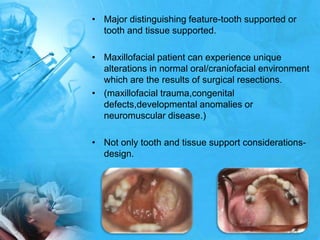
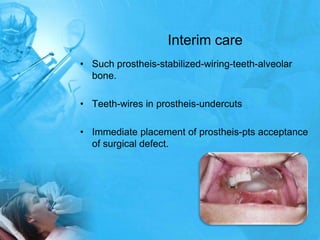
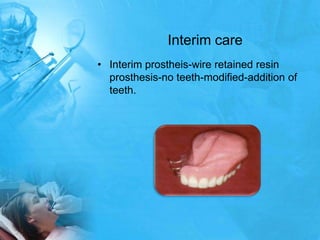
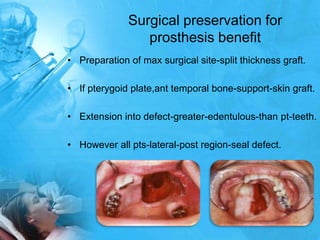
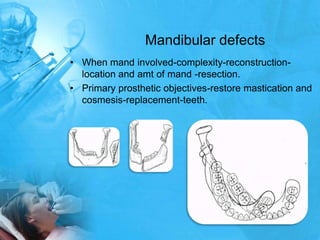
Removal partial denture considerations in maxillofacial prosthetics discusses interim, definitive, and surgical considerations for prosthetics following maxillofacial defects. Interim prosthetics aim to separate oral and nasal cavities and improve swallowing/speech. Definitive prosthetics restore function after tissue healing. Surgical preservation of teeth and tissues benefits prosthetics by providing support and retention. Mandibular reconstruction challenges include soft tissue bulk and bone placement impacting function.